The Dawn Phenomenon Decoded: Why Your Morning Blood Sugar Is High (Despite Eating Nothing)
You wake up, check your blood sugar, and see a number that makes no sense: 165 mg/dL. But you haven’t eaten anything in 12 hours. You followed your diet perfectly yesterday. Your bedtime reading was normal. Yet somehow, while you were sleeping, your blood sugar skyrocketed. Welcome to the dawn phenomenon—one of the most frustrating and misunderstood aspects of blood sugar management.
Cleveland Clinic research confirms that dawn phenomenon affects over 50% of people with diabetes—both Type 1 and Type 2—yet most people don’t understand what’s actually happening or how to manage it effectively. The result? Frustration, higher A1C levels, and the feeling that your body is working against you.
What Is Dawn Phenomenon? (The Scientific Truth)
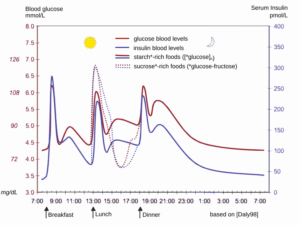
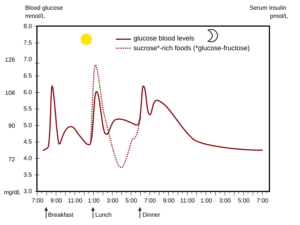
Dawn phenomenon isn’t a malfunction—it’s actually your body trying to do something helpful, but going overboard. Every single person experiences hormonal changes between 3 AM and 8 AM that are designed to help you wake up with energy. The problem? When you have diabetes or insulin resistance, this natural process goes haywire.
Here’s what’s actually happening: While you sleep, your body releases a cocktail of hormones including cortisol, growth hormone, epinephrine, and glucagon. These hormones signal your liver to dump stored glucose into your bloodstream—nature’s way of giving you energy to start the day. If you don’t have diabetes, your pancreas responds by releasing exactly the right amount of insulin to handle this glucose surge.
But if you have diabetes? Your pancreas either can’t produce enough insulin or your cells resist insulin’s effects. Result: all that glucose just sits in your bloodstream, creating those mysteriously high morning readings that seem to come from nowhere.
❌ Common Myth
Dawn phenomenon means you ate too much the night before or did something wrong with your diabetes management.
✅ Scientific Fact
Dawn phenomenon is a completely natural hormonal process that occurs in everyone—people with diabetes just can’t compensate for it properly.
The Hormone Orchestra: What’s Really Happening While You Sleep
Understanding dawn phenomenon requires grasping the complex hormonal symphony playing out in your body every night. Research shows that this isn’t just one hormone acting alone—it’s a carefully orchestrated process that begins around 3 AM.
2-3 AM: The Setup Phase
Growth hormone levels peak, triggering increased glucose production in the liver while simultaneously reducing insulin sensitivity in muscle and fat tissue.
4-5 AM: Cortisol Awakens
Cortisol begins its daily rise, further stimulating glucose production and creating insulin resistance. This is your body’s natural “wake-up call.”
6-7 AM: Peak Effect
Multiple hormones work together to maximize glucose availability. In healthy individuals, insulin compensates perfectly. In diabetes, glucose accumulates.
8-9 AM: Extended Dawn
Some people experience “extended dawn phenomenon” where elevated glucose persists even after eating breakfast, indicating more severe insulin resistance.
What makes this particularly challenging is that your body is naturally more insulin resistant in the morning hours compared to the rest of the day. This means even if your pancreas produces some insulin, it’s fighting an uphill battle against hormones that are actively working against it.
Dawn Phenomenon vs. The Somogyi Effect: Solving the Morning Mystery
Here’s where many people get confused—and even some healthcare providers miss this distinction. There are actually two different reasons your morning blood sugar might be high, and the treatments are completely different.
| Factor | Dawn Phenomenon | Somogyi Effect | Poor Control |
|---|---|---|---|
| Cause | Natural hormone release | Overnight hypoglycemia rebound | Insufficient medication |
| 3 AM Blood Sugar | Normal or high | Low (below 70 mg/dL) | High |
| Frequency | 50%+ of people with diabetes | Rare (possibly overestimated) | Variable |
| Treatment Approach | Strategic timing, lifestyle | Reduce nighttime insulin | Increase overall medication |
⚠️ Critical Distinction: Recent research using continuous glucose monitors suggests the Somogyi effect may be much rarer than previously thought. Most morning highs are actually dawn phenomenon or inadequate overnight insulin coverage.
The definitive way to distinguish between these causes? Check your blood sugar at 2-3 AM for several nights. If it’s normal or high, you’re dealing with dawn phenomenon. If it’s low, you might have the Somogyi effect (though this is increasingly uncommon with modern insulin preparations).
Why Dawn Phenomenon Gets Worse Over Time
One of the most frustrating aspects of dawn phenomenon is that it often worsens as diabetes progresses. Research published in ScienceDirect shows that both the duration of diabetes and HbA1c levels directly correlate with the magnitude of dawn phenomenon.
Early Diabetes/Prediabetes
- Mild dawn phenomenon (20-40 mg/dL rise)
- May only occur occasionally
- Often manageable with lifestyle changes
- Pancreas still produces some insulin
Advanced Diabetes
- Severe dawn phenomenon (60+ mg/dL rise)
- Occurs almost daily
- Requires medical intervention
- Minimal endogenous insulin production
This progression happens because of two converging factors: declining pancreatic function and increasing insulin resistance. As your pancreas produces less insulin over time, it becomes increasingly unable to compensate for those powerful morning hormones. Simultaneously, chronic high blood sugar levels worsen insulin resistance, creating a vicious cycle.
“Dawn phenomenon is like a stress test for your metabolic system—it reveals how much functional insulin capacity you have left.”
The Real Impact: Beyond Just Numbers
Many people think dawn phenomenon is just an annoying number on their glucose meter. That’s dangerously wrong. Persistent morning hyperglycemia contributes significantly to overall glycemic control and long-term complications.
The Hidden Consequences
Morning blood sugar spikes don’t just affect your A1C—they set a cascade of metabolic dysfunction that impacts your entire day. High morning glucose leads to increased insulin resistance throughout the day, making blood sugar control progressively more difficult.
Consider this: if your blood sugar spikes to 200 mg/dL every morning and takes 3-4 hours to normalize, you’re spending 25-30% of your day in a hyperglycemic state. Over months and years, this persistent exposure drives the complications we associate with poorly controlled diabetes: cardiovascular disease, neuropathy, nephropathy, and retinopathy.
But there’s another impact most people miss: the psychological toll. Waking up to high blood sugar readings every morning creates a sense of helplessness and failure, even when you’re doing everything “right.” This can lead to diabetes burnout and abandonment of otherwise good management strategies.
Diagnosing Dawn Phenomenon: The Right Way
Most people try to self-diagnose dawn phenomenon by looking at their morning readings compared to bedtime. While this gives clues, proper diagnosis requires understanding overnight glucose patterns, not just two data points.
For those without CGM access, systematic fingerstick testing can work, but it requires commitment. Mayo Clinic protocols recommend checking blood sugar at bedtime, 3 AM, and upon waking for at least 3-5 nights to establish a pattern.
DIY Dawn Phenomenon Detection Protocol:
- ✓ Test blood sugar at exactly the same times: bedtime (10-11 PM), 3 AM, and upon waking
- ✓ Record all readings along with any unusual events (stress, illness, medication changes)
- ✓ Look for a consistent pattern of morning readings 20+ mg/dL higher than 3 AM readings
- ✓ Note the timing of the glucose rise—true dawn phenomenon peaks between 6-8 AM
- ✓ Track for at least 5 different nights to account for daily variations
An alternative method developed by researchers involves calculating dawn phenomenon magnitude using pre-meal glucose readings. By comparing pre-breakfast glucose to the average of pre-lunch and pre-dinner readings, you can detect dawn phenomenon with 71% sensitivity and 68% specificity—not perfect, but useful for screening.
Treatment Strategies: What Actually Works
Here’s where most advice falls short: treating dawn phenomenon requires understanding that conventional diabetes management strategies often don’t work. Standard oral medications typically have minimal effect on dawn phenomenon, and simply increasing long-acting insulin can create dangerous overnight hypoglycemia.
⚠️ Treatment Pitfall: The instinct to increase overall insulin or medication doses to combat morning highs often leads to dangerous low blood sugar episodes later in the night, potentially causing the very rebound effect you’re trying to avoid.
The Insulin Pump Advantage
For people using insulin, insulin pump therapy represents the gold standard for dawn phenomenon management. Unlike long-acting insulin injections that provide steady insulin levels, pumps can be programmed to deliver precisely timed insulin increases during the early morning hours.
Pump Programming Strategy
- Midnight-3 AM: Lower basal rates to prevent overnight lows
- 3-6 AM: Gradually increase basal rates
- 6-9 AM: Peak basal rates to counter hormone surge
- 9 AM onwards: Return to normal daytime rates

Fine-Tuning Process
- Start Conservative: Small 10-20% increases in basal rates
- Monitor Closely: CGM data essential for adjustments
- Gradual Changes: Adjust one time period at a time
- Account for Variables: Stress, illness affect needs
Lifestyle Interventions: The Underestimated Approach
While medical management gets most attention, lifestyle interventions can significantly impact dawn phenomenon severity—sometimes more than medications. The key is understanding which interventions target the underlying hormonal processes.
Hormonal Disruption Pattern
- Late bedtimes (after midnight)
- Inadequate sleep (less than 6 hours)
- High stress levels
- Evening carbohydrate intake
- Sedentary evenings
Sleep optimization deserves special attention. Research shows that sleep deprivation and poor sleep quality directly worsen dawn phenomenon by disrupting cortisol rhythms and increasing insulin resistance. People who consistently sleep 6-8 hours and maintain regular sleep schedules show significantly lower dawn phenomenon severity.
Advanced Management: Beyond Basic Strategies
Once you’ve mastered the fundamentals, several advanced strategies can provide additional dawn phenomenon control. These approaches target specific aspects of the underlying physiology and are particularly helpful for people with severe or refractory dawn phenomenon.
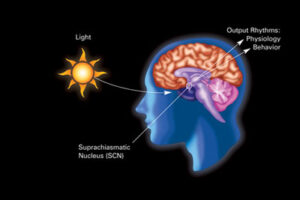
Circadian Rhythm Optimization
Your body’s internal clock directly influences hormone release patterns. Disrupted circadian rhythms can worsen dawn phenomenon by causing erratic cortisol and growth hormone release. Strategic light exposure and meal timing can help reestablish healthy circadian patterns.
Morning Light Exposure (6-8 AM)
Bright light exposure immediately upon waking helps establish strong circadian rhythms and may reduce cortisol dysregulation that contributes to dawn phenomenon.
Evening Light Restriction (after 9 PM)
Blue light exposure from screens can disrupt melatonin production and cortisol patterns. Using blue light filters or avoiding screens helps maintain natural hormone cycles.
Consistent Meal Timing
Eating at regular times helps synchronize metabolic rhythms. Having your largest meal earlier in the day when insulin sensitivity is highest can reduce dawn phenomenon severity.
Targeted Nutritional Strategies
Beyond basic carbohydrate restriction, specific nutrients and timing strategies can influence dawn phenomenon. Research indicates that the composition and timing of your last meal significantly impacts morning glucose levels.
Click to Expand: Supplement Strategies for Dawn Phenomenon
- Magnesium Glycinate (200-400mg): Supports healthy cortisol patterns and insulin sensitivity
- Chromium Picolinate (200-400mcg): May improve insulin function during morning hormone surge
- Alpha-Lipoic Acid (300-600mg): Enhances cellular glucose uptake and insulin sensitivity
- Melatonin (0.5-3mg): Supports healthy sleep and may modulate cortisol release timing
- Vitamin D3 (2000-4000 IU): Deficiency associated with worsened insulin resistance and dawn phenomenon
Always consult healthcare providers before starting new supplements, especially if taking medications.
When Dawn Phenomenon Signals Bigger Problems
While dawn phenomenon is common in diabetes, sudden worsening or extreme elevations can indicate underlying issues that require immediate attention. Understanding these warning signs can prevent serious complications.
Progressive worsening of dawn phenomenon often signals declining pancreatic function or increasing insulin resistance. This natural progression in diabetes requires proactive management adjustments rather than simply accepting higher morning readings as inevitable.
❌ Dangerous Assumption
“Dawn phenomenon is just something I have to live with—there’s nothing I can do about it.”
✅ Empowering Truth
Dawn phenomenon is highly manageable with the right combination of medical treatment, lifestyle optimization, and understanding of individual patterns.
The Connection to Overall Metabolic Health
Dawn phenomenon doesn’t exist in isolation—it’s intimately connected to overall metabolic health and often reflects broader issues with insulin sensitivity, stress management, and circadian health. This is why comprehensive approaches, like those outlined in The Ultimate Guide to Natural Diabetes Support, are essential for long-term management success.
People who successfully manage dawn phenomenon often find improvements in other areas: better energy throughout the day, improved mood stability, reduced cravings, and enhanced overall glucose control. This suggests that targeting dawn phenomenon can create positive cascading effects throughout your metabolic system.
Your Dawn Phenomenon Action Plan
Managing dawn phenomenon successfully requires a systematic approach tailored to your individual patterns and circumstances. Here’s a step-by-step protocol for taking control of your morning blood sugar readings.
Phase 1: Assessment (Weeks 1-2)
- Document current patterns with systematic testing
- Identify contributing factors (sleep, stress, diet)
- Establish baseline measurements
- Rule out other causes of morning highs
Phase 2: Implementation (Weeks 3-6)
- Optimize sleep hygiene and circadian rhythms
- Adjust evening meal composition and timing
- Implement stress management techniques
- Work with healthcare provider on medication timing
Phase 3: Optimization (Weeks 7-12)
- Fine-tune successful strategies based on results
- Consider advanced interventions if needed
- Establish sustainable long-term routines
- Monitor for seasonal or life changes affecting patterns
Phase 4: Maintenance (Ongoing)
- Continue successful interventions consistently
- Periodic reassessment of effectiveness
- Adapt strategies for changing health needs
- Share successful strategies with healthcare team
Daily Dawn Phenomenon Management Checklist:
- ✓ Maintain consistent sleep schedule (bed by 11 PM, wake at same time daily)
- ✓ Finish eating at least 3 hours before bedtime
- ✓ Include light evening physical activity (10-15 minute walk after dinner)
- ✓ Check blood sugar at consistent times and record patterns
- ✓ Practice stress reduction techniques, especially in evening
- ✓ Take medications at prescribed times without skipping doses
- ✓ Stay hydrated throughout the day but limit fluids before bed
The key to long-term success lies in understanding that dawn phenomenon management is not a one-size-fits-all approach. What works for one person may need significant modification for another based on their diabetes type, duration, current medications, lifestyle factors, and individual hormone patterns.
“The goal isn’t to eliminate dawn phenomenon entirely—it’s to reduce its impact to manageable levels that don’t compromise your overall glucose control or quality of life.”
Remember that dawn phenomenon is fundamentally your body’s attempt to prepare you for the day ahead. By working with these natural processes rather than fighting against them, you can achieve better glucose control while maintaining the energy and alertness you need for daily activities.
References
- Cleveland Clinic. Dawn Phenomenon: What It Is, Causes, Symptoms & Treatment. Cleveland Clinic Medical Professional. 2025.
- Schmidt FH, Pilkington TRE. Dawn Phenomenon. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 May.
- American Diabetes Association. High Morning Blood Glucose. Diabetes.org Patient Resources. 2024.
- Wikipedia Contributors. Dawn phenomenon. Wikipedia, The Free Encyclopedia. 2025.
- Virta Health. The Dawn Phenomenon: Why is my blood sugar high in the morning? Virta Health Blog. 2024.
- WebMD. Dawn Phenomenon vs. Somogyi Effect: Diabetes Morning Highs. WebMD Medical Reference. 2024.
- Mayo Clinic. The dawn phenomenon: What can you do? Mayo Foundation for Medical Education and Research. 2022.
- ScienceDirect. Dawn Phenomenon – an overview. ScienceDirect Topics. 2024.
- Healthline. Dawn Phenomenon: What It Means for People with Diabetes. Healthline Media. 2021.
- Diabetes.co.uk. Dawn Phenomenon (Liver Dump) – Causes & Treatment. Diabetes Digital Media. 2023.
Medical Disclaimer
The information provided in this article is for educational purposes only and should not be considered as medical advice. Always consult with a qualified healthcare professional before making any changes to your diabetes management plan. Dawn phenomenon management may require medication adjustments that should only be made under medical supervision. Individual results may vary, and what works for one person may not be appropriate for another. If you experience consistently high morning blood sugar readings or symptoms of diabetic ketoacidosis, seek immediate medical attention. This content is not intended to diagnose, treat, cure, or prevent any disease.