Types of Eye Floaters Pictures: Visual Guide to What You See

You’re seeing dark spots, threads, or cobweb-like shapes floating across your vision when you look at bright surfaces—and you need to know what you’re dealing with. When you search for types of eye floaters pictures online, you’ll find mostly artistic renderings that don’t match what you actually see. Here’s why: floaters are three-dimensional structures floating inside your eye, casting shadows on your retina. No external camera can photograph these internal shadows, which is why every “floater picture” online is either a simulation or someone’s artistic interpretation.What you need instead? Detailed visual descriptions that match your actual experience. This guide provides precise descriptions of eight distinct floater patterns—what they look like, how they move, and what causes each one. You’ll learn which patterns indicate normal vitreous aging versus those signaling retinal tears or posterior vitreous detachment requiring care within 24–48 hours. Floater type, quantity, and timing determine whether you need emergency evaluation or safe monitoring—accurate identification protects your vision.By the end, you’ll have a self-assessment framework for identifying your specific floater type, understanding the vitreous humor changes creating it, and recognizing exactly when to schedule same-day ophthalmology evaluation versus when observation is appropriate.
What Eye Floaters Look Like: Quick Visual Reference
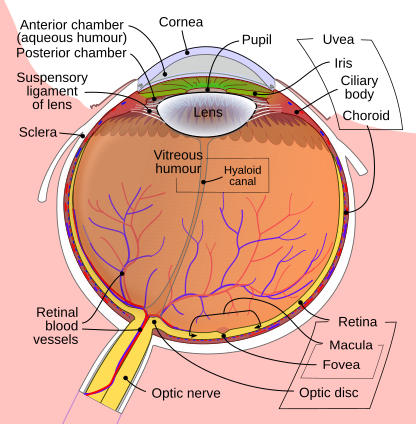
Eye floaters are shadows cast on your retina by tiny clumps of collagen protein or cellular debris suspended in the vitreous humor—the gel-like substance filling 80% of your eye’s interior. They become most visible against uniform bright backgrounds (blue sky, white walls, computer screens). Why? The contrast makes the shadows stand out, and your pupil constricts in bright light, sharpening the shadow edges.
Quick identification tip: The floater pattern you see reflects the three-dimensional structure of whatever’s casting the shadow. Thread-like floaters are literally strands of collapsed vitreous collagen. Ring floaters are circular because they’re cross-sections of tube-shaped structures.
| Floater Type | What You See | Primary Cause | Action Level |
|---|---|---|---|
| Cobweb/Thread | Thin squiggly lines, broken spider web strands, hair-like fibers | Collagen fiber clumping from vitreous aging | Benign (monitor) |
| Spot/Dot | Small dark circles, varying from pinpoint to BB-size | Condensed vitreous gel or cellular debris | Benign (monitor) |
| Weiss Ring | Large circular or C-shaped ring, doughnut appearance | Vitreous detachment from optic nerve head | Schedule exam (non-urgent) |
| Cloud/Diffuse | Hazy patches with soft edges, smoke-like shadows | Widespread vitreous liquefaction | Benign (monitor) |
| Dense Black Spot | Nearly opaque dark area blocking vision briefly | Blood cell clump or dense cellular aggregate | Evaluate timing (see below) |
| Sudden Shower | 20+ new floaters appearing within hours | Vitreous hemorrhage or retinal tear | Emergency (24 hours) |
| Curtain/Shadow | Gray veil moving across peripheral vision | Retinal detachment progression | Emergency (immediate) |
| Flashes + Floaters | Light sparks/lightning bolts with new floaters | Vitreous traction on retina | Urgent (same day) |
The timing of floater appearance often matters more than the type itself. A single cobweb floater developing gradually over weeks is fundamentally different from the same pattern appearing overnight alongside flashes—the latter requires immediate evaluation even though the visual description is identical.
Quick Self-Assessment: What Type Do You Have?
Answer these three questions to quickly identify your floater pattern:
- Shape: Does it look like threads/lines, dots/circles, a large ring, or hazy clouds?
- Timeline: Did it appear gradually over weeks/months, or suddenly within hours/days?
- Accompanying symptoms: Any flashes of light, shadows in peripheral vision, or vision loss?
If you answered:
- Threads + gradual + no other symptoms → Likely benign cobweb floaters from normal vitreous aging
- Dots/spots + gradual + no other symptoms → Likely benign spot floaters from vitreous condensation
- Large ring + recent (days-weeks) + no other symptoms → Likely Weiss ring from posterior vitreous detachment (schedule exam within 1-2 weeks)
- Any pattern + sudden (hours-days) + with flashes or shadows → Potential retinal tear or detachment (seek same-day evaluation)
- 20+ new floaters + sudden + any accompanying symptoms → Floater shower requiring emergency evaluation within 24 hours
8 Types of Eye Floaters: Detailed Visual Breakdown
The following descriptions explain exactly what each floater type looks like, how it moves, and what causes it. Use these visual details to match your experience and understand whether your floater pattern indicates normal aging changes or conditions requiring evaluation.
1. Cobweb/Thread Floaters (Fibrous Strand Type)
These are the most common floaters in people under 50. You’ll see thin, meandering lines that look like tangled fishing line, broken spider silk, or loose threads drifting slowly through your visual field. They typically appear semi-transparent or gray rather than solid black. The key identifying feature? Their wiggly, organic shape—they curve and loop rather than forming geometric patterns.
Movement behavior: Cobweb floaters lag behind your eye movements. Look left, and they drift left a moment later, then slowly drift back when your gaze stops. This delayed motion occurs because they’re suspended in liquid vitreous that moves like honey, not water. Some people describe it as watching seaweed wave in slow-motion currents.
What creates them: As vitreous humor ages, its collagen framework begins to collapse and clump together. Individual collagen fibrils—normally too small to see—bundle into thicker strands that cast visible shadows. Think of it like cotton candy forming from individual sugar molecules: the substance is the same, but the structure changes from invisible to visible. This process is a natural part of aging for the vitreous gel that fills your eye.
“The vitreous is about 98% water and 2% structure. When that structure fails, it creates the shadows we call floaters.”
— National Eye Institute, Vitreous Disorders Overview
Age correlation: Most common between ages 30–55. If you’re younger than 30 with prominent cobweb floaters, you may have high myopia (nearsightedness)—which accelerates vitreous changes by 10–15 years.
2. Spot/Dot Floaters
These appear as discrete circular shadows ranging from nearly microscopic pinpoints to spots the size of a small pea. Unlike threads, dots have defined edges and maintain a consistent round or oval shape. They often travel in small groups of 3–8 spots rather than appearing solo. Density varies: some are barely visible gray dots, while others are nearly opaque dark circles.
Movement behavior: Spot floaters tend to sink with gravity more than thread floaters do—they’re denser cellular aggregates rather than hollow collagen strands. You’ll notice them settling toward the bottom of your visual field when you look straight ahead, then rising slowly when you look down. This “bobbing” motion distinguishes them from other types.
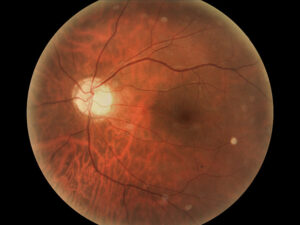
Transparency variations: Translucent gray spots suggest liquefied vitreous pockets or white blood cells from mild inflammation. Darker, more opaque spots typically contain red blood cells, melanin granules, or condensed cellular debris. A sudden change from gray to black in existing spot floaters warrants evaluation—it can indicate bleeding into the vitreous.
3. Ring/Circle Floaters (Weiss Rings)
Weiss rings are large circular or C-shaped floaters that suddenly appear, often described as looking through a smoke ring or seeing a floating doughnut. They’re typically 2–3 times larger than spot floaters and maintain a consistent circular shape. The ring may be complete or incomplete (appearing as a thick C or horseshoe), and the edges are usually well-defined rather than fuzzy.
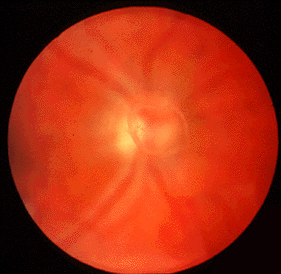
Clinical significance: A Weiss ring forms when the vitreous separates from the tissue surrounding your optic nerve (the point where your optic nerve enters the eye). The ring is literally a circular piece of glial tissue that pulled away during posterior vitreous detachment (PVD). While posterior vitreous detachment (PVD) is a normal aging process, it carries a 10–15% risk of creating a retinal tear during separation.
What to do: Schedule a dilated eye exam within 1–2 weeks of noticing a new ring floater, even without other symptoms. Your eye doctor will examine your peripheral retina for tears. Most Weiss rings are benign, but the examination is essential—small tears are treatable with laser if caught early.
Age correlation: Typically appears between ages 55–75, though it can occur earlier in highly myopic eyes or after eye trauma/surgery.
4. Cloud/Diffuse Floaters
These are hazy, undefined shadows with soft edges that look like smoke, fog, or gauze drifting through your vision. Unlike the sharp-edged patterns of threads or rings, cloud floaters have gradual transitions from darker centers to lighter peripheries. Some people describe them as “smudges on glasses that move when I try to look at them.”
Movement behavior: Cloud floaters move more slowly and smoothly than other types because they represent widespread changes throughout the vitreous rather than discrete objects. They rarely dart or wiggle—instead, they glide like slow-moving storm clouds.
Clinical note: While usually benign, extensive cloud floaters can occasionally indicate asteroid hyalosis (calcium-lipid deposits) or, more rarely, inflammatory conditions like vitritis. If clouds are accompanied by decreased vision, eye pain, or redness, same-day evaluation is warranted.
5. Dense Black Spot Floaters
These are nearly opaque dark areas that temporarily block your vision when they drift across your central visual axis. They’re darker and denser than typical gray spot floaters, appearing as solid black circles or irregular blobs. The key distinguishing feature? They noticeably obscure whatever you’re looking at for a second or two as they pass through your line of sight.
Composition: Dense black floaters usually contain red blood cells from microscopic vitreous hemorrhages. Small bleeds can occur from normal vitreous separation tugging on tiny retinal blood vessels. While often harmless, the concern is why bleeding occurred—was it benign traction or a retinal tear?
Decision rule: One or two dense black spots appearing gradually over weeks typically don’t require urgent care. However, multiple dark spots appearing within 24 hours, or any black spots with flashes of light, require same-day evaluation to rule out retinal tear or detachment.
6. Sudden Shower of Floaters
This describes the abrupt appearance of dozens of new floaters—often a mix of spots, threads, and dark streaks—appearing within hours rather than days or weeks. People often describe it as “pepper specks,” “a swarm of gnats,” or “looking through dirty water.” The sheer quantity differentiates this from normal floater development.
“More than 20 new floaters appearing suddenly is a red flag for retinal tear until proven otherwise.”
— American Academy of Ophthalmology Retinal Guidelines
Why it’s urgent: A floater shower typically indicates vitreous hemorrhage (bleeding into the vitreous cavity) or a cascade of cellular debris from a retinal tear.
What causes it: During posterior vitreous detachment, the vitreous pulls away from the retinal surface. If a blood vessel tears during this separation, red blood cells flood the vitreous, creating the shower effect. Alternatively, if the retina itself tears, cellular debris from the damaged tissue creates similar symptoms.
7. Curtain or Shadow in Peripheral Vision

This isn’t a floater in the traditional sense—it’s a gray or dark veil that obscures part of your peripheral (side) vision and progressively moves inward. It may look like a curtain being drawn across your visual field from the side, top, or bottom. Unlike floaters that move with eye movement, this shadow stays in a fixed area of your vision.
What it means: A moving curtain/shadow indicates progressive retinal detachment—the retina is peeling away from the back wall of the eye. The shadow represents the area where your retina is no longer functioning. This is an ophthalmic emergency—retinal detachment requires surgery within 24–48 hours to prevent permanent vision loss in that eye.
⚠️ Emergency protocol: If you notice a curtain or shadow, stop reading this article and call an ophthalmologist or go to an emergency room immediately. Do not wait until morning if it’s nighttime; do not wait until Monday if it’s the weekend. Retinal detachment is one of the few true eye emergencies.
8. Flashes of Light (Photopsia) With Floaters
Flashes appear as brief sparks, lightning bolts, or camera-flash effects in your peripheral vision, often accompanied by new floaters. The flashes typically last a fraction of a second and may occur repeatedly over hours or days. They’re most noticeable in dim lighting or with eyes closed, appearing on the temporal (outer) side of your visual field.
Mechanism: Flashes occur when the vitreous tugs on the retina (a phenomenon known as photopsia in medical terminology), mechanically stimulating the photoreceptor cells. Your brain interprets this mechanical stimulation as light, even though no external light entered your eye. Think of it like the phenomenon of “seeing stars” when you bump your head—mechanical stimulation creates a light sensation.
Clinical significance: Flashes alone (without new floaters) often indicate benign vitreous traction and resolve as PVD completes. However, flashes plus new floaters together suggest the traction is strong enough to tear retinal tissue or cause bleeding, requiring same-day or next-day examination. The combination carries higher risk than either symptom alone.
Duration matters: Flashes lasting weeks to months with stable floaters suggest completed PVD (low risk). Flashes plus increasing floaters over days suggest ongoing traction (higher risk requiring evaluation).
How to Monitor Your Eye Floaters Over Time: A Data-Driven Protocol
Most guidance tells you to “watch for changes” in floaters—but that advice is too vague to be actionable. What specific changes matter? How often should you check? What observations help your ophthalmologist make better decisions? This systematic monitoring protocol gives you concrete criteria and a simple tracking framework. It’s the same approach we apply to metabolic markers, blood pressure, and other health metrics where trend data outperforms snapshots.
The Weekly Sky Test (Structured Observation Protocol)
Floaters are notoriously inconsistent—they seem worse on tired days, in certain lighting, or when you’re anxious about them. That’s why standardized observation conditions eliminate noise from your data. Here’s the protocol used in floater research studies, adapted for home use:
Standardized testing conditions:
- Time: Mid-morning (10–11 AM) when lighting is consistent and you’re not fatigued
- Location: Stand in the same outdoor spot with clear sky view, or use the same white wall indoors
- Method: Look at the sky/wall for 30 seconds per eye (cover the other), moving your gaze slowly up-down, then left-right
- Documentation: Immediately note count, type, and subjective density (1–10 scale) while the image is fresh
What to record each week: Most people track too much or too little. Focus on these four variables that correlate with clinical significance:
| Variable | What to Note | Why It Matters |
|---|---|---|
| Quantity | Approximate count (1–5, 6–15, 16–30, 30+) | Sudden jumps (doubling within 7 days) warrant evaluation |
| Density/Opacity | Rate visibility 1–10 (1=barely visible, 10=blocks vision) | Increase of 3+ points suggests hemorrhage or inflammation |
| Dominant Type | Threads, spots, rings, clouds (pick primary pattern) | Type changes (threads → spots) indicate new process |
| Flash Activity | None / occasional / frequent (per day) | New or increasing flashes override stable floater readings |
Why weekly? Daily tracking creates anxiety and overdetection—you’ll notice normal fluctuations that don’t matter clinically. Monthly gaps miss acute changes requiring intervention. Weekly cadence balances sensitivity with sustainable effort, and it provides your ophthalmologist with useful trend data rather than a single-day snapshot that may be unrepresentative.
Stop Criteria: When to Escalate From Monitoring to Action
One of the most valuable aspects of tracking? Knowing when to stop tracking and seek evaluation. These thresholds are based on retinal tear risk stratification from ophthalmology literature, translated into observable criteria you can apply at home without medical equipment:
Schedule same-day or next-day evaluation if:
- Floater count doubles within any 7-day period (e.g., 6 → 12 floaters)
- Density score increases by 3+ points within 2 weeks
- New flashes appear alongside increasing floaters
- Type changes from benign pattern (threads/clouds) to concerning pattern (rings/dense spots)
- Any shadowing or curtain effect in peripheral vision, regardless of floater stability
Schedule routine exam (2–4 weeks) if:
- New Weiss ring appears without other symptoms
- Gradual increase in floater count over 4–8 weeks (suggesting ongoing PVD)
- Persistent subjective concern despite stable measurements
Continue monitoring if:
- All metrics remain stable for 4+ consecutive weeks
- Minor fluctuations (±2 floaters, ±1 density point) with no trend direction
- Floaters present >6 months without recent changes
Preparing for Your Ophthalmology Visit: Bring Objective Data

When you coordinate with your eye doctor, trend data outperforms subjective descriptions. “I think they’re getting worse” is less actionable than “My count went from 8 to 17 over three weeks, and density increased from 4/10 to 7/10.” Here’s what to bring:
- Your tracking log: 4–8 weeks of weekly observations shows whether changes are acute or gradual
- First-notice date: When did you first observe current floaters? Acute onset (<7 days) vs. chronic (months/years) changes urgency
- Associated symptoms timeline: Flashes, shadows, vision changes—map them to floater changes
- Risk factors: High myopia, previous eye surgery/trauma, family history of retinal detachment, diabetes
This structured data helps your ophthalmologist stratify your risk more accurately than clinical examination alone. Studies show that patient-reported symptom progression predicts retinal pathology as reliably as some clinical signs—but only when the reporting is systematic rather than impressionistic.
Factors That Affect Floater Visibility (What Actually Helps)
No lifestyle change or supplement eliminates existing floaters—the collagen clumps are structural, not metabolic. However, certain factors affect how prominently you notice them, which matters for daily quality of life even if the vitreous floaters themselves remain unchanged.
What may reduce floater awareness:
- Consistent hydration: The vitreous is 98% water. While no studies prove dehydration worsens eye floater symptoms, some people report less prominent floaters when well-hydrated. Low-risk to try; don’t expect dramatic changes.
- Screen break protocol: The 20-20-20 rule (every 20 minutes, look 20 feet away for 20 seconds) reduces eye strain. Won’t eliminate floaters but may reduce the cognitive effort of filtering them out.
- Metabolic optimization: If you have diabetes or inflammatory conditions, optimizing control has extensive benefits—potential floater reduction is speculative but costs nothing extra since you should optimize these anyway.
“We focus on monitoring rather than interventions because objective data guides timing, not supplements.”
— Remedy Verified Clinical Monitoring Framework
Why monitoring beats intervention: Unlike blood pressure or blood sugar (where lifestyle changes produce measurable improvements), vitreous floaters have no proven natural remedies. Once collagen fibers clump, they don’t un-clump through diet or supplements. Your effort is better invested in the systematic monitoring system below—it catches sight-threatening retinal complications when early treatment is most effective.
Common Myths About Eye Floaters: Separating Fact From Fiction
| Myth | Fact |
|---|---|
| “All floaters are harmless and just part of aging.” | Most floaters are benign, but timing and pattern matter critically. A sudden shower of floaters or floaters with flashes can signal retinal tears requiring treatment within 24–48 hours. The floater type matters less than whether it appeared gradually or suddenly. |
| “Eye exercises or supplements can dissolve floaters.” | No evidence supports this claim. Floaters result from structural collagen clumping in the vitreous—a physical change that doesn’t respond to nutritional or movement interventions. Marketing claims for pineapple enzymes, turmeric, or eye yoga? They lack clinical trial support. |
| “Floaters always go away on their own.” | Some floaters persist indefinitely. While your brain often learns to filter them out (neural adaptation), the physical floaters may remain. Floaters present at birth typically last lifelong, while those from posterior vitreous detachment may fade as they settle below your line of sight—but this takes months to years, not weeks. |
| “If my eye exam was normal last year, new floaters aren’t concerning.” | Retinal conditions develop acutely. A normal exam 6–12 months ago doesn’t protect you from current tears or detachment. New floaters (especially if sudden or accompanied by flashes) require current evaluation—regardless of past exam results. |
| “Floaters are just in my head or related to stress.” | Floaters are real physical structures casting shadows on your retina—they’re not imagined or psychosomatic. However, awareness of floaters can increase with anxiety or attention focus. The floaters exist whether you’re stressed or calm, but stress may make you notice them more. |
| “Young people don’t get floaters.” | While floaters are most common after age 50, young adults (especially those with high myopia) frequently develop them. About 25% of people under 40 report floaters. High myopia, eye trauma, or inflammatory conditions accelerate vitreous changes that typically occur with aging. |
Frequently Asked Questions About Eye Floater Types
Can eye floaters change type over time?
Yes. As posterior vitreous detachment progresses, thread-like floaters may consolidate into larger clumps or develop into Weiss rings. Additionally, new processes (like vitreous hemorrhage) can add different types alongside existing ones. However, a sudden type change—especially from benign patterns to dense spots or rings—warrants evaluation because it suggests a new vitreous event rather than gradual evolution.
What’s the most common type of eye floater?
Cobweb/thread floaters are most common overall, representing about 60–70% of reported floaters. Spot floaters are second most common (20–25%), while Weiss rings and cloud floaters are less frequent (5–10% each). However, most people with chronic floaters have a mix of types rather than a single pure pattern.
Do younger people get different types of floaters than older adults?
Generally yes. People under 40 more often report thread/cobweb floaters or small clusters of spots, typically related to high myopia or premacular bursa floaters. Weiss rings and diffuse cloud floaters are more characteristic of the posterior vitreous detachment process, which typically occurs after age 50. Dense black spots from vitreous hemorrhage can occur at any age but become more common with advancing years.
Can you have multiple types of floaters at once?
Absolutely. It’s common to have threads and spots, or a Weiss ring with scattered smaller floaters. Each floater represents a different structure in your vitreous, so multiple patterns simply mean multiple clumps or strands exist. The presence of multiple types isn’t concerning by itself—what matters is whether they appeared suddenly or gradually accumulated over time.
How many floaters are too many?
There’s no absolute number, but context matters. If you’ve had 10–15 stable floaters for years, that’s typically benign. However, going from 5 floaters to 25+ within days signals potential vitreous hemorrhage or retinal tear requiring immediate evaluation. The rate of change matters more than the total count. As a rough guideline: sudden appearance of 20+ new floaters within hours to days is a medical emergency.
Are black floaters more dangerous than gray ones?
Not necessarily, but density combined with timing matters. Gray translucent floaters usually represent collagen strands or white blood cells and are typically benign. Dense black floaters more often contain red blood cells from minor vitreous hemorrhage. A few black floaters developing gradually are usually harmless. Multiple new black floaters appearing within 24 hours suggest active bleeding and warrant same-day evaluation.
Why can’t eye floaters be photographed?
Floaters exist inside your eye, between the lens and retina, floating in the vitreous humor. They’re shadows cast on your retina—the light-sensing tissue at the back of your eye. External cameras photograph what light reflects off your eye’s surface, not the internal shadows your retina perceives. Even specialized ophthalmology cameras that photograph the retina can’t capture floaters the way you see them, though advanced imaging techniques help ophthalmologists plan treatments because the shadows constantly move and appear differently depending on viewing angle and lighting. This is why visual descriptions are more accurate than pictures for identifying what you’re experiencing.
What to Do Right Now: Your Next Steps
Based on your current situation, here’s your immediate action plan:
If You Have Emergency Signs (Act Within Hours)
- Sudden shower of 20+ new floaters
- Flashes of light with new floaters
- Dark curtain or shadow in peripheral vision
- Sudden vision loss in one eye
Action: Call an ophthalmologist immediately or go to an emergency room. Don’t wait until tomorrow if it’s evening. Don’t wait until Monday if it’s the weekend. Retinal detachment requires treatment within 24-48 hours—this is one of the few true eye emergencies.
If You Have Urgent Signs (Act Within Days)
- New large ring-shaped floater (Weiss ring)
- Multiple new dense black spots appearing over 2-3 days
- Floater count doubled within a week
Action: Schedule a dilated eye exam within 1-2 weeks. Call your eye doctor’s office and explain the symptoms—most practices have protocols for urgent floater evaluations. Be specific about timing and changes.
If You Have Stable Chronic Floaters (Monitor Systematically)
- Threads or spots present for months/years
- No recent changes in quantity or quality
- No flashes or shadows
Action: Start the weekly sky test protocol this week. Document your baseline (count, type, density rating 1-10) and set a recurring calendar reminder for the same day/time each week. This creates the trend data that distinguishes normal fluctuations from concerning changes.
If You’re Unsure Which Category You Fall Into
Action: Default to caution and schedule a routine eye exam. Explain your symptoms over the phone—the office can help determine urgency. Better to have a normal exam than to miss a treatable retinal tear.
Bottom Line
Understanding eye floater types isn’t about memorizing categories—it’s about recognizing the difference between structural aging that requires monitoring and acute changes that demand immediate care. The pattern you see matters less than how quickly it appeared and what symptoms accompany it. Thread floaters developing over months? Completely different risk profile than the identical pattern appearing overnight with flashes.
What separates effective floater management from anxious guessing? Systematic observation with clear decision criteria. Rather than vague instructions to “watch for changes,” you now have specific thresholds: quantity doubling within a week, density jumping 3+ points, new flashes alongside new floaters. These concrete markers eliminate ambiguity about when monitoring shifts to action. The weekly sky test protocol gives you reproducible data that helps your ophthalmologist assess risk more accurately than examination alone.
Most floaters are permanent but harmless. Your job isn’t to eliminate them—it’s to catch the rare cases where they signal retinal tears or detachment when early treatment prevents vision loss. Start your first observation this week using standardized conditions. Document your baseline. Trust that you’ll recognize meaningful changes when they occur. Systematic monitoring outperforms both dismissive waiting and constant anxiety.
References
- National Eye Institute. Floaters – Eye Conditions and Diseases. U.S. National Institutes of Health; 2024.
- American Academy of Ophthalmology. What Are Floaters and Flashes? AAO Patient Education; 2024.
- Hollands H, Johnson D, Brox AC, Almeida D, Simel DL, Sharma S. Acute-onset floaters and flashes: is this patient at risk for retinal detachment? JAMA. 2009;302(20):2243-2249.
- Sebag J. Vitreous and vision degrading myodesopsia. Prog Retin Eye Res. 2020;79:100847.
- Byer NE. Natural history of posterior vitreous detachment with early management as the premier line of defense against retinal detachment. Ophthalmology. 1994;101(9):1503-1514.
- American Society of Retina Specialists. Posterior Vitreous Detachment. Patient Information Resources; 2024.
- Stein JD, Zacks DN, Grossman D, et al. Adverse events after pars plana vitrectomy among Medicare beneficiaries. Arch Ophthalmol. 2009;127(12):1656-1663.
- Webb BF, Webb JR, Schroeder MC, North CS. Prevalence of vitreous floaters in a community sample of smartphone users. Int Ophthalmol. 2013;33(5):595-599.
Disclaimer
⚠️ Disclaimer: The information provided in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. Eye floaters can indicate serious conditions requiring immediate care. Always consult a qualified ophthalmologist or optometrist if you experience new floaters, sudden changes in existing floaters, flashes of light, or vision changes. This is especially critical if symptoms appear suddenly or worsen rapidly. Remedy Verified does not provide medical services, and the content shared here should not be considered a substitute for professional eye care. Retinal tears and detachment are medical emergencies—when in doubt, seek same-day evaluation. Use of this website and its information is at your own risk.