Magnesium for Diabetes: The Mineral That Improves Insulin Sensitivity
Exploring the benefits of magnesium for diabetes can provide new insights into managing the condition effectively.
For the complete strategy that ties diet, lifestyle, and supplements together, read our hub: The Ultimate Guide to Natural Diabetes Support.
Introduction
Magnesium is one of the most widely used minerals in human metabolism, yet it’s also one of the most commonly under-consumed nutrients. For people living with type 2 diabetes or prediabetes, that gap matters. Magnesium participates in hundreds of enzymatic reactions—including those involved in glucose transport and insulin signaling—so falling short can nudge blood sugar in the wrong direction. Encouragingly, both large cohort studies and clinical trials suggest that improving magnesium status can support healthier glycemic control and reduce the risk of progression to type 2 diabetes.
This guide explains what magnesium does, why deficiency is common in diabetes, what the research shows, which foods and supplements actually work, and how to build a practical plan you can sustain. Throughout, we’ll link to trusted sources such as the NIH Office of Dietary Supplements, the Harvard T.H. Chan School of Public Health, and peer-reviewed studies on PubMed.
What Is Magnesium and Why It Matters for Glucose Control
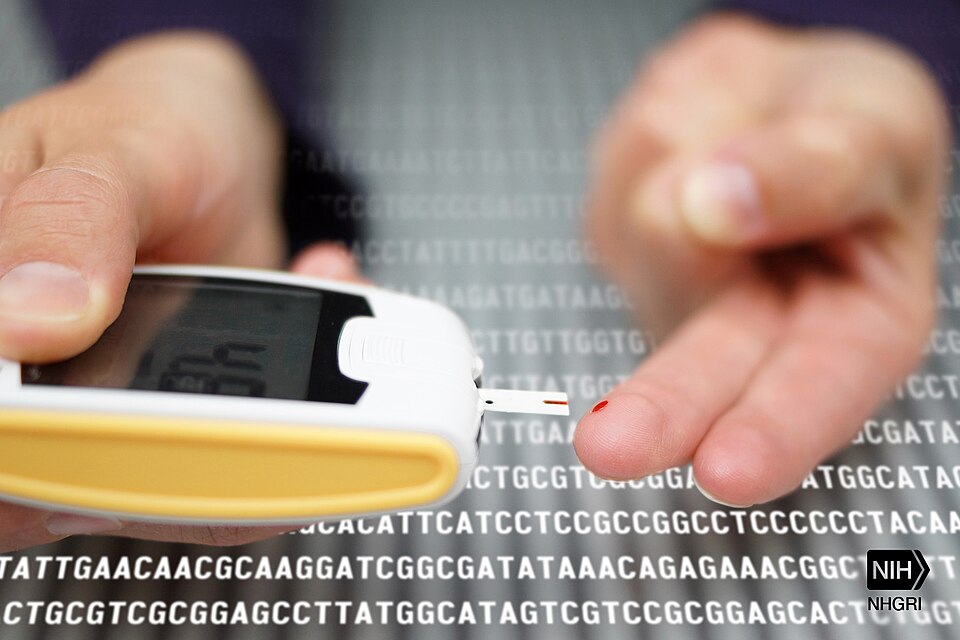
Magnesium is an essential mineral and electrolyte that helps convert food to energy, stabilize cell membranes, and regulate ion channels. In glucose metabolism specifically, magnesium is a cofactor for kinases in the insulin signaling cascade and influences GLUT4 translocation—the step that helps shuttle glucose into muscle and fat cells. Low magnesium can therefore impair insulin action and contribute to insulin resistance.
- Insulin signaling cofactor: Magnesium enables key enzymes in the insulin pathway to function properly, so a shortfall can blunt the body’s response to insulin and make post-meal spikes harder to control.
- Glucose transport and muscle uptake: By supporting GLUT4 activity and mitochondrial energy production in skeletal muscle, adequate magnesium helps tissues use glucose more efficiently during and after meals.
- Inflammation and oxidative stress: Suboptimal magnesium status is associated with higher inflammatory markers; restoring levels may help lower chronic inflammation that worsens insulin resistance.
Magnesium and Blood Sugar Regulation: What the Research Shows

- Prospective cohorts: Large populations followed for years show a dose–response relationship: each incremental increase in daily magnesium intake is associated with lower diabetes risk (Harvard summary).
- Clinical trials in insulin resistance: Supplementation (often 250–400 mg elemental magnesium/day) has improved HOMA-IR and fasting glucose in people with prediabetes or metabolic syndrome (e.g., trials indexed on PubMed).
- Trials in type 2 diabetes: Studies report modest but meaningful improvements in fasting glucose and sometimes HbA1c when magnesium is added to standard care—particularly in participants starting with low serum magnesium.
Takeaway: Magnesium is not a replacement for medication, but it’s a credible, low-risk lever that can complement diet, movement, and prescribed therapy.
Why Magnesium Deficiency Is Common in Diabetes
People with type 2 diabetes have an elevated likelihood of suboptimal magnesium status due to urinary losses driven by hyperglycemia, lower dietary intake, and certain medications. Because serum magnesium is tightly regulated, a normal lab value doesn’t always reflect tissue levels; symptoms and dietary patterns still matter.
- Glycosuria and urinary losses: Elevated blood glucose can increase urine output and magnesium excretion, slowly eroding the body’s reserves even when intake looks adequate on paper.
- Lower intake from modern diets: Highly processed foods and refined grains contain less magnesium than whole grains, legumes, nuts, and leafy greens; shifting toward minimally processed staples often corrects a significant portion of the gap.
- Medication and health factors: Certain diuretics, proton pump inhibitors, and long-term GI conditions can reduce absorption or increase losses, creating a need for more attentive intake.
Clinical Evidence: Prevention and Management
Two lines of evidence matter most: long-term prevention data and short-term intervention trials.
- Prevention: Multiple pooled analyses of prospective cohorts report a statistically significant reduction in new-onset type 2 diabetes among participants with higher magnesium intake, even after adjusting for BMI and other lifestyle factors (Harvard overview).
- Management: Randomized trials in people with type 2 diabetes and low magnesium status have shown improvements in fasting glucose, insulin sensitivity indices, and sometimes HbA1c after 8–24 weeks of supplementation (common doses: ~300–400 mg elemental magnesium per day; see PubMed).
- Cardiometabolic context: Magnesium status also correlates with blood pressure, arrhythmia risk, and muscle function, making it a broadly relevant nutrient in cardiometabolic health (NIH ODS professional fact sheet).
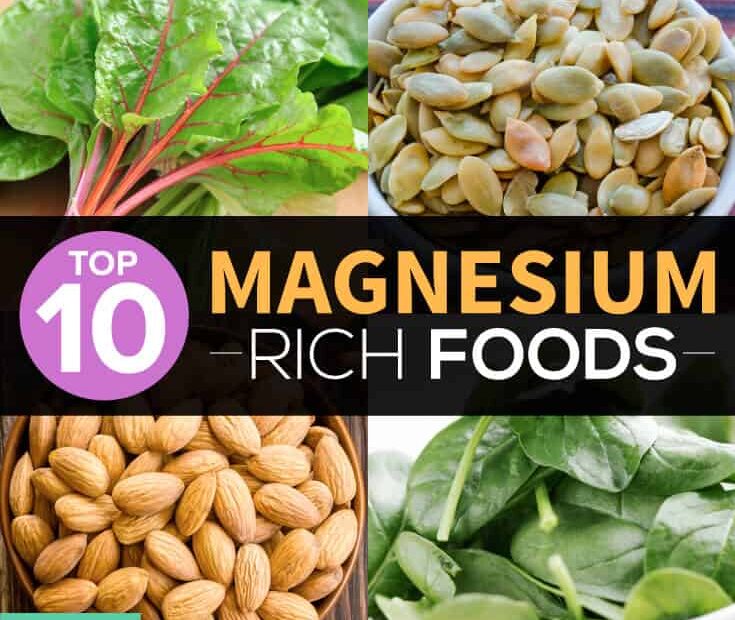
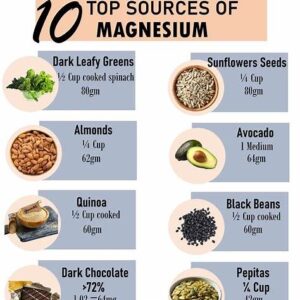
Best Food Sources of Magnesium (and How to Use Them)
Food-first works, especially when you build meals around legumes, nuts, seeds, whole grains, and leafy greens. Here’s how to turn those staples into everyday habit—without relying on sugar-heavy sauces or refined starches.

| Food | Approx. Mg (per serving) | How to Use It (Practical Ideas) |
|---|---|---|
| Pumpkin seeds (1 oz) | ~150 mg | Sprinkle on Greek yogurt with cinnamon; fold into salads; blend into pesto. |
| Almonds (1 oz) | ~80 mg | Pair with fruit for a balanced snack; grind into almond meal for crusts. |
| Spinach, cooked (1 cup) | ~150 mg | Stir into omelets or soups; sauté with olive oil and garlic. |
| Black beans (1 cup) | ~120 mg | Burrito bowls; puree for a protein-rich soup base. |
| Quinoa, cooked (1 cup) | ~115 mg | Base for grain bowls; chill for next-day salads. |
| Dark chocolate (70–85%, 1 oz) | ~65 mg | Enjoy a square after dinner; melt a small amount over berries. |
| Avocado (1 medium) | ~60 mg | Mash with lime and herbs; whole-grain toast with eggs. |
- Balance matters at meals: Pair magnesium-rich foods with protein and fiber to slow digestion and reduce post-meal glucose spikes.
- Swap refined for whole: Replace white rice with quinoa or farro; trade croutons for pumpkin seeds; use unsweetened oats with nuts.
- Plan for consistency: Include at least one high-magnesium food at every meal so intake stays steady without tracking obsessively.
For detailed nutrient data, see the USDA FoodData Central database.
Magnesium Supplements for Diabetes: Forms, Absorption, and Doses
When diet alone isn’t enough—or when lab work and symptoms suggest a deficit—supplementation can help. Not all forms are absorbed the same way, and tolerability varies. Choose a form you’ll actually take consistently.
| Form | Best For | Absorption & Tolerability | Notes |
|---|---|---|---|
| Magnesium glycinate | Daily use; sensitive GI tracts | High bioavailability; gentle on stomach | Good first choice for long-term use; often taken in the evening for calm. |
| Magnesium citrate | General supplementation | Well absorbed; mild laxative effect in some | Split doses with meals if GI sensitivity occurs. |
| Magnesium oxide | Constipation + budget | Lower absorption; stronger laxative effect | Less ideal for repleting levels; consider other forms if possible. |
| Magnesium malate | Muscle energy and soreness | Good tolerability for many | Pairs well with morning doses; some find it “energizing.” |
| Magnesium threonate | CNS support, cognition | Designed for brain penetration | Often pricier; use when cognitive support is prioritized. |
- Typical doses: Many trials in insulin resistance or type 2 diabetes use ~250–400 mg elemental magnesium daily; check the label for elemental content rather than total compound weight.
- Timing and splitting: If you experience GI upset, split the daily amount into two or three doses with meals; consistent smaller doses often absorb better than large single boluses.
- Quality and labeling: Choose brands that disclose form, elemental amount, and independent testing; avoid proprietary blends that hide the actual magnesium content.
Safety, Interactions, and Who Should Be Cautious
Magnesium from food is safe for most people. Supplements are also generally safe when used as directed, but a few cautions apply—especially if you have medical conditions or take certain medications.
- Kidney disease: Reduced renal function can impair magnesium excretion, increasing risk of elevated levels; always consult your clinician before supplementing if you have CKD.
- Medication interactions: Magnesium can interfere with absorption of tetracycline and fluoroquinolone antibiotics and certain thyroid medications; take these drugs several hours apart from magnesium (see NIH ODS professional fact sheet).
- GI symptoms: Loose stools are more common with citrate and oxide; switching to glycinate or lowering the dose usually resolves the issue.
- Hypoglycemia awareness: As overall insulin sensitivity improves with diet, movement, and supplements, monitor glucose closely to avoid lows—especially if you use insulin or sulfonylureas; follow the latest ADA Standards of Care.
Magnesium vs. Other Minerals in Diabetes (Quick Comparison)
| Nutrient | Primary Role | Evidence for Glycemic Impact | Notes |
|---|---|---|---|
| Magnesium | Insulin signaling, glucose transport | Moderate evidence for fasting glucose and insulin sensitivity; prevention support in cohorts | Food-first plus 250–400 mg/day supplements if needed. |
| Chromium | Insulin cofactor | Mixed; benefits may depend on deficiency status | Consider only with clinician guidance due to variability. |
| Zinc | Insulin storage and secretion | Some evidence for glycemic markers; more robust for immune/skin | Avoid excess; balance with copper if supplementing long-term. |
| Potassium | Electrolyte balance, blood pressure | Indirect glycemic effects via cardiometabolic health | Manage with clinician if on ACE inhibitors or ARBs. |
Building a Practical Magnesium Plan (Step-by-Step)
- Audit your baseline: Review your usual meals and identify low-magnesium spots (e.g., refined grains, limited legumes/nuts). Add one high-magnesium food to each meal and repeat that pattern daily for two weeks.
- Layer in movement: Pair meals with a 10–15-minute walk to improve post-meal glucose uptake. Magnesium plus light activity is a simple, sustainable combo for insulin sensitivity.
- Consider supplements if needed: If intake remains low or symptoms persist (cramps, low energy, insulin resistance), start with 200 mg elemental magnesium at night (glycinate or citrate), then titrate to ~300–400 mg/day as tolerated.
- Track and adjust: Log fasting and post-meal glucose a few days per week. If values improve and GI tolerance is good, continue; if not, adjust form/dose with your clinician’s input.
- Integrate with your broader plan: Combine magnesium with proven levers—adequate protein, viscous fiber (beans, oats), sleep hygiene, stress management—outlined in our main guide.
FAQs
Can magnesium lower blood sugar?
It can help. Trials show improvements in fasting glucose and insulin sensitivity, especially in people who start out deficient. It’s an adjunct to—not a replacement for—medical therapy and lifestyle.
What type of magnesium is best for diabetes?
Glycinate and citrate are well-absorbed and generally gentle on the stomach. Oxide is cheaper but less bioavailable and more likely to loosen stools.
How much magnesium should I take?
Common supplemental targets are ~250–400 mg elemental magnesium per day. Start lower if you’re sensitive, and split doses with meals if needed.
How long until I notice benefits?
Dietary changes can help within weeks; supplement trials often run 8–12 weeks. Track fasting and post-meal numbers to see your personal response.
Can I get enough from food alone?
Yes—if your diet is rich in legumes, nuts, seeds, whole grains, and leafy greens. Many people still benefit from a supplement to reliably reach targets.
Key Takeaways
- Magnesium for diabetes is evidence-supported: Higher intake is linked with lower risk of type 2 diabetes, and supplementation improves insulin sensitivity in many trials.
- Food first, supplements as needed: Build meals around legumes, nuts, seeds, greens, and whole grains; use 250–400 mg/day supplements if diet alone falls short.
- Integrate with your routine: Pair magnesium with fiber-rich meals, post-meal walks, consistent sleep, and prescribed therapy; see our Ultimate Guide for the full playbook.
References
- NIH Office of Dietary Supplements. Magnesium — Health Professional Fact Sheet.
- Harvard T.H. Chan School of Public Health. The Nutrition Source: Magnesium.
- USDA FoodData Central. Nutrient profiles for foods rich in magnesium.
- PubMed search: randomized controlled trials of magnesium in type 2 diabetes.
- American Diabetes Association. Standards of Care in Diabetes—2025.
Author Bio
Omar Aljaff is the founder of Remedy Verified, where he translates complex research on natural remedies into practical, safe strategies for people managing chronic conditions.
Disclaimer
The information in this article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional before changing your diet, supplements, or medications—especially if you use insulin, sulfonylureas, or have kidney disease.