Introduction
You’re here because you’re worried about antibiotic resistance, dealing with medication side effects, or searching for complementary support for a minor infection. The real question isn’t whether natural antimicrobial compounds exist—they do, and research backs it up. What matters is which ones actually work, how to use them safely, and when you absolutely need prescription antibiotics instead.
Here’s the reality: the clinical literature on natural antibiotics is mixed. Garlic (allicin), raw honey (hydrogen peroxide), and oregano oil (carvacrol) show genuine antimicrobial activity in peer-reviewed studies. Others? Overhyped or barely studied. This guide cuts through the noise with evidence-based analysis of 12 natural antibiotics—including specific dosing protocols, quality sourcing criteria, and clear safety boundaries that most articles completely skip.
You’ll learn which natural antibiotics work for specific infections, how to prepare them correctly (it matters more than you’d think), and exactly when to see a doctor instead. Bottom line: Natural options can complement medical care when used responsibly, but they can’t replace prescription antibiotics for serious bacterial infections. Let’s dig into what the research actually supports.
Quick Start Guide: What to Try First
If you have a minor infection right now:
- Check these red flags first—if ANY apply, see a doctor today (not tomorrow):
- Fever above 101°F (38.3°C) for more than 48 hours
- Rapidly spreading redness or red streaks from a wound
- Difficulty breathing, chest pain, or confusion
- Severe pain that’s getting worse despite home treatment
- Facial swelling, difficulty swallowing, or swelling near your eye
- For respiratory infections (sore throat, congestion, cough): Start with raw garlic—2-3 crushed cloves daily—or raw honey at 1 tablespoon three times daily. Important: crush garlic and wait 10 minutes before eating it.
- For minor cuts or skin wounds: Clean thoroughly first. Then apply raw honey (Manuka UMF 10+ if you can get it) directly to the wound. Cover with a sterile bandage and change it daily.
- For suspected food poisoning (diarrhea, nausea without vomiting blood): Try oregano oil capsules at 150-300mg twice daily, but no more than 5 days total. Always take with food.
- Track improvement: You should see some progress within 3-5 days. No improvement or things getting worse? Stop and see your doctor.
Not sure what you have? Skip to the comparison table to match your symptoms with the right natural antibiotic.
• Fever above 103°F (39.4°C)
• Infection spreading rapidly (redness expanding hourly)
• You’re pregnant, immunocompromised, or have diabetes
• Difficulty breathing or swallowing
• Pain is severe or getting worse despite treatment
• Any infant under 3 months with fever above 100.4°F (38°C)In these situations, natural antibiotics cannot help—go to urgent care or the emergency room today.
What Are Natural Antibiotics and Do They Actually Work?

Natural antibiotics are plant extracts, foods, and compounds with antibacterial properties backed by scientific research. Studies show that substances like garlic (allicin), honey (hydrogen peroxide), and oregano oil (carvacrol) fight certain bacteria effectively. They work as complementary antimicrobial agents—but here’s the critical part: they can’t replace prescription antibiotics for serious infections. Always coordinate use with your healthcare provider.
When we talk about “antibiotics,” we mean substances that kill or inhibit bacterial growth. Sure, pharmaceutical antibiotics dominate modern medicine (and for good reason). But certain natural compounds demonstrate genuine antibacterial activity in controlled studies. Think of these herbal antibiotics and antimicrobial foods as tools for minor infections and prevention—they’re not emergency interventions.
The evidence quality varies significantly. Garlic? It’s got robust support from randomized controlled trials and meta-analyses showing effectiveness against antibiotic-resistant bacteria. Honey’s wound-healing properties show up in clinical practice guidelines. Oregano oil demonstrates strong antibacterial properties in lab studies but needs more human trials. The antimicrobial mechanisms differ too: some disrupt bacterial cell membranes, others mess with bacterial DNA, and some create pH environments where bacteria can’t survive.
Bottom line: Natural antibiotics with antibacterial and antimicrobial properties work for minor bacterial infections and immune support when you use them correctly under medical guidance. They excel at prevention and as home remedies for infections. But for serious stuff—pneumonia, sepsis, kidney infections—prescription antibiotics remain absolutely essential.
The Most Studied Natural Antibiotics: Mechanisms and Evidence
The following 12 natural antibiotics represent compounds with the strongest research backing. Each includes the active antimicrobial component, evidence quality, and practical considerations for safe use.
1. Garlic (Allicin)

Garlic contains organosulfur compounds—primarily allicin—that disrupt bacterial cell membranes and shut down enzymes bacteria need to survive. Here’s the chemistry: when you crush raw garlic and let it sit for 10 minutes, the enzyme alliinase converts alliin into allicin, which is your primary antimicrobial compound.
A 2021 review concluded that garlic’s organosulfur compounds work against a wide variety of bacteria, including multi-drug resistant strains. Fresh garlic extract has shown activity against MRSA (methicillin-resistant Staphylococcus aureus), E. coli, and Salmonella in controlled studies. That’s not marketing hype—it’s peer-reviewed research.
Best for: Respiratory infections, digestive pathogens, cardiovascular support with antimicrobial benefits.
Forms and dosing: Raw crushed garlic (2-4 cloves daily), aged garlic extract (600-1,200 mg daily), or garlic oil capsules. Raw preparations give you the highest allicin content—but only if you prepare them correctly.
Safety notes: Garlic can increase bleeding risk when you combine it with anticoagulant medications like warfarin. If you’re scheduled for surgery, stop garlic supplements 7-10 days beforehand. Start with lower doses to assess tolerance since some people get digestive upset or, well, noticeable body odor.
2. Raw Honey (Especially Manuka)

Honey’s antimicrobial power comes from multiple mechanisms: hydrogen peroxide production, low pH (typically 3.2-4.5), high osmotic pressure, and—in medical-grade Manuka honey—methylglyoxal (MGO). Together, these create an environment where bacteria simply can’t survive or replicate.
Ancient cultures used honey for wound care, and here’s the thing: modern research validates this practice. A 2021 review notes that honey contains antibacterial compounds and could serve as an alternative antibacterial agent with real therapeutic potential. Medical-grade Manuka honey now appears in hospital wound care protocols. That’s a long way from “folk remedy.”
Best for: Wound healing, burn treatment, throat infections, digestive support. Topical applications show the strongest evidence.
Forms and dosing: Medical-grade Manuka honey with a UMF (Unique Manuka Factor) rating of 10+ for wounds; raw, unprocessed honey for internal use (1 tablespoon as needed). Apply directly to clean wounds or take it internally for throat and digestive support.
Safety notes: Never give honey to infants under 12 months—botulism risk from dormant Clostridium botulinum spores. Their immature digestive systems can’t neutralize these spores. For topical use, make sure wounds are clean before application. If you’re diabetic, monitor blood sugar when using honey internally since it does contain glucose.
3. Oregano Oil (Carvacrol)

Oregano essential oil contains carvacrol and thymol—phenolic compounds that disrupt bacterial cell membranes and prevent biofilm formation. Carvacrol specifically damages the outer membrane of bacteria, causing cell contents to leak out and bacteria to die. It’s powerful stuff.
A 2022 review notes that oregano oil’s antimicrobial effect likely comes from carvacrol’s ability to penetrate bacterial cell walls. A 2023 study highlights that oregano oil might work as a potential antibacterial agent against Streptococcus mutans—the primary bacteria responsible for dental cavities.
Best for: Food-borne pathogens (E. coli, Salmonella), respiratory infections, sinus congestion, digestive infections.
Forms and dosing: Essential oil capsules (150-600 mg daily for short-term use, typically 2 weeks maximum), diluted essential oil for topical use (1-2 drops per teaspoon carrier oil), or fresh/dried oregano in cooking. Never ingest undiluted essential oil—seriously, don’t.
Safety notes: Oregano oil is potent, which is why time-limited trials only. Prolonged use may disrupt beneficial gut bacteria. Don’t use it undiluted on skin (chemical burns are no joke). Avoid during pregnancy. People with high blood pressure or hyperthyroid conditions should talk to their clinician before using oregano oil.
4. Ginger (Gingerol)
Ginger’s antimicrobial activity comes from gingerol and related compounds that inhibit bacterial growth and reduce inflammation. These bioactive compounds interfere with bacterial communication systems and protein synthesis.

The scientific community recognizes ginger as a natural antibiotic. A 2022 study suggests that ginger could effectively inhibit various bacteria, including Streptococcus mutans, Enterococcus faecalis, Staphylococcus species, and Lactobacillus species. Beyond antimicrobial effects, ginger offers antioxidant and anti-inflammatory benefits.
Best for: Oral infections, respiratory support, digestive bacteria, nausea with antimicrobial needs.
Forms and dosing: Fresh ginger root (1-2 inches daily, grated into tea or food), dried ginger powder (1-3 grams daily), or standardized extract (250 mg 2-3 times daily). Fresh preparations offer the most gingerol.
Safety notes: Generally well-tolerated. High doses (>5 grams daily) may cause digestive upset or interact with blood thinners. If you’re taking anticoagulant medications, coordinate ginger supplementation with your clinician.
5. Echinacea
Echinacea stimulates immune response while also exerting direct antibacterial effects on respiratory pathogens. The plant’s polysaccharides and alkamides enhance white blood cell activity and inhibit bacterial enzyme systems.
Native American and traditional healers used echinacea for centuries to treat infections and wounds. A 2022 article notes that echinacea has an antibacterial effect on respiratory bacteria. Studies also suggest it may possess antiviral properties and could help treat respiratory tract infections in both children and adults.
Best for: Upper respiratory infections (prevention and early intervention), wound healing, immune support during infection risk periods.
Forms and dosing: Tincture (2-3 mL three times daily), tea (1-2 cups daily), or capsules (300-500 mg three times daily). Most research uses Echinacea purpurea or Echinacea angustifolia species.
Safety notes: Take during acute illness or high-risk periods only—continuous use may reduce effectiveness. People with autoimmune conditions should avoid echinacea, as immune stimulation could worsen symptoms. Allergic reactions are possible in those sensitive to plants in the daisy family.
6. Thyme Essential Oil (Thymol)
Thyme essential oil contains thymol and carvacrol—phenolic compounds that disrupt bacterial cell walls and interfere with bacterial metabolism. Thymol specifically targets the lipid membrane of bacteria, causing structural damage and death.
Research shows thyme essential oil is especially helpful against antibiotic-resistant bacteria. A 2011 study tested both lavender and thyme essential oils against over 120 strains of bacteria. Researchers found thyme essential oil to be more effective at killing bacteria than lavender essential oil.
Best for: Antibiotic-resistant bacterial strains, topical wound care, respiratory infections when diffused.
Forms and dosing: Essential oil for topical use only (1-2 drops per teaspoon carrier oil like coconut or olive oil), diffused for respiratory support, or culinary thyme in cooking. Never take thyme essential oil internally.
Safety notes: Thyme essential oil is for external use only. Do not ingest. Always dilute before skin application—undiluted oil causes irritation and potential chemical burns. People with high blood pressure or hyperthyroid conditions should avoid thyme essential oil. Test a small area first to check for sensitivity.
7. Clove (Eugenol)
Clove’s antimicrobial power comes from eugenol, a phenolic compound that damages bacterial cell membranes and disrupts protein function. Eugenol also exhibits anesthetic properties, which explains clove’s traditional use for toothache relief.
A 2023 study notes that clove essential oil may possess a strong inhibitory effect against Staphylococcus aureus. Similarly, a 2020 article notes that clove extract may have potential as a new antibacterial agent, particularly for oral pathogens.
Best for: Dental infections, oral bacteria, toothaches with antibacterial needs, topical wound care.
Forms and dosing: Whole cloves (chew 1-2 for dental pain), clove essential oil diluted (1 drop in carrier oil for topical use), clove water extract, or culinary use in cooking. For dental applications, place a whole clove near the affected tooth.
Safety notes: Undiluted clove oil can cause burns and tissue damage—always dilute for topical use. Ingesting large amounts of clove oil can cause liver damage, vomiting, and breathing difficulties. Use small amounts and coordinate with your dentist for dental infections, as abscesses require professional drainage.
8. Apple Cider Vinegar (Acetic Acid)
Apple cider vinegar’s antimicrobial properties stem from acetic acid, which creates a low pH environment hostile to bacterial growth. The “mother” (cloudy strands) in raw, unfiltered versions contains beneficial enzymes and probiotics.
ACV has been used for centuries as a natural antibiotic and antiseptic. Research on modern applications remains limited compared to other natural antibiotics, but in vitro studies show antibacterial activity against common pathogens. Traditional use focused on topical disinfection and digestive support.
Best for: Topical wound disinfection, skin infections, digestive support (anecdotal), UTI prevention (limited evidence).
Forms and dosing: Raw, unfiltered apple cider vinegar with “the mother” (1-2 tablespoons diluted in 8 oz water daily), topical application for skin issues (dilute 1:1 with water). Always dilute—never apply or consume undiluted.
Safety notes: Undiluted ACV can erode tooth enamel and burn esophageal tissue. Always dilute and consider drinking through a straw. If you have gastroparesis or take medications that slow gastric emptying, discuss ACV with your clinician first, as it may worsen symptoms. May interact with insulin and diuretic medications.
9. Turmeric (Curcumin)
Turmeric’s active compound curcumin offers both antimicrobial and anti-inflammatory properties. Curcumin disrupts bacterial cell membranes and interferes with bacterial protein synthesis. Its anti-inflammatory effects help reduce infection-related tissue damage.
Multiple studies examine turmeric’s role in wound healing and skin infections. The combination of antimicrobial activity and inflammation reduction makes turmeric valuable for infections accompanied by swelling and pain. Curcumin’s poor bioavailability improves significantly when combined with black pepper (piperine).
Best for: Skin infections, wound healing, anti-inflammatory support during infections, digestive antimicrobial needs.
Forms and dosing: Fresh turmeric root (1-3 grams daily), turmeric powder (1-3 grams daily), or curcumin extract (500-2,000 mg daily with black pepper or piperine). Topical paste can be applied to skin infections.
Safety notes: High doses may cause digestive upset. Turmeric can interact with blood thinners and diabetes medications. The active compound curcumin is fat-soluble, so consume with healthy fats for better absorption. Always combine with black pepper (increases absorption by up to 2,000%).
10. Myrrh Oil
Myrrh contains terpenoids and sesquiterpenes that exhibit antimicrobial properties. Uniquely, research suggests myrrh oil preferentially kills non-growing bacteria—the dormant forms that often resist conventional antibiotics.
A 2020 in vitro study found that myrrh oil preferentially kills non-growing bacteria without the organisms building resistance. Typically, non-growing bacteria tend to be more antibiotic-resistant than actively growing bacteria, making myrrh’s mechanism particularly interesting for persistent infections.
Best for: Persistent infections, oral health, potential against antibiotic-resistant strains (preliminary research).
Forms and dosing: Myrrh essential oil (follow product instructions, typically diluted for topical use), myrrh tincture, or myrrh-containing mouthwash products. Myrrh is typically sold pre-packaged—follow label dosing.
Safety notes: Myrrh is generally well-tolerated but may cause diarrhea when ingested. Topical application can cause minor skin rash in sensitive individuals. Large doses may affect heart function—stick to recommended amounts. Avoid during pregnancy.
11. Goldenseal (Berberine)
Goldenseal contains berberine, an alkaloid that disrupts bacterial DNA replication and interferes with bacterial attachment to tissues. Berberine also demonstrates activity against fungi and some parasites beyond its antibacterial effects.
Berberine has strong research backing. Studies compare its metabolic effects to metformin, and it shows broad-spectrum antimicrobial activity. Berberine works particularly well for digestive infections because it concentrates in the intestinal tract after oral consumption.
Best for: Digestive infections, UTI prevention, immune support, metabolic health with antimicrobial needs.
Forms and dosing: Goldenseal root capsules (500-1,000 mg up to three times daily for short-term use), berberine extract (500 mg 2-3 times daily), or tincture. Use time-limited trials (2-3 weeks maximum).
Safety notes: Berberine can interact with medications metabolized by CYP enzymes and P-glycoprotein—review your medication list with your clinician before starting. May lower blood sugar, so coordinate with diabetes medications. Avoid during pregnancy and breastfeeding. Long-term use may disrupt beneficial gut bacteria.
12. Pau d’Arco (Lapachol)
Pau d’Arco contains naphthoquinones—particularly lapachol—that inhibit bacterial and fungal enzyme systems. Traditional use in South American medicine focused on infections and immune support, with modern research beginning to validate some applications.
Research on Pau d’Arco remains less robust than top-tier natural antibiotics, but preliminary studies and traditional use patterns suggest antimicrobial and antifungal activity. It appears particularly useful for Candida overgrowth and fungal infections.
Best for: Fungal infections (Candida), immune support, potential antibacterial effects (emerging research).
Forms and dosing: Pau d’Arco tea (2-3 cups daily), capsules (500-1,000 mg 2-3 times daily), or tincture. Inner bark preparations are standard. Use time-limited trials.
Safety notes: High doses may cause nausea, vomiting, or bleeding issues due to anticoagulant effects. Avoid during pregnancy or if taking blood thinners. Quality varies significantly among products—choose reputable brands with third-party testing.
Matching Natural Antibiotics to Specific Infections
Choosing the right natural antibiotic depends on the type of infection, location, and severity. This comparison table maps natural antibiotics to common conditions based on research evidence and traditional use patterns.
Use this as a starting point for discussions with your clinician, not as a substitute for professional diagnosis. Serious infections require medical evaluation regardless of natural options you’re considering.
| Natural Antibiotic | Best For | Evidence Level | Typical Dose | Key Safety Notes |
|---|---|---|---|---|
| Garlic | Respiratory infections, MRSA, E. coli, cardiovascular support | Strong (RCTs, meta-analyses) | 2-4 raw cloves/day or 600-1,200 mg extract | Blood thinner interaction; stop before surgery |
| Manuka Honey | Wound healing, burns, throat infections, topical skin infections | Strong (clinical use, RCTs) | Topical application or 1 tbsp internal | Never for infants <1 year; monitor blood sugar |
| Oregano Oil | Food-borne pathogens, respiratory infections, sinus issues | Moderate (in vitro, small trials) | 150-600 mg/day for max 2 weeks | Short-term use only; dilute for topical |
| Ginger | Oral bacteria, respiratory support, digestive infections | Moderate (in vitro, small trials) | 1-3 grams fresh/dried daily | May interact with blood thinners |
| Echinacea | Upper respiratory infections, wound healing, immune support | Moderate (mixed trial results) | 300-500 mg 3x/day during acute illness | Avoid with autoimmune conditions |
| Thyme Oil | Antibiotic-resistant bacteria, topical wounds, respiratory (diffused) | Moderate (in vitro strong) | Diluted topical only; diffuse for respiratory | Never ingest; dilute before skin use |
| Clove | Dental infections, oral bacteria, toothaches | Moderate (in vitro, traditional use) | 1-2 whole cloves or diluted oil topically | Undiluted oil causes burns; liver toxicity risk |
| Apple Cider Vinegar | Topical disinfection, skin infections, digestive support | Limited (traditional use, in vitro) | 1-2 tbsp in 8 oz water; 1:1 dilution topical | Erodes enamel; burns if undiluted |
| Turmeric | Skin infections, wound healing, anti-inflammatory support | Moderate (multiple mechanisms) | 1-3 grams with black pepper daily | Blood thinner interaction; take with fat |
| Myrrh Oil | Persistent infections, oral health, resistant strains | Limited (promising in vitro) | Follow product instructions; diluted topical | May cause GI upset; avoid in pregnancy |
| Goldenseal/Berberine | Digestive infections, UTI prevention, metabolic support | Strong (for berberine metabolic effects) | 500 mg 2-3x/day for 2-3 weeks max | CYP enzyme interactions; lowers blood sugar |
| Pau d’Arco | Fungal infections (Candida), immune support | Limited (traditional use) | 500-1,000 mg 2-3x/day or tea | Anticoagulant effects; avoid in pregnancy |
Evidence levels explained:
- Strong: Multiple RCTs, meta-analyses, or clinical use guidelines support effectiveness
- Moderate: Some controlled trials, strong in vitro data, or consistent traditional use with emerging research
- Limited: Primarily traditional use, preliminary research, or strong in vitro data awaiting human trials
Using this table: Start with options that have stronger evidence for your specific condition. Introduce one natural antibiotic at a time, monitor for effects and side effects, and coordinate with your clinician—especially if you take medications or have chronic conditions. Time-limited trials (2-4 weeks) with clear stop criteria prevent indefinite use without benefit.
Quick Reference – Start Here:
- Respiratory infection: Garlic (2-3 cloves daily) or raw honey (1 tbsp 3x daily)
- Minor wound: Medical-grade Manuka honey (UMF 10+) applied topically
- Food poisoning: Oregano oil (150-300mg twice daily, max 5 days)
- Oral/tooth pain: Clove oil diluted or whole clove placed near tooth
- Prevention during cold season: Garlic or echinacea (rotate every 8 weeks)
Using Natural Antibiotics Safely: Risks and Red Flags
Natural compounds can cause real harm when you use them incorrectly or combine them inappropriately with medications. Because these substances influence biological systems, they carry interaction risks, contraindications, and potential for adverse effects—particularly when you layer them with prescription drugs or use them in vulnerable populations.
Medication Interactions That Matter
The most significant risks happen when natural antibiotics amplify or interfere with prescription medications. These interactions work through several mechanisms: enzyme inhibition, protein binding competition, or additive pharmacological effects. Let’s get specific.
Garlic and anticoagulants: Garlic inhibits platelet aggregation through multiple pathways. When combined with warfarin, clopidogrel, or aspirin, bleeding risk increases measurably. If you’re scheduled for surgery, discontinue garlic supplements 7-10 days beforehand to restore normal clotting function. Food amounts in cooking (1-2 cloves) pose minimal risk, but concentrated extracts require coordination with your prescriber.
Berberine and CYP enzymes: Berberine inhibits cytochrome P450 enzymes (particularly CYP3A4 and CYP2D6) and P-glycoprotein transport. Because of that, medications metabolized by these pathways—including statins, calcium channel blockers, and many antidepressants—may reach higher blood levels than intended. Start berberine at lower doses if you take multiple medications, and discuss timing strategies with your clinician to minimize overlap.
Natural antibiotics and diabetes medications: Garlic, berberine, bitter melon, and cinnamon can all lower blood glucose. When you combine them with insulin or sulfonylureas (glyburide, glipizide), hypoglycemia risk increases significantly. Check blood sugar more frequently for the first 7-10 days after introducing any glucose-lowering natural compound. Keep fast-acting carbohydrates (glucose tablets, juice) accessible, and coordinate dosing adjustments with your clinician.
Oregano/thyme oil and blood pressure medications: Both oregano and thyme essential oils may lower blood pressure. If you take antihypertensive medications, introducing these oils could cause excessive blood pressure reduction. Monitor readings during the first week and report dizziness, lightheadedness, or unusual fatigue to your clinician.
Essential Oil Safety Protocols
Essential oils are concentrated plant compounds—typically 50-100 times more potent than the dried herb. This concentration delivers therapeutic effects but also increases toxicity risk when used improperly.
Dilution ratios that matter: For topical use, the standard safe dilution is 1-2 drops of essential oil per teaspoon (5 mL) of carrier oil. This creates approximately a 1-2% dilution—sufficient for antimicrobial effects without causing chemical burns. Carrier oils include coconut oil, olive oil, jojoba oil, or sweet almond oil. Never apply undiluted essential oils to skin, as they can cause second-degree burns, blistering, and permanent sensitization.
Internal use restrictions: Oregano and thyme essential oils should never be ingested. Even small amounts can cause severe mucous membrane irritation, liver toxicity, and central nervous system effects. If a natural health practitioner recommends internal essential oil use, seek a second opinion from a licensed physician or pharmacist. Food-grade herbs (dried oregano, thyme) offer antimicrobial benefits without the toxicity risks of concentrated oils.
Inhalation versus topical: Diffusing essential oils for respiratory support poses lower risk than topical or internal use, but prolonged exposure in poorly ventilated spaces can trigger headaches, dizziness, or respiratory irritation. Diffuse for 15-30 minute intervals with breaks, and ensure adequate ventilation.
Clear Stop Criteria and Medical Intervention Thresholds
Natural antibiotics work slowly—typically 3-5 days for minor infections. However, certain signs indicate infection severity that requires prescription antibiotics and professional care. Delaying appropriate treatment can lead to serious complications including sepsis, organ damage, or death.
Temperature thresholds: Fever above 101°F (38.3°C) lasting more than 48 hours suggests bacterial infection requiring medical evaluation. Fever above 103°F (39.4°C) at any point warrants same-day assessment. In infants under 3 months, any fever above 100.4°F (38°C) is a medical emergency.
Visual infection markers: Spreading redness beyond the initial infection site, red streaks extending from a wound, increasing swelling despite treatment, or pus with foul odor all indicate advancing infection. These signs suggest bacteria are overwhelming your immune response and natural interventions.
Systemic symptoms: Confusion, extreme fatigue, rapid heartbeat (>100 beats per minute at rest), rapid breathing (>20 breaths per minute), chills with shaking, or decreased urine output suggest sepsis—a life-threatening condition requiring emergency care. Do not attempt to treat these symptoms with natural antibiotics; call 911 or go to the emergency department immediately.
Timeline benchmarks: For minor infections treated with natural antibiotics, you should see improvement within 3-5 days. No improvement by day 5, or worsening at any point, requires medical reevaluation. “Improvement” means reduced pain, decreased redness/swelling, less drainage, or improved energy—not just stable symptoms.
Specific condition red flags:
- Urinary tract infections: Blood in urine, back/flank pain, fever, or vomiting require same-day medical evaluation—UTIs can progress to kidney infections rapidly
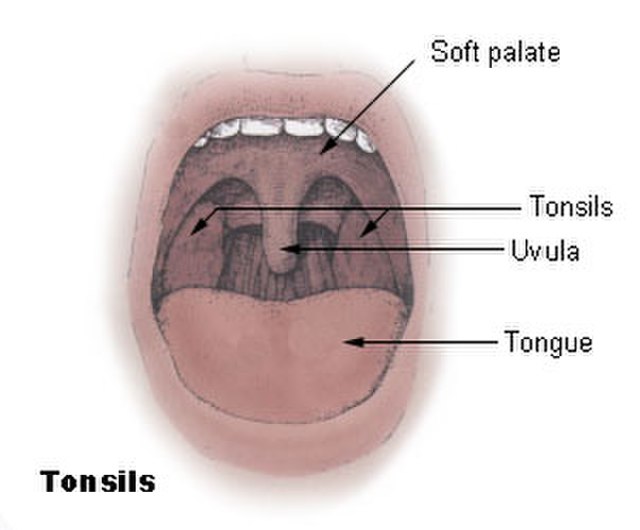
- Dental infections: Facial swelling, difficulty swallowing, fever, or swelling spreading to the eye area need emergency dental evaluation—dental abscesses can spread to the brain
- Respiratory infections: Difficulty breathing, chest pain, coughing up blood, confusion, or blue-tinged lips require emergency care—these suggest pneumonia or other serious conditions
- Skin infections: Rapidly spreading redness (progressing hourly), black/purple discoloration, severe pain disproportionate to appearance, or blistering could indicate necrotizing fasciitis—a surgical emergency
Special Populations and Adjusted Protocols
Certain groups face higher risks from natural antibiotics or require modified approaches due to physiology, metabolism, or underlying conditions.
Pregnancy and lactation: Most herbal antimicrobials lack safety data in pregnancy. Hormonal changes, increased blood volume, and altered drug metabolism make pregnant women more susceptible to both infections and adverse effects. Food amounts of garlic, ginger, and honey are generally safe, but concentrated extracts and essential oils should be avoided. Coordinate any supplementation with your obstetrician, as even “natural” compounds cross the placenta and enter breast milk.
Infants and children: Children metabolize drugs differently than adults, and dosing cannot simply be scaled by weight. Never give honey to infants under 12 months due to botulism risk—their immature digestive systems cannot neutralize dormant Clostridium botulinum spores. Essential oils pose higher toxicity risks in children due to smaller body size and developing organ systems. Coordinate any natural antibiotic use in children with their pediatrician, and start with the lowest effective dose.
Kidney disease: Your kidneys filter and eliminate many plant compounds. Impaired kidney function allows these substances to accumulate to toxic levels. If you have chronic kidney disease (CKD stage 3 or higher), creatinine above 1.5 mg/dL, or history of kidney stones, discuss natural antibiotics with your nephrologist before use. Avoid combining multiple supplements, as the cumulative kidney burden increases disproportionately.
Liver disease: The liver metabolizes most herbal compounds. Cirrhosis, hepatitis, or elevated liver enzymes (ALT, AST) indicate reduced metabolic capacity. High-dose cinnamon (cassia variety), pau d’arco, and concentrated garlic supplements can stress the liver further. If you have liver disease, coordinate natural antibiotic use with your hepatologist and monitor liver enzymes more frequently during trials.
Autoimmune conditions: Echinacea and other immune-stimulating compounds can worsen autoimmune diseases by increasing immune system activity. If you have rheumatoid arthritis, lupus, multiple sclerosis, or inflammatory bowel disease, avoid immune-boosting natural antibiotics. Focus instead on compounds with antimicrobial effects but neutral immune impact, like honey or diluted oregano oil for specific infections.
Gastroparesis: Apple cider vinegar and any substance that delays gastric emptying can worsen gastroparesis symptoms. If you take GLP-1 medications (semaglutide, liraglutide), have diabetes with documented slow gastric emptying, or experience early satiety with small meals, discuss vinegar-based remedies with your clinician before use.
Quality Matters: Third-Party Testing and Batch Verification
Natural product quality varies dramatically between brands. Unlike prescription medications, supplements face minimal FDA oversight before market entry. Contaminants, incorrect dosing, and adulterated products appear regularly in independent testing.
Third-party certification to trust: Look for USP Verified, NSF Certified for Sport, or Informed Choice seals on product labels. These programs conduct independent testing for contaminant presence, ingredient accuracy, and proper manufacturing practices. Products without third-party verification rely solely on manufacturer claims—which independent testing shows are frequently inaccurate.
Batch-level testing: Some premium brands publish batch-specific test results online, showing heavy metal levels, microbial contamination, and active ingredient concentrations for each production run. This transparency allows you to verify exactly what you’re consuming. Brands that refuse to share batch data raise red flags about quality control practices.
Watch for proprietary blends: Labels listing “proprietary blend” without individual ingredient amounts prevent you from knowing actual doses. This obscurity makes it impossible to match research-based dosing or identify which ingredient caused adverse effects. Choose products with transparent labeling showing exact amounts of each compound.
How to Choose and Prepare Natural Antibiotics for Best Results
Here’s something most people don’t realize: the form, preparation, and storage of natural antibiotics dramatically impact their antimicrobial potency. Active compounds degrade with heat, light, oxygen exposure, and time. Understanding these factors helps you maximize effectiveness and avoid throwing money at inactive products.
Quality Markers and Form Selection
Not all garlic supplements contain allicin. Not all honey fights bacteria. The processing method, storage conditions, and source material determine whether a natural antibiotic retains therapeutic activity. Let’s break down what actually matters.
Garlic: Activation chemistry matters: Intact garlic cloves contain alliin, not allicin. When you crush or chew garlic, the enzyme alliinase converts alliin into allicin—the compound with antimicrobial properties. This conversion requires 10 minutes of exposure to air at room temperature. Because of that, swallowing whole cloves or immediately cooking crushed garlic prevents allicin formation.
Aged garlic extract (AGE) uses a different mechanism—long fermentation converts harsh compounds into stable, bioavailable organosulfur derivatives. AGE lacks the sharp garlic odor and causes less digestive upset, making it better tolerated for daily use. However, fresh crushed garlic provides higher peak allicin levels for acute infections.
Garlic powder and many supplements are processed at high heat, denaturing alliinase and preventing allicin formation. Check for “allicin potential” or “allicin yield” on supplement labels—this indicates the product can generate allicin in your digestive tract. Look for enteric-coated formulations that protect the tablet until it reaches your intestines, where pH conditions favor allicin formation.
Honey: Medical-grade versus table honey: Standard honey from grocery stores undergoes pasteurization (heat treatment) and filtration that remove pollen, enzymes, and some antimicrobial compounds. While still containing some hydrogen peroxide activity, processed honey has significantly lower antibacterial potency than raw varieties.
Medical-grade Manuka honey from New Zealand contains methylglyoxal (MGO) alongside hydrogen peroxide—offering dual antimicrobial mechanisms. The UMF (Unique Manuka Factor) rating indicates methylglyoxal concentration: UMF 10+ (minimum for therapeutic use), UMF 15+ (moderate infections), UMF 20+ (severe wounds). Higher UMF ratings cost more but deliver stronger antimicrobial effects. Verify UMF ratings through the official UMF Honey Association database to avoid counterfeit products.
For internal use, raw local honey offers antimicrobial benefits plus possible allergy relief through local pollen exposure. Choose opaque or amber glass jars over plastic, as light exposure degrades hydrogen peroxide activity over time.
Oregano oil: CO2 extraction versus steam distillation: Steam-distilled oregano oil is standard but exposes compounds to high heat, partially degrading carvacrol. CO2 extraction uses pressure instead of heat, preserving more carvacrol and related phenols. Check labels for “supercritical CO2 extracted” if you want maximum potency—these products cost more but deliver higher antimicrobial activity per dose.
Many oregano oil products are diluted before encapsulation. Look for “standardized to X% carvacrol” (typically 55-85% for quality products). Lower carvacrol percentages suggest dilution with carrier oils or use of low-quality source material.
Essential oils: Organic and GC/MS tested: Pesticide residues concentrate during essential oil production—1,000 pounds of plant material might yield 1 pound of oil. Because of that, conventional (non-organic) essential oils can contain concentrated pesticides at levels that cause toxicity. Choose certified organic essential oils for any product you’ll apply to skin or diffuse regularly.
Gas chromatography/mass spectrometry (GC/MS) testing identifies the chemical compounds present in essential oils and detects adulteration with synthetic fragrance chemicals. Reputable brands include GC/MS reports with each batch. If a brand markets “therapeutic grade” without GC/MS data, they’re using meaningless marketing language rather than verified quality standards.
Activation and Preparation Protocols
Certain preparation steps unlock antimicrobial activity, while others destroy it. These protocols are based on the chemistry of active compounds and how they behave under different conditions.
Garlic Activation Protocol
If you must cook with garlic, crush it first, wait 10 minutes to allow allicin formation, then add it during the final minutes of cooking to minimize heat exposure. Microwaving garlic before the 10-minute waiting period completely destroys antimicrobial activity.
Turmeric bioavailability enhancement: Curcumin, turmeric’s active compound, has notoriously poor absorption—your body absorbs less than 1% of consumed curcumin without enhancement strategies. Two proven enhancement methods increase absorption dramatically:
- Combine with black pepper: Piperine in black pepper inhibits enzymes that metabolize curcumin, increasing bioavailability up to 2,000%. Use ¼ teaspoon black pepper per 1 teaspoon turmeric powder. Most quality curcumin supplements include piperine (look for “with BioPerine”).
- Consume with fat: Curcumin is fat-soluble. Taking turmeric with coconut oil, olive oil, avocado, nuts, or a fatty meal improves absorption significantly. Some supplement formulations include curcumin bound to phospholipids (like Meriva) for enhanced absorption without requiring added fat.
For topical applications (wound paste), mix turmeric powder with raw honey—both contribute antimicrobial effects, and honey serves as a sticky carrier keeping turmeric in contact with the infection site.
Essential oil dilution formulas: The standard safe dilution for adult topical use is 1-2% concentration. Here’s how to calculate:
- 1% dilution: 6 drops essential oil per 1 oz (30 mL) carrier oil
- 2% dilution: 12 drops essential oil per 1 oz (30 mL) carrier oil
For children ages 6-12, use 0.5-1% dilution (3-6 drops per oz). For children ages 2-6, use 0.25% dilution (1.5 drops per oz). Never use essential oils topically on infants under 2 years old.
To dilute for immediate use, add 1-2 drops of oregano or thyme oil to 1 teaspoon (5 mL) carrier oil in your palm, mix, then apply. This creates approximately 1-2% dilution suitable for localized application to skin infections or wounds.
Honey application technique: For wound care, clean the area with saline or mild soap and water first. Apply a thick layer of honey (1-2 mm thick) directly to the wound bed, then cover with a sterile non-adherent dressing. Change dressings once daily. The honey draws fluid from the wound (osmotic effect) while killing bacteria—you may notice increased drainage initially, which is normal and beneficial.
For throat infections, take 1 tablespoon of raw honey directly, allowing it to coat the throat slowly rather than swallowing immediately. Avoid drinking liquids for 10-15 minutes afterward to maintain honey contact time with throat tissues.
Storage Practices That Preserve Potency
Improper storage accelerates degradation of active compounds, rendering natural antibiotics ineffective within weeks. These storage protocols maintain potency throughout the product’s shelf life.
Essential oils: Store in dark glass bottles (amber or cobalt blue) in a cool location away from direct sunlight. Heat and light degrade aromatic compounds rapidly. Refrigeration extends shelf life but can cause some oils to solidify—allow them to return to room temperature before use.
Once opened, most essential oils maintain potency for 1-2 years if stored properly. Citrus oils (lemon, orange) oxidize faster—use within 6-12 months of opening. If an essential oil smells rancid, musty, or “off,” discard it—oxidized oils can cause skin sensitization even if they didn’t before.
Honey: Never refrigerate honey—cold temperatures promote crystallization without preserving antimicrobial properties. Store at room temperature in a tightly sealed container. Honey is naturally antimicrobial and doesn’t spoil, but exposure to moisture can dilute hydrogen peroxide concentration and allow fermentation.
If honey crystallizes (becomes grainy or solid), this indicates natural glucose crystallization—not spoilage. Gently warm the container in hot water (not boiling) to reliquefy. Avoid microwaving honey, as uneven heating can create hot spots that destroy enzymes.
Dried herbs and powders: Store in airtight containers away from light, heat, and moisture. Glass jars with tight lids work better than plastic, which can allow oxygen penetration over time. Label containers with purchase dates—most dried herbs lose significant potency after 12 months.
Whole herbs (dried leaves, bark) retain potency longer than powdered forms. Grind herbs shortly before use for maximum fresh compound release. If dried herbs lose their characteristic aroma, they’ve likely lost antimicrobial activity too.
Fresh roots (ginger, turmeric): Store unpeeled roots in the refrigerator crisper drawer in a paper bag or wrapped in paper towels. This absorbs excess moisture while preventing dehydration. Fresh ginger lasts 3-4 weeks; turmeric lasts 2-3 weeks. For longer storage, peel and freeze in portion sizes—frozen ginger grates easily while still frozen.
Garlic: Store whole garlic bulbs in a cool, dry, well-ventilated location—not the refrigerator. Cold, humid conditions promote sprouting and mold growth. Once you break the bulb, individual cloves last 7-10 days at room temperature. Peeled garlic cloves deteriorate rapidly—use within 1-2 days or preserve in olive oil (refrigerated, use within 4 days to prevent botulism risk).
Tinctures and liquid extracts: Store in dark glass bottles with tight droppers. Most alcohol-based tinctures remain stable for 3-5 years without refrigeration. Glycerin-based tinctures have shorter shelf life (1-2 years) and benefit from refrigeration after opening. If you see cloudiness, mold, or off-odors, discard the product.
When Fresh Beats Supplements
For some natural antibiotics, fresh forms deliver benefits that capsules and extracts cannot replicate. Understanding when to choose fresh over processed helps you optimize therapeutic results.
Garlic: Fresh crushed garlic provides immediate high-dose allicin unavailable from most supplements. For acute respiratory infections or when you need peak antimicrobial activity, fresh garlic works better than aged extract or powder. However, for daily cardiovascular support with antimicrobial benefits, aged garlic extract offers consistent dosing without odor or digestive upset.
Ginger: Fresh ginger root contains gingerols that convert to shogaols when dried or heated. Shogaols have stronger anti-inflammatory effects, while gingerols offer more direct antimicrobial activity. For fighting active infections, fresh ginger provides more antimicrobial compounds. For inflammation management, dried ginger or standardized extracts work well.
Honey: Always choose raw honey over processed varieties for antimicrobial use. Heat pasteurization destroys enzymes that generate hydrogen peroxide. Filtered honey removes pollen and propolis—compounds that contribute to honey’s antimicrobial complexity. Medical-grade Manuka honey represents the exception where processing maintains antimicrobial standards.
Herbs as food versus concentrated extracts: Adding fresh or dried herbs to cooking (garlic, oregano, thyme, turmeric) provides antimicrobial compounds plus fiber, antioxidants, and flavor complexity that isolated extracts lack. Extracts deliver higher doses for acute infection management, but daily dietary inclusion of herbs offers sustained low-level antimicrobial support that may prevent infections from establishing.
Building Your Personal Natural Antibiotic Protocol: A Data-Driven Framework
Here’s the problem with most natural antibiotic advice: it follows one-size-fits-all recommendations that completely ignore individual biology, medication context, and specific infection types. The reality? What works brilliantly for your neighbor’s sinus infection might do absolutely nothing for your skin wound—or worse, cause adverse effects you didn’t see coming. This framework shows you how to test natural antibiotics systematically, measure results objectively, and build a personalized protocol based on your data rather than generic advice from the internet.
The Time-Boxed Trial Method
Taking supplements indefinitely without measurable benefit wastes money and increases cumulative toxicity risk. The time-boxed trial method prevents this by setting clear start dates, success metrics, and stop criteria before you begin. This approach comes from clinical trial design—where every intervention requires predefined endpoints and decision rules. No guessing, no hoping, just data.
Step 1: Define your specific goal with measurable outcomes. “Boost my immune system” is too vague to track—you can’t measure that. “Reduce frequency of upper respiratory infections from 6 per year to 3 or fewer” gives you a concrete target. “Heal this finger wound within 5 days with no signs of spreading infection” provides daily assessment criteria you can actually see.
For active infections, track pain level (0-10 scale), redness diameter in millimeters, swelling severity, drainage amount and color, and functional impact (can’t type, can’t walk normally, etc.). Take photos daily to document visual changes objectively—our memory distorts perception when we want something to work.
Step 2: Choose one natural antibiotic based on evidence match. Resist the urge to stack multiple supplements immediately. If you combine garlic, oregano oil, echinacea, and elderberry from day one, you can’t identify which compound helped, which did nothing, or which caused that headache on day three.
Match the natural antibiotic to infection location and pathogen type. Garlic for respiratory infections (strong evidence for respiratory pathogens). Honey for skin wounds (clinical validation for topical antimicrobial effects). Oregano oil for suspected food-borne illness (in vitro activity against E. coli and Salmonella). This matching increases your probability of measurable benefit.
Step 3: Set trial duration and stop criteria upfront. Write these down before starting—decision fatigue and optimism bias cloud judgment when you’re three weeks into an expensive supplement that isn’t working.
For acute infections: 5-7 day trial maximum. Improvement should begin within 48-72 hours for topical applications, 3-5 days for internal use. No improvement by day 5 triggers medical consultation, not supplement substitution.
For prevention trials: 8-12 weeks minimum to assess impact on infection frequency. If you normally get 2-3 colds during winter, you need a full cold season to evaluate whether echinacea or garlic supplementation reduced that frequency.
Stop criteria include: adverse effects (rash, digestive upset, headaches), no improvement by predefined timeline, conflicting higher priorities (like needing to start a prescription antibiotic), or achieving your goal (wound healed, infection resolved).
Step 4: Track systematically, review objectively. Use a simple log format:
Natural antibiotic: Garlic (crushed raw) Dose: 3 cloves daily Start date: [Date] Goal: Resolve throat infection within 5 days Stop criteria: Fever >101°F, no improvement by day 5, spreading infection Day 1: Pain 7/10, difficulty swallowing, white patches visible Day 2: Pain 6/10, swallowing slightly easier, white patches unchanged Day 3: Pain 4/10, can eat solid foods again, patches smaller Day 4: Pain 2/10, minimal discomfort, patches mostly resolved Day 5: Pain 1/10, eating normally, no visible infection Decision: Garlic trial successful for this infection type. Will repeat for future throat infections.
This documentation creates your personal evidence base. After 3-5 trials with different natural antibiotics, patterns emerge showing what works consistently for your biology and infection types.
Step 5: Build your personalized stack strategically. Once you’ve identified 2-3 natural antibiotics that deliver measurable benefits in solo trials, you can combine them strategically for enhanced effects—now knowing which compound contributed what.
Combine mechanisms, not redundancy. Garlic (disrupts bacterial membranes) + raw honey (multiple antimicrobial mechanisms including low pH) offers complementary actions. Garlic + aged garlic extract adds expense without different mechanisms. Layer proven options only after individual validation.
Seasonal Rotation Strategy: Preventing Adaptation
Bacteria can develop tolerance to natural antimicrobials when exposed continuously. While slower than antibiotic resistance development, adaptation still occurs. Seasonal rotation prevents this by cycling different compounds every 8-12 weeks, never allowing bacteria to fully adapt.
The rotation framework:
Winter rotation (cold/flu season): Focus on respiratory-supportive natural antibiotics. Weeks 1-8: Garlic (3 cloves daily or 600mg aged extract). Weeks 9-16: Echinacea (300mg three times daily, take only during high-risk periods or early symptoms—not continuously). This rotation matches winter’s higher respiratory infection risk while preventing garlic tolerance.
Spring rotation (allergy season, sinus issues): Shift to anti-inflammatory antimicrobials. Weeks 1-8: Raw local honey (1 tablespoon daily for potential allergy relief plus antimicrobial benefits). Weeks 9-16: Ginger (fresh root tea or 1g daily dried). These address inflammation while maintaining antimicrobial support for sinus infections that often follow allergy flare-ups.
Summer rotation (food safety focus, wounds): Emphasize topical and digestive antimicrobials. Weeks 1-8: Oregano oil capsules (150mg twice daily) during travel or higher food poisoning risk periods. Weeks 9-16: Keep raw honey and diluted essential oils on hand for immediate wound care. Summer’s higher outdoor activity increases wound risk.
Fall rotation (back-to-school, immune preparation): Build immune resilience before winter. Weeks 1-8: Turmeric with black pepper (500mg curcumin with piperine daily for anti-inflammatory immune support). Weeks 9-16: Begin transitioning back to garlic before winter respiratory season peaks.
This rotation accomplishes three goals: maintains year-round antimicrobial support, prevents bacterial adaptation through mechanism diversity, and matches natural antibiotic selection to seasonal infection patterns.
The Minimum Effective Dose Principle
More natural antibiotics don’t equal better results. Minimum effective dose (MED) represents the smallest amount that produces your desired outcome. Operating at MED reduces adverse effect risk, lowers cost, prevents tolerance development, and allows room to increase dosing if needed.
Finding your MED through bracketing:
Start below standard research doses. If studies used 1,200mg aged garlic extract, begin your trial at 600mg. Track outcomes daily. If 600mg achieves your goal (reduced infection frequency, faster wound healing), you’ve found MED without unnecessary excess.
If results fall short, increase by 25-50% increments weekly while maintaining your tracking log. 600mg → 900mg → 1,200mg progression shows you exactly where benefit appears. Many people discover their MED sits below published research doses because individual biology varies tremendously.
Example: Published studies use 2-4 cloves fresh garlic daily for cardiovascular and antimicrobial benefits. You start with 1 clove daily for 4 weeks. If you achieve your infection reduction goal, 1 clove is your MED—why consume more? If not, increase to 2 cloves for 4 weeks and reassess.
Titration for essential oils: Standard dilution is 1-2% for topical antimicrobial use. But sensitive skin might respond to 0.5% dilution, saving expensive oils and reducing irritation risk. Start lower, increase only if results disappoint. For diffusion, start with 3-4 drops in a diffuser rather than 8-10 drops—respiratory benefits often appear at lower concentrations.
MED prevents toxicity accumulation. Herbs contain dozens of compounds beyond the primary active ingredient. At high doses, secondary compounds that cause no issues at normal amounts can accumulate to problematic levels. Garlic’s diallyl disulfide provides antimicrobial benefits but causes digestive upset at excessive doses. Cassia cinnamon’s coumarin offers some benefits but causes liver stress when you consume 6 grams daily trying to maximize effects you’d achieve with 2 grams.
Integration Timing: Syncing With Your Medical Care
Natural antibiotics work best as coordinated additions to medical care, not parallel interventions your doctor doesn’t know about. Integration timing determines whether natural options enhance outcomes or create dangerous interactions.
Before starting prescription antibiotics: If you develop a minor infection and want to try natural antibiotics first, communicate your plan with your clinician. Set strict timelines: “I’ll try garlic for 3 days. If not improving or worsening, I’ll start the prescribed antibiotic immediately.” This keeps your doctor informed and ensures prescription backup when needed.
Some clinicians support this approach for minor infections in otherwise healthy adults. Others prefer immediate antibiotic use. Respect their clinical judgment—they know your full medical history and risk factors you might not consider.
During prescription antibiotic treatment: Some natural antibiotics may enhance antibiotic effectiveness. Fresh garlic extract shows synergistic effects with certain antibiotics in research studies, improving outcomes against resistant bacteria. However, timing matters critically.
Take prescription antibiotics exactly as directed—never skip or delay doses to “make room” for natural supplements. If adding natural antimicrobials during prescription antibiotic treatment, separate dosing by 2-3 hours and inform your prescriber. Some combinations work beautifully; others interfere with absorption or metabolism.
After completing prescription antibiotics: This represents ideal timing for probiotic + gentle antimicrobial support. Prescription antibiotics decimate beneficial gut bacteria along with pathogens. Raw honey, small amounts of garlic in food, and fermented foods help restore microbiome balance while preventing secondary infections during vulnerable recovery periods.
Avoid strong antimicrobials (high-dose oregano oil, berberine, concentrated garlic extract) immediately post-antibiotics—your microbiome needs restoration, not further disruption. Wait 2-4 weeks, then reintroduce stronger natural antimicrobials if needed.
For recurrent infections: Natural antibiotics shine in prevention protocols between acute episodes. If you get 4-5 UTIs yearly despite antibiotic treatment, adding D-mannose and cranberry extract during UTI-free periods may reduce recurrence frequency. If winter brings 6 respiratory infections annually, garlic or echinacea during high-risk months might cut that to 2-3 infections.
Track infection frequency for one year without intervention (your baseline), then track another year with your natural antibiotic prevention protocol. Comparing these periods shows whether your protocol delivers measurable prevention benefits worth continuing.
Cost-Effectiveness Analysis: Maximizing Value
Natural antibiotics range from pennies per serving (garlic, ginger) to several dollars daily (medical-grade Manuka honey, therapeutic essential oils). Cost-effectiveness analysis helps you allocate resources to interventions delivering the best results per dollar spent.
Calculate cost per benefit unit: If you spend $40 monthly on aged garlic extract and reduce sick days from 8 to 3 annually, that’s $96 yearly for 5 fewer sick days—approximately $19 per prevented illness. If those sick days each cost $200 in lost wages, your return on investment is 10x. If you’re salaried without lost wages, calculate the quality-of-life value of not being sick.
Compare this to other interventions. A $25 bottle of medical-grade Manuka honey lasting 3 months treats multiple small wounds effectively. Cost per wound treatment: $2-3. Urgent care visit for infected wound: $150. The honey justifies its premium price through reliable results and avoided medical visits.
Free or low-cost foundations first: Fresh garlic costs $0.50 per bulb (10-12 cloves). At 2 cloves daily, one bulb provides nearly a week of high-quality natural antibiotic for $0.50—about 7 cents per serving. If garlic delivers 70% of the infection reduction you’d get from a $45 aged extract bottle, the fresh garlic offers dramatically better cost-effectiveness.
Raw local honey runs $8-12 per pound and provides both antimicrobial benefits and allergy support. One pound lasts 2-3 months at tablespoon-daily dosing—roughly 10 cents per serving. Compare this to elderberry syrup at $1-2 per serving, and honey wins on cost-effectiveness for year-round use.
Premium products for specific indications: Medical-grade Manuka honey (UMF 15+) costs $40-60 for 8oz but delivers clinically validated wound healing that cheap honey cannot match. For serious wounds or diabetic ulcers, this premium is justified. For daily immune support, standard raw honey works fine.
CO2-extracted oregano oil costs 2-3x more than steam-distilled versions but provides 20-30% higher carvacrol content. If you need maximum antimicrobial effect for acute food poisoning, the premium extraction justifies cost. For prevention during travel, standard oregano oil suffices.
Time value of health: Factor in how quickly natural antibiotics resolve infections versus letting them linger. If garlic resolves your throat infection in 5 days versus 10 days without treatment, those 5 extra days of discomfort, reduced productivity, and potential complication risk have value. Even a $30 monthly supplement cost becomes reasonable if it prevents just one infection requiring time off work or medical intervention.
Building Your Reference Library: Personal Case Studies
Generic natural antibiotic advice fails because individual biology varies enormously. Your personal reference library—documented trials showing what worked, what failed, and what caused problems—becomes more valuable than any published guide.
Case study template for your trials:
Trial #___: [Natural Antibiotic Name] Date: [Start - End] Indication: [Specific infection or prevention goal] Dose: [Exact amount, frequency, timing] Duration: [Days/weeks] Form: [Fresh, extract, oil, etc.] Cost: [Total spent] Outcomes: - Primary goal: [Met/Not met/Partially met] - Time to improvement: [Days] - Side effects: [None/Describe] - Interactions noted: [None/Describe] - Quality of life impact: [Scale 1-10] Objective data: - [Photos, measurements, symptom scores] Decision: - Keep for future use: [Yes/No] - Conditions: [When to use again] - Adjustments: [Dose/timing/form changes] - Cost-effectiveness: [Worth it/Not worth it]
After 10-15 documented trials, patterns emerge with remarkable clarity. You might discover: Garlic prevents your colds reliably but does nothing for skin infections. Raw honey heals minor cuts within 3 days but your throat infections need medical antibiotics. Oregano oil works brilliantly for your food poisoning but triggers migraines. Echinacea reduces your cold duration from 10 to 6 days consistently.
These personal insights beat generic recommendations because they’re based on your biology, your infection patterns, and your response history. Share this reference library with your clinician—documented trials demonstrate thoughtful self-care and help them make better recommendations tailored to your proven responses.
Cross-reference with medication changes: If you start blood pressure medication or diabetes treatment, flag this in your library. Natural antibiotics you previously tolerated well might now cause interactions. Your reference library prevents you from blaming garlic for hypoglycemia when the real culprit is the new interaction between garlic and metformin you just started.
Update for aging and life changes: Natural antibiotic responses change as you age, during pregnancy, with menopause, or after major health events. A 30-year-old might tolerate high-dose garlic extract beautifully; the same person at 65 with reduced kidney function might need half that dose. Review and update your library during major life transitions.
The Counterintuitive Truth: When NOT to Use Natural Antibiotics
Knowing when natural antibiotics offer little benefit—or actively interfere with better options—demonstrates more sophisticated understanding than knowing when to use them.
Viral infections dominate: Most respiratory infections, sore throats, and “stomach flu” episodes stem from viruses, not bacteria. Natural antibiotics don’t kill viruses effectively. Taking garlic for influenza might offer minor anti-inflammatory benefits, but it won’t shorten duration meaningfully. Elderberry and echinacea show some antiviral activity, but these aren’t classified as “antibiotics.”
If you’re paying $40 monthly for natural antibiotics to prevent colds, you’re targeting the wrong mechanism. Sleep quality, stress management, hand hygiene, and avoiding crowded spaces during peak season prevent more infections than any antimicrobial. Reallocating that $40 to a gym membership or meditation app delivers better infection reduction through immune system optimization.
Serious infections need serious medicine: Pneumonia, kidney infections, severe cellulitis, sepsis, meningitis, and bone infections require prescription antibiotics immediately—often intravenously. Natural antibiotics cannot deliver the tissue concentrations and pharmacokinetic profiles needed to treat these life-threatening conditions.
Delaying appropriate treatment for dangerous infections to “try natural options first” can result in permanent organ damage or death. No amount of garlic or oregano oil will save you from sepsis. Recognize this boundary clearly.
Prevention paradox: You can’t prevent infections you’re not at risk for. If you get one minor infection every 2-3 years, daily natural antibiotic supplementation costs hundreds of dollars annually to prevent maybe one illness. That’s poor cost-effectiveness. Save natural antibiotics for actual infections or high-risk periods (air travel, winter, after stress events).
Chronic conditions need different approaches: If you have chronic sinusitis, recurrent UTIs, or persistent skin infections, underlying causes need addressing—not just antimicrobial Band-Aids. Chronic infections often stem from structural issues (deviated septum), immune dysfunction, biofilm formation, or undiagnosed conditions like diabetes. Natural antibiotics might provide temporary symptom relief while missing the root problem entirely.
Work with your clinician to identify WHY infections keep recurring. Treat that cause (surgery for structural issues, immunoglobulin replacement for immune deficiency, better diabetes control) rather than perpetually fighting infections with natural or prescription antimicrobials.
Your Action Checklist: Getting Started Today
Use this checklist to start using natural antibiotics safely and effectively:
Before your first trial:
☐ Review your current medications with your doctor or pharmacist for potential interactions
☐ Identify your specific goal (treat current infection, prevent future infections, support wound healing)
☐ Choose ONE natural antibiotic based on your infection type (see comparison table above)
☐ Set a trial end date (5 days for acute infection, 8-12 weeks for prevention)
☐ Write down your stop criteria (no improvement by day X, specific side effects, fever above Y)
During your trial:
☐ Track symptoms daily (pain level 0-10, redness diameter, functional impact)
☐ Take photos of wounds or visible infections for objective comparison
☐ Monitor for side effects (digestive upset, rash, headache, unusual symptoms)
☐ Check blood sugar more frequently if using garlic, berberine, or cinnamon
☐ Keep fast-acting carbs available if you take diabetes medications
After 5-7 days (acute infection) or 8-12 weeks (prevention):
☐ Review your documented results objectively
☐ Decide: Keep (it worked), Drop (no benefit), or Adjust (modify dose/form)
☐ Add successful options to your personal reference library
☐ Share results with your healthcare provider at next visit
☐ Plan next trial if needed (introduce one new option at a time)
⚠️ Get medical help immediately if:
☐ Fever exceeds 101°F for more than 48 hours or reaches 103°F at any point
☐ Redness spreads beyond the initial infection site or red streaks appear
☐ Pain worsens despite 3 days of treatment
☐ You develop difficulty breathing, chest pain, confusion, or severe weakness
☐ Facial swelling occurs with dental infections
— Clinical Antimicrobial Research
Natural Antibiotics Myths Debunked by Research

Let’s clear up some persistent misconceptions. Separating evidence from marketing claims helps you make informed decisions and avoid throwing money at ineffective approaches.
| Myth | Fact |
|---|---|
| “Natural antibiotics can replace prescriptions for serious infections” | Natural options complement care but cannot treat severe bacterial infections like pneumonia, sepsis, kidney infections, or meningitis. Research shows modest effects at best for minor infections. Serious bacterial infections require prescription antibiotics’ tissue penetration, dosing precision, and pharmacokinetics that natural compounds cannot achieve. |
| “All honey works the same as an antibiotic” | Medical-grade Manuka honey has significantly higher antimicrobial activity due to methylglyoxal (MGO) content. Regular processed honey loses enzymes and compounds during pasteurization and filtration. UMF ratings (10+, 15+, 20+) indicate methylglyoxal levels—higher ratings deliver stronger antibacterial effects. Not all honey provides therapeutic antimicrobial benefits. |
| “Essential oils are safe because they’re natural” | Undiluted essential oils cause chemical burns, allergic reactions, and organ toxicity. Oregano and thyme oils should never be ingested—even small amounts cause severe mucous membrane irritation and liver toxicity. Always dilute to 1-2% for topical use. “Natural” doesn’t mean safe; essential oils are 50-100x more concentrated than dried herbs. |
| “You can’t develop resistance to natural antibiotics” | While slower than antibiotic resistance, bacteria can adapt to natural compounds with continuous exposure. Biofilm-forming bacteria show particular adaptability. Rotation strategies (changing compounds every 8-12 weeks) and time-limited trials prevent adaptation. Natural antibiotics should not be used indefinitely without breaks. |
| “More is better for natural remedies” | High doses increase toxicity risk without proportional benefits. Cassia cinnamon contains coumarin—safe at culinary amounts but hepatotoxic at supplement doses. Garlic causes bleeding issues at excessive doses. Finding your minimum effective dose reduces adverse effects while maintaining benefits. More often means more side effects, not better results. |
| “If a little helps, a lot will help more” | Dose-response curves for natural antibiotics often plateau or reverse at high doses. Beyond minimum effective dose, additional amounts provide no extra benefit and increase toxicity risk. Turmeric absorption doesn’t improve past optimal fat and black pepper combinations. Excessive honey intake raises blood sugar without enhancing antimicrobial activity. |
| “Natural antibiotics work immediately like prescription antibiotics” | Natural antimicrobials work more slowly—typically 3-5 days before noticeable improvement. Prescription antibiotics achieve higher tissue concentrations faster. If you need rapid infection control (spreading cellulitis, high fever), natural options won’t deliver fast enough. Save them for minor infections and prevention, not medical emergencies. |
| “Natural antibiotics boost your immune system” | Some compounds (echinacea, elderberry) stimulate immune response. Others (garlic, honey, oregano oil) kill bacteria directly without immune system involvement. “Immune boosting” isn’t universally positive—people with autoimmune conditions should avoid immune stimulation. Most natural antibiotics work through direct antimicrobial mechanisms, not immune enhancement. |
Frequently Asked Questions
Let’s address the most common questions we hear about natural antibiotics—with straight answers based on research, not marketing hype.
What is the strongest natural antibiotic?
Garlic (allicin) and oregano oil (carvacrol) show the broadest antibacterial properties in research. Garlic effectively fights gram-positive and gram-negative bacteria, including antibiotic-resistant strains like MRSA. Oregano oil exhibits powerful antimicrobial activity against food-borne pathogens and respiratory bacteria. However, effectiveness depends on infection type—raw honey excels for wound infections while garlic works better for respiratory issues.
Can natural antibiotics cure a bacterial infection?
Natural antibiotics can help resolve minor bacterial infections like small skin wounds, mild throat infections, or early-stage UTIs when used properly. However, they cannot cure serious bacterial infections requiring prescription antibiotics—pneumonia, severe cellulitis, kidney infections, or sepsis need immediate medical treatment. Use natural options for prevention and minor infections only, coordinating with your doctor for anything beyond mild symptoms.
How long do natural antibiotics take to work?
Topical applications (honey on wounds, diluted essential oils) show effects within 24-48 hours—reduced pain, less redness, decreased drainage. Internal use (garlic, echinacea, ginger) requires 3-5 days for noticeable improvement in mild infections. No improvement by day 5 requires medical evaluation. Natural antibiotics work slower than prescription antibiotics due to lower tissue concentrations and different mechanisms.
Are natural antibiotics safe for children?
Food amounts are safe for children—garlic in meals, ginger tea, honey for children over 1 year. Never give honey to infants under 12 months (botulism risk). Supplements and essential oils require pediatric guidance due to higher toxicity risks in smaller bodies. Essential oils should never be used on infants under 2 years. Always coordinate natural antibiotic use with your child’s pediatrician and start with the lowest effective dose.
Do natural antibiotics kill viruses?
Natural antibiotics primarily target bacteria, not viruses. Most respiratory infections, sore throats, and stomach bugs are viral—natural antibacterial agents won’t shorten duration significantly. Some compounds like elderberry and echinacea show antiviral properties in studies, but these work through different mechanisms than antibacterial activity. For viral infections, focus on rest, hydration, and symptom management rather than antibacterial treatments.
Can I take natural antibiotics with prescription medications?
Some combinations are safe, others create risks. Garlic amplifies blood thinners (warfarin, aspirin) increasing bleeding. Berberine inhibits drug-metabolizing enzymes, raising blood levels of statins and antidepressants. Natural antibiotics that lower blood sugar combined with diabetes medications increase hypoglycemia risk. Always review your complete medication list with your doctor before starting any natural antibiotic. Never stop prescribed medications without medical supervision.
Which natural antibiotic is best for a tooth infection?
Clove oil (eugenol) provides both antibacterial effects and pain relief for dental infections. Apply diluted clove oil topically or place a whole clove near the affected tooth for temporary relief. However, dental infections typically require professional drainage and prescription antibiotics—natural options only provide temporary symptom relief. Facial swelling, fever, difficulty swallowing, or swelling near your eye requires emergency dental care immediately.
How much do natural antibiotics cost?
Fresh garlic costs approximately $0.07 per serving (2 cloves from a $0.50 bulb). Raw honey ranges from $0.10-0.30 per tablespoon for local varieties. Medical-grade Manuka honey costs $40-60 per 8oz jar. Oregano oil capsules run $15-30 for a month’s supply. Essential oils range $10-40 per bottle lasting 3-6 months. Generic prescription antibiotics often cost $4-20 per course. Cost-effectiveness depends on prevention success and your specific infection patterns.
Can natural antibiotics prevent antibiotic resistance?
Using natural antibiotics for minor infections may reduce unnecessary prescription antibiotic use, potentially slowing resistance development at a population level. However, bacteria can develop tolerance to natural compounds with continuous exposure—though slower than prescription antibiotic resistance. Rotation strategies (changing compounds every 8-12 weeks) and time-limited use help prevent adaptation. Natural antibiotics should complement, not replace, appropriate antibiotic stewardship.
What’s the difference between antibacterial and antimicrobial?
Antibacterial specifically means “kills or inhibits bacteria.” Antimicrobial is broader—it means “kills or inhibits microorganisms” including bacteria, fungi, viruses, and parasites. Natural antibiotics typically have antibacterial properties (work against bacteria) and may also have antifungal or antiviral effects. For example, oregano oil has antibacterial properties against E. coli and antimicrobial activity against Candida fungus. The terms are often used interchangeably when discussing bacterial infections.
References
- Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008;57(5):712-717. PubMed
- Ankri S, Mirelman D. Antimicrobial properties of allicin from garlic. Microbes Infect. 1999;1(2):125-129. PubMed
- Brudzynski K. A current perspective on hydrogen peroxide production in honey. Food Chem. 2020;332:127229. PubMed
- Sakkas H, Papadopoulou C. Antimicrobial activity of basil, oregano, and thyme essential oils. J Microbiol Biotechnol. 2017;27(3):429-438. PubMed
- Manayi A, Vazirian M, Saeidnia S. Echinacea purpurea: Pharmacology, phytochemistry and analysis methods. Pharmacogn Rev. 2015;9(17):63-72. PMC Article
- Pasupuleti VR, Sammugam L, Ramesh N, Gan SH. Honey, propolis, and royal jelly: A comprehensive review of their biological actions and health benefits. Oxid Med Cell Longev. 2017;2017:1259510. PMC Article
- Borlinghaus J, Albrecht F, Gruhlke MC, Nwachukwu ID, Slusarenko AJ. Allicin: Chemistry and biological properties. Molecules. 2014;19(8):12591-12618. PMC Article
- Sharifi-Rad M, Varoni EM, Iriti M, et al. Carvacrol and human health: A comprehensive review. Phytother Res. 2018;32(9):1675-1687. PubMed
- Hewlings SJ, Kalman DS. Curcumin: A review of its effects on human health. Foods. 2017;6(10):92. PMC Article
- Hudson EA, Dinh PA, Kokubun T, Simmonds MS, Gescher A. Characterization of potentially chemopreventive phenols in extracts of brown rice that inhibit the growth of human breast and colon cancer cells. Cancer Epidemiol Biomarkers Prev. 2000;9(11):1163-1170. PubMed
- Josling P. Preventing the common cold with a garlic supplement: A double-blind, placebo-controlled survey. Adv Ther. 2001;18(4):189-193. PubMed
- White B, Judkins DZ. Clinical inquiry: Does turmeric relieve inflammatory conditions? J Fam Pract. 2011;60(3):155-156. PubMed
- National Institutes of Health Office of Dietary Supplements. Garlic Fact Sheet. Updated 2020.
- Centers for Disease Control and Prevention. Antibiotic Resistance & Patient Safety Portal. Updated 2024.
- World Health Organization. Antimicrobial Resistance Fact Sheet. Updated 2023.
Conclusion: Natural Antibiotics as Part of a Comprehensive Strategy
Natural antibiotics work—but not as miracle cures or prescription replacements. They shine in a specific role: preventing infections during high-risk periods, supporting recovery from minor bacterial infections, and complementing medical care when you use them systematically. Here’s the truth: the difference between people who get real benefits and those who waste money on supplements that do nothing comes down to one thing—methodology over hope.
The time-boxed trial approach, minimum effective dosing, seasonal rotation strategy, and personal reference library transform natural antibiotics from random experiments into evidence-based protocols tailored to your biology. This systematic framework (test one compound at a time, set clear stop criteria, track outcomes objectively, keep what works) creates personalized data worth more than any generic recommendation. You’ll learn exactly which natural antibiotics work for your infection patterns and which ones waste your money.
Start with one: garlic for respiratory infections, raw honey for minor wounds, or oregano oil for suspected food poisoning. Set a 5-day trial. Track daily. Coordinate with your clinician. The documented result—improvement or lack thereof—tells you whether to keep that option in your toolkit. After 5-10 trials, you’ll have built a personalized reference library showing what actually works for your body. That knowledge compounds over years, making you progressively better at preventing and managing minor infections naturally while recognizing when prescription antibiotics remain absolutely essential.
Related Articles
- 7 Natural Supplements to an Appropriate Blood Sugar Levels
- Omega-3 vs Omega-6: Finding the Right Balance to Reduce Inflammation
- Can Garlic Lower Blood Pressure? Science-Backed Facts
- The Ultimate Guide to Natural Diabetes Support
- Natural Remedies vs Prescription Drugs: What’s the Difference?
Author Bio
The Remedy Verified Team is dedicated to exploring natural, research-backed approaches to chronic health conditions. Our writers translate complex scientific studies into clear, practical insights to help readers make informed decisions about their health. also check out About the Author
Disclaimer
⚠️ Disclaimer: The information provided in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. Natural remedies, supplements, and lifestyle changes may affect individuals differently. Always consult a qualified healthcare professional before making any changes to your diet, medications, or health routine—especially if you have an existing medical condition, are pregnant, or are taking prescription drugs. Remedy Verified does not provide medical services, and the content shared here should not be considered a substitute for professional medical guidance. Use of this website and its information is at your own risk.