Vitamin D and Diabetes: Sunshine Nutrient for Insulin Sensitivity
Deficiency in the “sunshine vitamin” is widespread—and research shows it may directly impact blood sugar control. Explore how vitamin D links to type 2 diabetes, the best ways to boost your levels, and what the science actually says about supplementation.
For a full framework on diet, supplements, and lifestyle, see our Ultimate Guide to Natural Diabetes Support.
The Overlooked Problem of Vitamin D Deficiency in Diabetes
More than one billion people worldwide are estimated to have inadequate vitamin D levels, according to the Mayo Clinic. Among individuals with type 2 diabetes, rates of deficiency run even higher. Why? Lower sun exposure, higher body mass index, darker skin tone, and certain medications all contribute. The CDC notes that most Americans fail to meet recommended intakes from food alone.
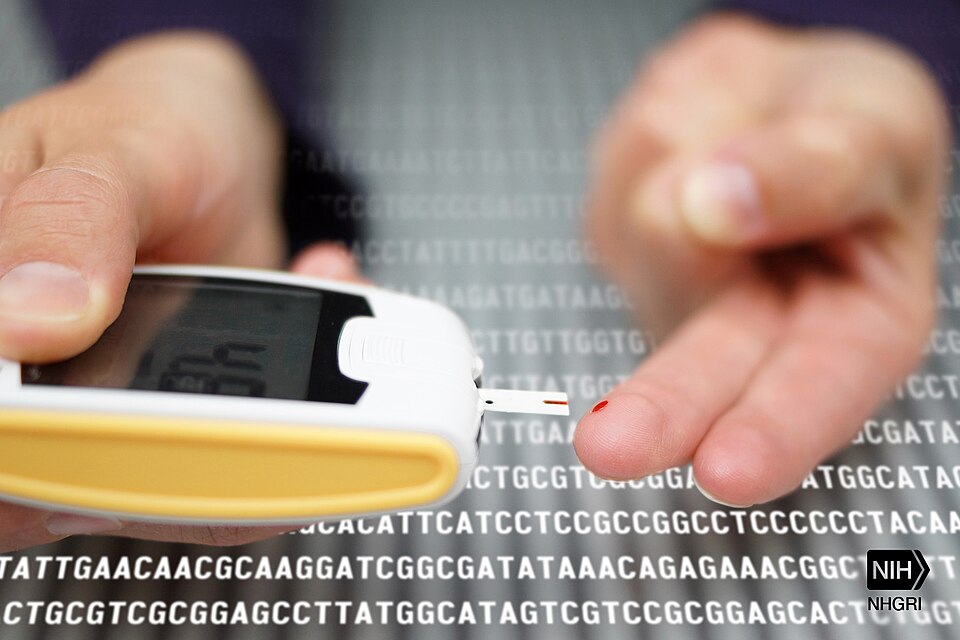
For people living with diabetes, this deficiency matters. Research shows vitamin D receptors exist in pancreatic beta cells and muscle tissue—two sites critical to blood sugar regulation. When vitamin D status is low, both insulin secretion and glucose uptake are compromised.
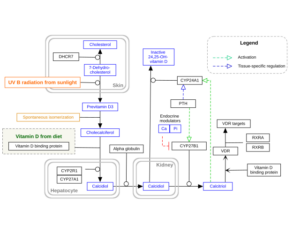
How Vitamin D Influences Insulin Sensitivity

“Vitamin D receptors in pancreatic β-cells and muscle tissue play roles in insulin secretion and glucose uptake.” Insulin secretion: Vitamin D binds to receptors in pancreatic beta cells, supporting normal insulin release after meals. Deficiency may blunt this process, worsening post-meal blood sugar spikes.
- Muscle glucose uptake: By activating genes related to insulin receptors in muscle, vitamin D improves the body’s ability to move glucose out of the bloodstream and into cells for energy.
- Inflammation control: Low vitamin D is associated with higher inflammatory markers, which drive insulin resistance. Correcting deficiency may lower systemic inflammation.
What Clinical Studies Show About Vitamin D and Diabetes

Evidence has been mixed but generally points toward benefit—especially in those who start with low levels. A 2018 meta-analysis found that vitamin D supplementation modestly improved fasting glucose and insulin sensitivity in people with type 2 diabetes and prediabetes. The Harvard T.H. Chan School of Public Health emphasizes that while vitamin D is not a cure, maintaining adequate levels supports overall metabolic health.
- Prevention data: Large cohort studies suggest people with sufficient vitamin D are at lower risk of developing type 2 diabetes compared to those deficient.
- Intervention trials: Supplementation (often 1000–2000 IU/day) shows modest improvements in insulin sensitivity and HbA1c, though results vary.
- Complications: Adequate vitamin D may reduce risk of diabetic neuropathy and cardiovascular disease, though more research is needed.
How to Get Enough Vitamin D

“Midday sun on skin for short durations remains the most natural way to maintain healthy vitamin D status.” Sunlight: Exposing face, arms, and legs to midday sun for 10–30 minutes a few times per week can provide meaningful amounts. Geographic latitude, skin tone, and sunscreen use all influence synthesis.

“Fatty fish and egg yolks provide natural vitamin D, complementing safe sun exposure.” Food sources: Fatty fish like salmon, sardines, and mackerel are top natural sources. Egg yolks and fortified foods (milk, cereals) contribute additional amounts. According to the NHS, it’s nearly impossible to meet needs through food alone in winter months.
- Supplements: Vitamin D3 (cholecalciferol) is better absorbed than D2. Typical doses range from 600–2000 IU daily, though some people require higher amounts to reach optimal blood levels (20–50 ng/mL).
Safety and Potential Risks
Vitamin D toxicity is rare but possible with excessive supplementation. Symptoms of dangerously high levels include nausea, weakness, and elevated calcium levels (hypercalcemia). People with chronic kidney disease or certain granulomatous conditions should use supplements only under medical supervision. Always check with your healthcare provider before starting high-dose vitamin D.
Vitamin D Compared to Other Nutrients in Diabetes
| Nutrient | Role in Diabetes | Evidence Strength | Notes |
|---|---|---|---|
| Vitamin D | Insulin secretion, glucose uptake, inflammation control | Moderate evidence; strongest in deficiency correction | Safe at 600–2000 IU/day for most adults |
| Magnesium | Insulin signaling and glucose transport | Robust evidence for insulin sensitivity support | See our magnesium article |
| Alpha-Lipoic Acid (ALA) | Antioxidant; helps diabetic neuropathy | Moderate evidence from clinical trials | Read about ALA |
FAQs
Can vitamin D prevent type 2 diabetes?
Studies suggest that adequate vitamin D reduces risk, but supplementation alone is not a guaranteed prevention method. It works best alongside healthy diet and lifestyle changes.
Does vitamin D lower blood sugar?
Some studies show modest reductions in fasting glucose and HbA1c, especially in those who are deficient. The effect is supportive, not curative.
Which form is best: D2 or D3?
Vitamin D3 (cholecalciferol) is better absorbed and maintains blood levels more effectively than D2 (ergocalciferol).
How much vitamin D should people with diabetes take?
Typical daily intakes range from 600–2000 IU, though individual needs vary. Blood testing is the best way to personalize dosage.
Can you get enough vitamin D from the sun alone?
It depends on location, skin tone, and lifestyle. In northern latitudes during winter, supplementation is often necessary.
Conclusion
Vitamin D deficiency is common—and correcting it can support insulin sensitivity, glucose regulation, and overall health. While it’s not a cure for diabetes, maintaining optimal levels through safe sun exposure, nutrient-rich foods, and well-dosed supplementation provides meaningful benefits. Work with your healthcare provider to monitor levels and integrate vitamin D into a broader, balanced diabetes support plan.
References
Author Bio
The Remedy Verified Team is dedicated to exploring natural, research-backed approaches to chronic health conditions. Our writers translate complex scientific studies into clear, practical insights to help readers make informed decisions about their health. About the Author
Disclaimer
The information provided in this article is for educational purposes only and is not intended as medical advice. Always consult your healthcare provider before making changes to your supplements, diet, or medications—especially if you have type 2 diabetes or are at risk of deficiency.