Understanding triglycerides normal values and LDL cholesterol ranges represents a fundamental aspect of cardiovascular risk assessment. Furthermore, these lipid measurements serve as critical indicators for predicting atherosclerotic cardiovascular disease development. Additionally, current evidence demonstrates that optimal lipid management extends far beyond traditional cholesterol monitoring approaches.
Modern lipid science reveals complex interactions between triglycerides and cholesterol metabolism. Moreover, recent clinical trials highlight the importance of achieving lower triglyceride targets than previously recommended. Consequently, healthcare providers increasingly recognize that standard cholesterol management may leave substantial residual cardiovascular risk unaddressed.
Understanding Triglycerides Normal Values: Clinical Significance and Risk Stratification

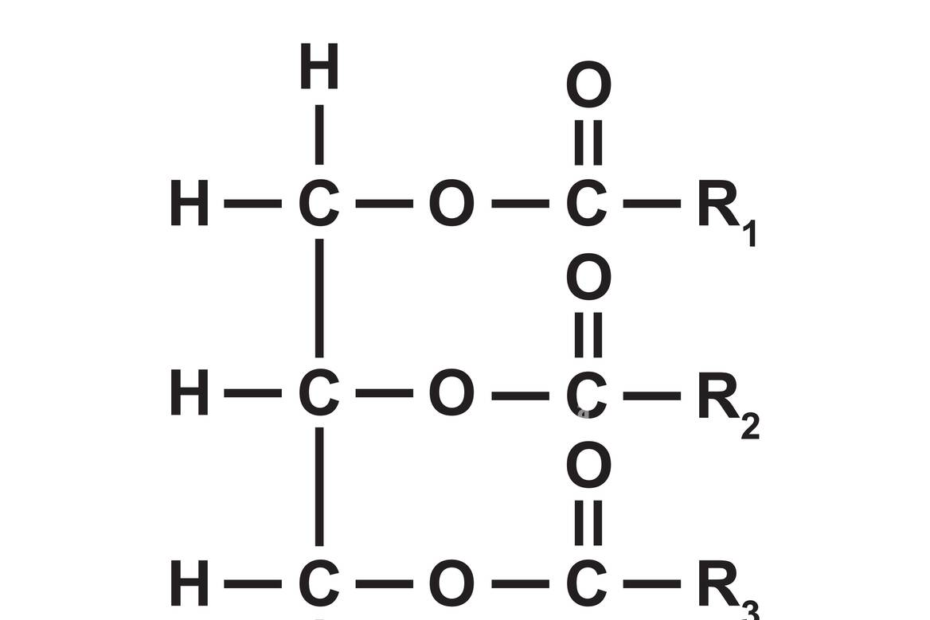
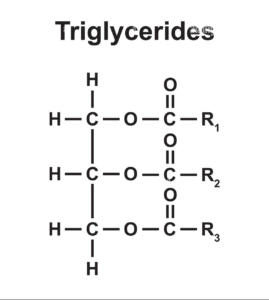
Triglycerides represent the most abundant fat molecules in human circulation. Specifically, these lipid compounds serve essential functions in energy storage and cellular metabolism. Nevertheless, elevated triglyceride concentrations significantly increase cardiovascular disease risk independent of cholesterol levels.
⏳ Triglyceride Risk Classification System
The National Heart, Lung, and Blood Institute establishes these classification ranges based on extensive population studies. However, emerging evidence from the REDUCE-IT trial suggests cardiovascular benefits occur when triglycerides remain below 135 mg/dL in high-risk patients. Therefore, clinicians increasingly adopt more stringent triglyceride targets for optimal risk reduction.
Importantly, triglyceride metabolism differs significantly from cholesterol pathways. While cholesterol primarily originates from dietary sources and hepatic synthesis, triglycerides fluctuate dramatically based on recent food intake. Consequently, accurate triglyceride measurement requires fasting for 8-12 hours to eliminate postprandial elevation effects.
Advanced Triglyceride Physiology and Metabolic Interactions
Triglyceride synthesis occurs through multiple biochemical pathways involving glycerol and fatty acid esterification. Initially, dietary fats undergo intestinal absorption and packaging into chylomicrons. Subsequently, these large lipoprotein particles transport triglycerides to peripheral tissues for energy utilization or adipose storage.
The liver simultaneously produces very-low-density lipoproteins (VLDL) containing endogenously synthesized triglycerides. Furthermore, insulin resistance dramatically increases hepatic triglyceride production while decreasing peripheral clearance. This dual mechanism explains why diabetic patients frequently develop hypertriglyceridemia despite adequate glycemic control.
LDL Cholesterol Ranges: Evidence-Based Targets for Cardiovascular Protection
LDL cholesterol ranges provide crucial information for cardiovascular risk stratification and therapeutic decision-making. Notably, extensive clinical trial evidence demonstrates that lower LDL levels correlate with reduced atherosclerotic cardiovascular disease events. Additionally, recent guidelines emphasize aggressive LDL lowering in high-risk populations.
| Risk Category | LDL Target (mg/dL) | Clinical Considerations |
|---|---|---|
| General Population | <100 | Optimal for primary prevention |
| Established ASCVD | <70 | High-intensity statin therapy recommended |
| Very High Risk ASCVD | <55 | Consider non-statin add-on therapy |
| Extreme Risk | <40 | Multiple major ASCVD events |
The 2018 AHA/ACC cholesterol guidelines revolutionized LDL management by establishing specific numerical targets. Previously, guidelines focused on percentage LDL reduction rather than absolute values. However, accumulating evidence demonstrates that achieving specific LDL thresholds provides superior cardiovascular protection.
Mechanistically, LDL particles infiltrate arterial walls where they undergo oxidative modification. Subsequently, these modified LDL particles trigger inflammatory cascades leading to atherosclerotic plaque formation. Therefore, reducing LDL concentrations decreases the substrate available for atherogenesis.
Precision Medicine Approaches to LDL Optimization
Contemporary LDL management incorporates sophisticated risk assessment tools beyond traditional lipid panels. For instance, apolipoprotein B measurement provides superior cardiovascular risk prediction compared to calculated LDL cholesterol. Furthermore, Lp(a) testing identifies patients with inherited elevated cardiovascular risk requiring aggressive interventions.
Genetic factors significantly influence individual LDL cholesterol responses to dietary and pharmacological interventions. Specifically, polymorphisms in PCSK9, LDLR, and APOB genes affect cholesterol metabolism efficiency. Consequently, personalized medicine approaches increasingly guide optimal LDL management strategies.
Integrating Triglycerides and LDL: Comprehensive Lipid Risk Assessment
Modern cardiovascular risk assessment requires simultaneous evaluation of triglycerides normal values and LDL cholesterol ranges. Importantly, these lipid parameters interact synergistically to influence atherosclerotic disease progression. Additionally, patients frequently present with mixed dyslipidemia requiring multifaceted therapeutic approaches.
Non-HDL cholesterol calculation provides valuable insight into total atherogenic particle burden. This measurement includes LDL cholesterol plus VLDL cholesterol (primarily triglyceride-rich particles). Therefore, non-HDL cholesterol captures cardiovascular risk from both cholesterol and triglyceride pathways simultaneously.
Research demonstrates that patients with elevated triglycerides and optimal LDL cholesterol maintain increased cardiovascular risk. Furthermore, the REDUCE-IT trial showed significant cardiovascular benefit from triglyceride lowering despite adequate statin therapy. Consequently, addressing residual triglyceride-mediated risk becomes essential for comprehensive cardiovascular protection.
Advanced Lipid Testing: Beyond Standard Panels
Nuclear magnetic resonance (NMR) spectroscopy and ion mobility techniques provide detailed lipoprotein particle analysis. These advanced tests measure LDL particle number and size distribution, offering superior cardiovascular risk prediction. Additionally, small dense LDL particles demonstrate increased atherogenicity compared to large buoyant LDL particles.

✅ Comprehensive Lipid Assessment Checklist:
• Standard lipid panel (total cholesterol, LDL, HDL, triglycerides)
• Non-HDL cholesterol calculation
• Apolipoprotein B measurement
• Lipoprotein(a) testing
• Consider advanced particle analysis in high-risk patients
• Assess family history and genetic risk factors
Epidemiological Insights: Population Trends and Risk Factors
Recent epidemiological data reveals concerning trends in triglyceride and cholesterol distributions across diverse populations. According to NHANES 2007-2014 data, approximately 25% of US adults maintain triglyceride levels above 150 mg/dL. Moreover, this prevalence increases to 31.6% among patients already receiving statin therapy, indicating substantial residual risk.
Age-related changes significantly affect lipid metabolism and optimal target ranges. For instance, triglyceride levels typically increase with advancing age in both men and women. However, women experience more dramatic triglyceride elevation after menopause due to hormonal changes affecting lipid metabolism. Consequently, post-menopausal women require enhanced cardiovascular risk monitoring.
Gender differences extend beyond hormonal influences to include genetic and lifestyle factors. Men generally develop elevated triglycerides earlier than women, particularly during middle age. Furthermore, men show higher prevalence of combined hyperlipidemia with both elevated triglycerides and LDL cholesterol. These patterns necessitate gender-specific approaches to lipid management.
Metabolic Syndrome and Lipid Interactions
Metabolic syndrome represents a cluster of cardiovascular risk factors including elevated triglycerides, reduced HDL cholesterol, and insulin resistance. Importantly, this condition affects approximately 35% of US adults and dramatically increases cardiovascular disease risk. Additionally, metabolic syndrome patients frequently require combination therapy targeting multiple lipid abnormalities simultaneously.
The pathophysiology of metabolic syndrome involves complex interactions between adipose tissue inflammation, insulin resistance, and dyslipidemia. Specifically, visceral adiposity releases inflammatory cytokines that impair insulin signaling and increase hepatic triglyceride synthesis. Subsequently, these metabolic changes promote atherogenic lipoprotein production and cardiovascular disease progression.
“Understanding the intricate relationships between triglycerides, LDL cholesterol, and metabolic health enables clinicians to provide more effective cardiovascular risk reduction strategies.”
Evidence-Based Management Strategies: Optimizing Lipid Profiles
Achieving optimal triglycerides normal values and LDL cholesterol ranges requires evidence-based therapeutic interventions tailored to individual risk profiles. Initially, lifestyle modifications provide the foundation for lipid management across all risk categories. However, pharmacological therapy becomes essential for patients who cannot achieve targets through lifestyle changes alone.
⏳ Stepwise Lipid Management Protocol
Statin therapy represents the cornerstone of LDL cholesterol management with extensive evidence supporting cardiovascular benefit. Mayo Clinic research demonstrates that high-intensity statins can reduce LDL cholesterol by 50% or more in most patients. Furthermore, combination therapy with ezetimibe provides additional 13-20% LDL reduction when statins alone prove insufficient.
For triglyceride management, lifestyle interventions often produce dramatic improvements, particularly weight loss and refined carbohydrate restriction. However, patients with persistent hypertriglyceridemia may require pharmacological therapy with fibrates, omega-3 fatty acids, or newer agents targeting specific metabolic pathways.
Novel Therapeutic Approaches and Future Directions
Recent advances in lipid pharmacology have introduced innovative mechanisms for achieving optimal triglycerides normal values and LDL cholesterol ranges. PCSK9 inhibitors represent a major breakthrough, providing powerful LDL reduction through enhanced hepatic LDL receptor expression. Additionally, these agents demonstrate cardiovascular outcome benefits in high-risk populations.
Emerging triglyceride-targeted therapies include apolipoprotein C-III inhibitors and ANGPTL3 antagonists. These novel agents address specific components of triglyceride metabolism, offering hope for patients with severe hypertriglyceridemia resistant to conventional therapy. Furthermore, clinical trials investigating these approaches show promising results for both triglyceride reduction and cardiovascular event prevention.
Innovative LDL Therapies:
• PCSK9 inhibitors (alirocumab, evolocumab, inclisiran)
• Bempedoic acid for statin-intolerant patients
• Evinacumab for homozygous familial hypercholesterolemia
Advanced Triglyceride Treatments:
• Icosapent ethyl (purified EPA)
• Volanesorsen (apoC-III antisense)
• Pemafibrate (selective PPARα modulator)
Clinical Monitoring and Follow-Up: Ensuring Therapeutic Success
Effective lipid management requires systematic monitoring to ensure patients achieve and maintain optimal triglycerides normal values and LDL cholesterol ranges. Initially, baseline comprehensive lipid assessment establishes individual risk profiles and therapeutic targets. Subsequently, regular follow-up testing confirms therapeutic efficacy and identifies potential safety concerns.
✅ Monitoring Protocol for Lipid Management:
• Initial comprehensive lipid panel including apoB and Lp(a)
• Follow-up testing 6-8 weeks after therapy initiation or adjustment
• Annual lipid monitoring once stable on effective therapy
• Liver function assessment before and during statin therapy
• Creatine kinase monitoring if muscle symptoms develop
• Regular cardiovascular risk reassessment
The American Heart Association recommends lipid screening every 4-6 years for healthy adults, with more frequent monitoring for high-risk individuals. However, patients receiving lipid-lowering therapy require closer surveillance to optimize treatment effectiveness and minimize adverse effects.
Safety monitoring becomes particularly important with combination lipid therapies targeting both triglycerides and LDL cholesterol. For instance, combining statins with fibrates increases myopathy risk, necessitating careful patient selection and enhanced monitoring protocols. Additionally, some patients may experience drug interactions requiring dosage adjustments or alternative therapeutic approaches.
Personalized Medicine and Genetic Considerations

Pharmacogenomic testing increasingly guides optimal lipid management strategies by identifying patients likely to experience adverse effects or poor therapeutic responses. For example, SLCO1B1 polymorphisms predict statin-induced myopathy risk, while CYP2C8 variants affect fibrate metabolism. Consequently, genetic testing can inform safer, more effective treatment selection.
Familial hypercholesterolemia represents the most common genetic cause of premature cardiovascular disease, affecting approximately 1 in 250 individuals. These patients require aggressive LDL lowering from young age to prevent irreversible arterial damage. Furthermore, cascade screening of family members identifies additional high-risk individuals requiring early intervention.
For our comprehensive guide on managing elevated cholesterol levels, including detailed treatment protocols and lifestyle interventions, please reference our complete guide to understanding and managing high LDL levels.
Future Perspectives: Advancing Lipid Science and Cardiovascular Prevention
The evolving understanding of triglycerides normal values and LDL cholesterol ranges continues to reshape cardiovascular prevention strategies. Recent research reveals complex interactions between lipid metabolism, inflammation, and thrombosis that extend beyond traditional risk factor models. Moreover, emerging biomarkers and advanced imaging techniques provide enhanced cardiovascular risk assessment capabilities.
Artificial intelligence and machine learning applications increasingly support personalized lipid management by analyzing vast datasets to predict optimal therapeutic approaches. These technologies can identify subtle patterns in patient responses to different interventions, enabling more precise treatment selection. Furthermore, digital health platforms facilitate remote monitoring and medication adherence support for improved long-term outcomes.
The integration of lipid management with comprehensive cardiovascular risk reduction represents the future of preventive cardiology. This approach addresses not only triglycerides and LDL cholesterol but also blood pressure, diabetes management, smoking cessation, and lifestyle optimization. Consequently, patients receive coordinated care targeting all modifiable cardiovascular risk factors simultaneously.
Research continues to reveal new targets for lipid intervention, including novel pathways affecting triglyceride synthesis, cholesterol absorption, and lipoprotein metabolism. These discoveries promise even more effective therapies for achieving optimal lipid profiles in challenging patient populations. Additionally, outcome studies will continue to refine our understanding of optimal triglycerides normal values and LDL cholesterol ranges for different patient groups.
Understanding triglycerides normal values and LDL cholesterol ranges provides the foundation for effective cardiovascular risk management. Through evidence-based approaches combining lifestyle interventions with appropriate pharmacotherapy, clinicians can help patients achieve optimal lipid profiles and reduce their risk of atherosclerotic cardiovascular disease. Regular monitoring and personalized treatment strategies ensure sustained therapeutic success and improved long-term cardiovascular outcomes.
References
- National Heart, Lung, and Blood Institute. High Blood Triglycerides. Comprehensive guidelines on triglyceride classification and management strategies.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR Guideline on the Management of Blood Cholesterol. Circulation. 2019;139(25):e1082-e1143.
- Cleveland Clinic. Triglycerides: Levels & Normal Range. Evidence-based information on triglyceride physiology and clinical significance.
- Virani SS, Akeroyd JM, Nambi V, et al. Prevalence of US Adults with Triglycerides ≥ 150 mg/dl: NHANES 2007–2014. Cardiol Ther. 2020;9(1):207-213.
- Cleveland Clinic. Cholesterol: Understanding Levels & Numbers. Comprehensive analysis of cholesterol interpretation and clinical applications.
- American Heart Association. What Your Cholesterol Levels Mean. Expert guidance on cholesterol risk assessment and management.
- Karanchi H, Muppidi V, Wyne K. Hypertriglyceridemia. StatPearls. 2023 Aug 14.
- MedlinePlus. Triglycerides Test. National Library of Medicine comprehensive testing information.
Related Articles
Author Bio
The Remedy Verified Team translates complex metabolic science into clear, practical strategies for everyday health.
Disclaimer
This article is for educational purposes only and does not constitute medical advice. Always consult with qualified healthcare professionals before making any changes to your medical care or treatment plan. Individual results may vary, and this information should not be used to diagnose, treat, cure, or prevent any medical condition.