Understanding High LDL Cholesterol: Complete Guide to Causes, Management, and Treatment Options
High LDL cholesterol represents one of the most significant modifiable risk factors for cardiovascular disease, affecting nearly 25 million American adults. However, the landscape of LDL management has evolved dramatically in recent years, with groundbreaking research revealing new mechanisms of cholesterol metabolism and innovative treatment approaches that extend far beyond traditional statin therapy.
The Molecular Mechanisms Behind High LDL Cholesterol
Recent NIH research published in Nature has revolutionized our understanding of how LDL cholesterol accumulates in the bloodstream. Scientists have now visualized, for the first time, the precise molecular interactions between LDL particles and their receptors—discoveries that explain why some individuals develop dangerously high cholesterol levels despite following heart-healthy lifestyles.
The process begins when your liver produces cholesterol and packages it into LDL particles for transport throughout your body. Normally, LDL receptors on liver cells capture these particles and remove them from circulation. However, genetic mutations can impair this clearing mechanism, causing LDL to accumulate and eventually deposit as plaque in arterial walls.
⏳ How LDL Buildup Occurs:

Step 1: Liver produces cholesterol and packages it into LDL particles
Understanding LDL Cholesterol Levels and Diagnostic Criteria
Current medical guidelines categorize LDL cholesterol levels into distinct ranges, though recent research suggests these traditional thresholds may require personalization based on individual risk factors. Moreover, the 2025 American College of Cardiology guidelines have lowered treatment thresholds, recognizing that “lower is better” for most patients.
| LDL Cholesterol Level | Classification | Cardiovascular Risk | Treatment Approach |
|---|---|---|---|
| Less than 100 mg/dL | Optimal | Low | Lifestyle maintenance |
| 100-129 mg/dL | Near optimal | Mild increase | Lifestyle modifications |
| 130-159 mg/dL | Borderline high | Moderate increase | Intensive lifestyle changes |
| 160-189 mg/dL | High | Significant increase | Medication consideration |
| 190 mg/dL or higher | Very high | Substantial increase | Immediate medication |
Primary Causes of Elevated LDL Cholesterol
Understanding why LDL cholesterol becomes elevated requires examining both modifiable and non-modifiable factors. Interestingly, recent research has challenged some long-held assumptions about dietary cholesterol’s impact on blood cholesterol levels.
Genetic Factors and Familial Hypercholesterolemia
Approximately one in 250 people carries genetic mutations causing familial hypercholesterolemia (FH), a condition that can elevate LDL cholesterol levels above 190 mg/dL from birth. FH affects about 1.3 million Americans, yet 90% remain undiagnosed. The condition results from mutations in genes controlling LDL receptor function, PCSK9 protein production, or apolipoprotein B structure.
Dietary Influences: Separating Fact from Fiction

Contrary to popular belief, recent controlled feeding studies demonstrate that dietary cholesterol from eggs has minimal impact on blood cholesterol levels compared to saturated fat intake. The primary dietary culprits for elevated LDL include saturated fats found in red meat, full-fat dairy products, and processed foods.
• Red meat and processed meats (beef, pork, sausage, bacon)
• Full-fat dairy products (whole milk, butter, cheese)
• Tropical oils (coconut oil, palm oil)
• Fried foods and fast food items
• Commercial baked goods with trans fats
• Foods high in saturated fat content
Metabolic and Lifestyle Factors
Beyond genetics and diet, several metabolic conditions contribute to elevated LDL cholesterol. These factors often interconnect, creating a cascade effect that compounds cardiovascular risk.
Physical inactivity reduces HDL cholesterol levels while allowing LDL to remain elevated. Additionally, excess weight around the midsection correlates with higher triglycerides and lower HDL, creating an atherogenic lipid profile. Smoking compounds these effects by damaging arterial walls and reducing the body’s ability to clear cholesterol effectively.
Evidence-Based Lifestyle Interventions for LDL Management
Research from the National Cholesterol Education Program demonstrates that comprehensive lifestyle interventions can achieve substantial LDL reductions. The most effective approaches combine specific dietary modifications with structured physical activity programs.
The Therapeutic Lifestyle Changes (TLC) Protocol
The TLC approach represents the gold standard for non-pharmaceutical cholesterol management. This evidence-based program focuses on three core components: targeted nutrition, regular exercise, and weight management.
⏳ TLC Implementation Strategy:
Advanced Dietary Strategies for LDL Reduction
Recent meta-analyses reveal that specific foods provide targeted cholesterol-lowering benefits beyond general dietary improvements. These functional foods work through multiple mechanisms, including blocking cholesterol absorption, increasing cholesterol excretion, and reducing hepatic cholesterol synthesis.
• Oats and oat bran (3-4g daily)
• Beans and legumes (1/2 cup daily)
• Apples and citrus fruits with pectin
• Psyllium fiber supplements (5-10g)
• Fortified margarines and spreads
• Sterol-enriched orange juice
• Nuts, especially almonds and walnuts
• Vegetable oils (olive, canola, sunflower)
Omega-3 fatty acids from fatty fish provide additional cardiovascular benefits beyond LDL reduction. Studies show that consuming fish twice weekly can lower triglycerides while providing anti-inflammatory effects that protect arterial walls from plaque formation.
Exercise Protocols for Optimal Cholesterol Management

Physical activity affects cholesterol levels through multiple pathways. Aerobic exercise primarily increases HDL cholesterol and improves LDL particle size, while resistance training helps maintain muscle mass during weight loss efforts.
Medical Treatment Options for High LDL Cholesterol
When lifestyle interventions prove insufficient for achieving target LDL levels, pharmaceutical interventions become necessary. The treatment landscape has expanded significantly beyond traditional statin therapy, offering multiple options for patients who cannot tolerate standard treatments or require additional LDL reduction.
Statin Therapy: Mechanism and Efficacy
Statins remain the first-line treatment for elevated LDL cholesterol, working by inhibiting HMG-CoA reductase, the rate-limiting enzyme in cholesterol synthesis. High-intensity statins can reduce LDL cholesterol by 50% or more, with proven cardiovascular outcome benefits across diverse patient populations.
However, statin effectiveness varies considerably among individuals due to genetic polymorphisms affecting drug metabolism. Additionally, some patients experience muscle-related side effects that limit their ability to tolerate optimal doses.
PCSK9 Inhibitors: Revolutionary LDL Reduction
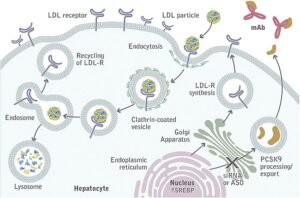
The development of PCSK9 inhibitors represents a paradigm shift in cholesterol management. These medications work by blocking PCSK9 protein, which normally destroys LDL receptors. By preserving more LDL receptors, PCSK9 inhibitors enhance the liver’s ability to clear cholesterol from circulation.
Currently available PCSK9 inhibitors include:
**Monoclonal Antibodies:**
– Alirocumab (Praluent): Administered every 2-4 weeks
– Evolocumab (Repatha): Available in monthly and biweekly formulations
**Small Interfering RNA (siRNA):**
– Inclisiran (Leqvio): Requires only twice-yearly injections after initial dosing
Emerging Treatment Approaches
Several innovative therapies are advancing through clinical development, offering hope for patients with refractory hypercholesterolemia. Gene editing technologies, including CRISPR-based approaches, show promise for permanently reducing PCSK9 production and achieving long-lasting LDL reduction.
Additionally, combination therapies using multiple mechanisms simultaneously can achieve greater LDL reduction than any single agent. For example, combining high-intensity statins with ezetimibe and PCSK9 inhibitors can reduce LDL cholesterol by 80% or more.
Special Considerations and Complex Cases
Familial Hypercholesterolemia Management
Patients with genetic forms of hypercholesterolemia require aggressive treatment from an early age. Children with familial hypercholesterolemia may need statin therapy as young as 8-10 years old to prevent premature atherosclerosis.
For individuals with homozygous familial hypercholesterolemia—the most severe form affecting 1 in 250,000 people—standard medications may prove insufficient. These patients often require LDL apheresis, a procedure that filters cholesterol directly from the blood, performed every 1-2 weeks.
• Genetic testing for family members
• Early initiation of high-intensity statins
• Addition of ezetimibe if LDL remains elevated
• PCSK9 inhibitors for inadequate response
• LDL apheresis for homozygous cases
• Lifestyle counseling for entire family
Controversial Research and Evolving Perspectives
Recent studies have challenged some traditional assumptions about cholesterol and cardiovascular risk. A 2025 study from The Lundquist Institute found that metabolically healthy individuals following ketogenic diets showed no correlation between high LDL levels and arterial plaque accumulation, suggesting that cholesterol may not universally predict cardiovascular risk.
Similarly, research from Sardinia’s longevity zones demonstrated that individuals over 90 with higher cholesterol levels actually lived longer than those with lower levels. These findings emphasize the importance of individualized risk assessment rather than universal cholesterol targets.
Monitoring and Long-term Management Strategies
Effective LDL cholesterol management requires ongoing monitoring and adjustment of treatment strategies. The frequency of testing depends on baseline risk factors, treatment intensity, and response to interventions.
⏳ Monitoring Schedule:

Baseline: Complete lipid panel, liver enzymes, HbA1c
Integration with Comprehensive Cholesterol Management
Understanding high LDL cholesterol requires viewing it within the broader context of lipid metabolism and cardiovascular health. For comprehensive information about cholesterol management, including HDL optimization and triglyceride control, refer to our detailed complete guide to understanding and managing high cholesterol levels.
This integrated approach ensures that LDL reduction strategies complement overall cardiovascular health optimization rather than focusing solely on a single biomarker.
Future Directions and Emerging Research
The field of cholesterol management continues evolving rapidly, with several promising developments on the horizon. Oral PCSK9 inhibitors currently in Phase 2 trials could eliminate the need for injections while maintaining efficacy. Gene therapy approaches may offer one-time treatments providing lifelong cholesterol control.
Additionally, artificial intelligence algorithms are being developed to predict individual responses to different cholesterol-lowering therapies, enabling precision medicine approaches that optimize treatment selection based on genetic and metabolic profiles.
The future of cholesterol management lies in personalized medicine approaches that consider individual genetic profiles, metabolic status, and lifestyle factors rather than one-size-fits-all treatment protocols.
Conclusion: Taking Control of Your LDL Cholesterol
High LDL cholesterol represents a significant but manageable cardiovascular risk factor. Recent scientific advances have provided unprecedented insights into cholesterol metabolism while expanding treatment options beyond traditional approaches. Whether through comprehensive lifestyle modifications, targeted medications, or combination therapies, effective LDL management can dramatically reduce cardiovascular risk.
The key lies in early detection, accurate risk assessment, and implementation of evidence-based interventions tailored to individual needs and preferences. By understanding the mechanisms behind cholesterol elevation and working closely with healthcare providers, individuals can achieve optimal LDL levels and protect their long-term cardiovascular health.
References
- NIH Research Reveals New Insights About How ‘Bad’ Cholesterol Works in the Body. National Institutes of Health. April 2025.
- 2018 AHA/ACC/AACVPR Guideline on the Management of Blood Cholesterol. American Heart Association. 2018.
- Maturation of Lipid Management in the 2025 ACC/AHA Acute Coronary Syndrome Guideline. Journal of the American College of Cardiology. 2025.
- The Latest Thinking on Inherited High Cholesterol. Harvard Health Publishing. December 2024.
- New Drug Used in Combination Therapy Reduces LDL Cholesterol. Cleveland Clinic. May 2025.
- New Study Shakes Up Heart Disease Theory. SciTechDaily. April 2025.
- Impact of Dietary Cholesterol from Eggs and Saturated Fat on LDL Cholesterol Levels. American Journal of Clinical Nutrition. 2025.
- What is Familial Hypercholesterolemia? American Heart Association. August 2024.
- Therapeutic Lifestyle Changes (TLC) To Lower Cholesterol. National Heart, Lung, and Blood Institute.
- PCSK9 Inhibitors: How They Manage Cholesterol. Cleveland Clinic. March 2025.
- Emerging Gene Therapies For Familial Hypercholesterolemia. American College of Cardiology. 2025.
- What to Do When High Cholesterol Runs in Your Family. Johns Hopkins Medicine. May 2025.
Author Bio
The Remedy Verified Team translates complex metabolic science into clear, practical strategies for everyday health.
Medical Disclaimer
This content is for informational purposes only and should not replace professional medical advice. Always consult with your healthcare provider before making changes to your treatment plan or starting new medications. Individual results may vary, and treatment decisions should be made in consultation with qualified medical professionals who can assess your specific health conditions and risk factors.