Lower Cholesterol Supplements: Evidence-Based Guide to Natural Options
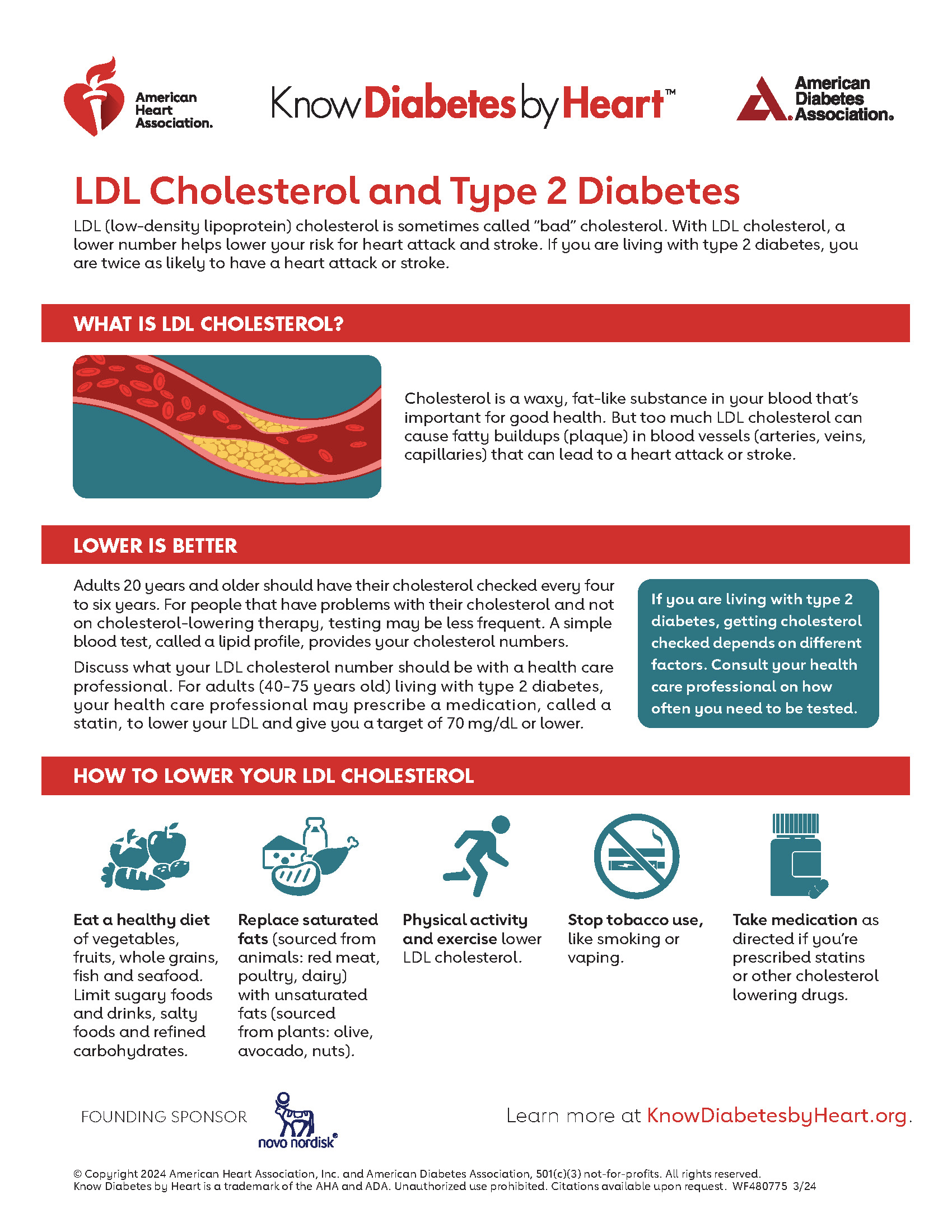
Elevated cholesterol levels affect nearly 94 million Americans, consequently driving a substantial market for supplements promising cholesterol reduction. However, navigating the complex landscape of lower cholesterol supplements requires understanding which options demonstrate scientific validity versus marketing claims. Furthermore, recent research has fundamentally challenged long-held assumptions about supplement effectiveness, particularly when compared to established medical interventions.
The quest for best supplements to lower cholesterol has intensified as consumers increasingly seek natural alternatives to pharmaceutical options. Moreover, the dietary supplement industry, valued at approximately $50 billion annually, aggressively markets numerous products specifically targeting cardiovascular health. Nevertheless, rigorous clinical trials reveal significant gaps between marketing promises and actual efficacy for most popular supplements.
Understanding Cholesterol and Supplement Mechanisms
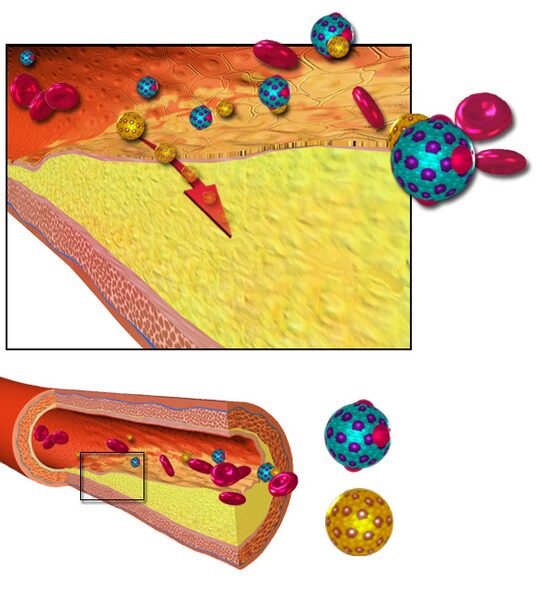
Cholesterol metabolism involves intricate biochemical pathways that supplements can theoretically influence through multiple mechanisms. Specifically, dietary supplements may target cholesterol absorption in the intestines, hepatic cholesterol synthesis, or bile acid metabolism. Additionally, some compounds work by enhancing cholesterol elimination or modifying lipoprotein particle composition and size.
Understanding these mechanisms becomes crucial when evaluating supplement claims and setting realistic expectations. Furthermore, the complexity of cholesterol regulation explains why single-ingredient supplements often produce disappointing results. Consequently, the most promising approaches typically involve multi-component formulations targeting different pathways simultaneously.
Plant Sterols and Stanols: The Most Established Option
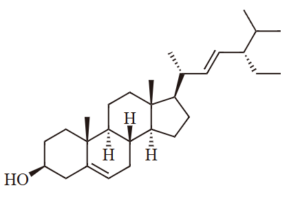
Plant sterols and stanols represent the most scientifically validated category of cholesterol-lowering supplements, with extensive research demonstrating consistent benefits. Mechanistically, these compounds compete with dietary cholesterol for absorption in the small intestine, thereby reducing cholesterol bioavailability. Moreover, studies show that dietary supplements containing plant stanols or sterols, taken with meals, can reduce cholesterol levels.
⏳ Plant Sterol Action Timeline:
Research consistently demonstrates that plant sterols require specific dosing protocols for optimal effectiveness. Importantly, Cleveland Clinic recommends consuming 2-3 grams daily of plant sterols with meals for maximum cholesterol-lowering benefits. Additionally, these compounds work best when incorporated into fortified foods rather than taken as isolated supplements.
However, plant sterols are not appropriate for everyone. Specifically, individuals with sitosterolemia, a rare genetic condition affecting sterol metabolism, should avoid these supplements entirely. Furthermore, some research suggests potential concerns about elevated plant sterol levels and cardiovascular risk, though this remains controversial among experts.
Red Yeast Rice: Potent but Problematic
Red yeast rice contains monacolin K, a compound chemically identical to the prescription medication lovastatin. Consequently, red yeast rice products with substantial monacolin K content can produce significant cholesterol reductions. However, the FDA has determined that red yeast rice containing more than trace amounts of monacolin K is an unapproved new drug and cannot be legally sold as a dietary supplement.
Clinical trials examining red yeast rice effectiveness reveal impressive results, but with significant caveats. For instance, a randomized controlled trial found that red yeast rice reduced LDL cholesterol by 23.3% to 25.6% in participants with hypercholesterolemia. Nevertheless, the unpredictable nature of monacolin K content across products makes consistent dosing nearly impossible.
Moreover, the regulatory gray area surrounding red yeast rice creates substantial quality control challenges. Furthermore, consumers cannot reliably determine whether products contain therapeutic amounts of active compounds or potentially harmful contaminants. Consequently, most healthcare providers recommend avoiding red yeast rice supplements in favor of regulated pharmaceutical alternatives.
Fiber Supplements and Soluble Fiber

Soluble fiber represents one of the most mechanistically sound approaches to cholesterol reduction through supplementation. Specifically, soluble fiber binds bile acids in the digestive tract, forcing the liver to convert cholesterol into replacement bile acids. Additionally, certain types of soluble fiber can influence gut microbiota composition, potentially affecting cholesterol metabolism through secondary mechanisms.
“Fiber binds to cholesterol and eliminates it from your body. Getting enough fiber also reduces your risk of diseases, prevents constipation and keeps you feeling full for longer.”
Psyllium husk stands out among fiber supplements for its robust clinical evidence supporting cholesterol reduction. Specifically, studies demonstrate that psyllium can reduce LDL cholesterol by 5-10% when consumed consistently. Moreover, studies suggest that whole flaxseed and flaxseed lignans may help to lower cholesterol levels, though flaxseed oil does not provide the same benefits.

Beta-glucan, found in oats and barley, represents another well-studied soluble fiber with cholesterol-lowering properties. Furthermore, the FDA has approved health claims specifically for beta-glucan’s cardiovascular benefits. Nevertheless, achieving therapeutic doses through supplements rather than whole foods can be challenging and potentially less effective.
Omega-3 Fatty Acids: Mixed Evidence for Cholesterol
Omega-3 fatty acid supplements, particularly EPA and DHA from fish oil, have generated enormous consumer interest for cardiovascular health. However, their direct effects on LDL cholesterol remain modest and inconsistent across studies. Conversely, omega-3 supplements demonstrate more reliable effects on triglyceride reduction, particularly in individuals with elevated levels.

Recent large-scale trials have challenged previous assumptions about omega-3 supplements and cardiovascular outcomes. Importantly, the American Heart Association’s 2022 study found that fish oil showed no significant cholesterol-lowering effects compared to placebo. Nevertheless, omega-3 supplements may benefit specific populations, particularly those with very high triglyceride levels exceeding 500 mg/dL.
The discrepancy between supplement studies and whole food research suggests that omega-3 benefits may depend on the complete nutrient matrix found in fish. Additionally, the quality and purity of omega-3 supplements vary dramatically across manufacturers. Consequently, individuals seeking omega-3 benefits should prioritize dietary sources over supplemental forms when possible.
Niacin: Once Promising, Now Discouraged
Niacin, also known as vitamin B3, was historically considered a promising option for cholesterol management due to its ability to raise HDL cholesterol and lower triglycerides. However, recent evidence has fundamentally changed recommendations regarding niacin supplementation for cardiovascular health. Specifically, Cleveland Clinic experts state that “niacin is no longer recommended as a treatment for lowering cholesterol” due to safety concerns and limited effectiveness.
Large-scale clinical trials revealed that niacin’s apparent benefits on cholesterol numbers did not translate into reduced cardiovascular events. Moreover, niacin supplementation carries significant side effect risks, including flushing, liver toxicity, and potential interference with diabetes management. Furthermore, most Americans already consume adequate niacin through fortified foods, making additional supplementation unnecessary and potentially harmful.
Emerging and Alternative Supplements
Several other compounds have attracted attention for potential cholesterol-lowering effects, though evidence remains limited or mixed. For instance, berberine shows promise in some studies for lipid management, but requires careful monitoring due to potential drug interactions. Similarly, artichoke leaf extract demonstrates modest cholesterol-lowering effects in certain populations.
| Supplement | Typical Dose | Evidence Quality | LDL Reduction |
|---|---|---|---|
| Plant Sterols/Stanols | 2-3g daily | Strong | 6-15% |
| Psyllium Husk | 5-10g daily | Moderate | 5-10% |
| Red Yeast Rice | Variable | Moderate* | 15-25% |
| Berberine | 500mg 2-3x daily | Limited | 10-15% |
| Garlic Extract | 600-900mg daily | Weak | 5-8% |
Green tea extracts have shown modest cholesterol-lowering effects in some studies, though results remain inconsistent. Additionally, limited evidence suggests that green tea may have cholesterol-lowering effects, but more research is needed to establish optimal dosing and long-term safety.
Realistic Expectations and Clinical Considerations
Setting appropriate expectations represents a crucial aspect of supplement-based cholesterol management. Importantly, even the most effective supplements typically achieve LDL reductions of 10-20%, whereas lifestyle modifications can reduce cholesterol by 20-30%. Furthermore, a low-dose statin medication achieved nearly 38% LDL reduction in direct comparison studies.
✅ Before Starting Cholesterol Supplements:
- Consult with healthcare provider about individual cardiovascular risk
- Establish baseline cholesterol levels through laboratory testing
- Review current medications for potential interactions
- Consider dietary and lifestyle modifications as primary interventions
- Evaluate supplement quality and third-party testing credentials
- Plan for follow-up monitoring to assess effectiveness
Individual responses to supplements vary dramatically based on genetics, baseline cholesterol levels, diet, and other factors. Consequently, what works effectively for one person may produce minimal results for another. Moreover, supplement quality varies significantly across manufacturers, making product selection critically important for achieving consistent results.
Integration with Lifestyle Interventions
The most effective cholesterol management approaches combine evidence-based supplements with comprehensive lifestyle modifications. Specifically, dietary changes emphasizing plant-based foods, soluble fiber, and healthy fats create synergistic effects with supplement interventions. Additionally, regular physical activity enhances supplement effectiveness through multiple mechanisms, including improved cholesterol particle metabolism.
“The wonderful news is that heart disease is 90% preventable. There are ways to manage high cholesterol, and even if you can’t do it with diet and exercise, there are amazing medications available.”
Successful cholesterol management requires sustained commitment to multiple interventions rather than relying solely on supplements. Furthermore, Mayo Clinic emphasizes that diet and exercise are proven ways to reduce cholesterol, with supplements serving as potential adjuncts. Nevertheless, supplements should never replace established medical interventions when significant cardiovascular risk exists.
Safety Considerations and Monitoring
Safety considerations become paramount when using cholesterol-lowering supplements, particularly for individuals with existing health conditions or those taking medications. Many supplements can interact with prescription drugs, potentially altering their effectiveness or increasing side effect risks. Moreover, some supplements require periodic monitoring to detect potential adverse effects on liver function or other organ systems.
Pregnant and breastfeeding women should exercise particular caution with cholesterol supplements, as safety data for these populations remains limited. Similarly, individuals with diabetes must carefully monitor blood glucose levels when using certain supplements that may affect glucose metabolism. Furthermore, those with bleeding disorders should avoid supplements that might increase bleeding risk.
The Future of Cholesterol Supplementation
Emerging research continues to explore novel compounds and delivery systems for cholesterol management through supplementation. Notably, scientists are investigating personalized approaches based on genetic profiles that might predict individual responses to specific supplements. Additionally, advances in nutraceutical formulation may enhance bioavailability and effectiveness of existing compounds.
However, the fundamental challenge remains translating modest cholesterol improvements into meaningful cardiovascular risk reduction. Consequently, future research must focus on clinical outcomes rather than solely laboratory values. Moreover, regulatory frameworks may evolve to provide better quality control and standardization for cholesterol-lowering supplements.
Making Informed Decisions
Choosing appropriate cholesterol supplements requires careful evaluation of individual circumstances, risk factors, and treatment goals. Initially, individuals should work with healthcare providers to assess overall cardiovascular risk and determine whether supplements represent an appropriate intervention. Subsequently, those pursuing supplement-based approaches should prioritize evidence-based options with established safety profiles.
Cost-effectiveness considerations also influence supplement selection, as some options require significant ongoing expenses for modest benefits. Furthermore, individuals should remain realistic about supplement limitations while maintaining focus on proven interventions like dietary modification and regular exercise. Ultimately, successful cholesterol management typically requires comprehensive approaches rather than single interventions.
References
- National Center for Complementary and Integrative Health. High Cholesterol and Natural Products: What the Science Says.
- National Center for Complementary and Integrative Health. 8 Tips: High Cholesterol and Dietary Supplements.
- Barrat E, et al. LDL-cholesterol lowering effect of a new dietary supplement: an open label, controlled, randomized, cross-over clinical trial. BMC Complement Altern Med. 2018.
- American Heart Association. 6 common “heart-health” supplements ineffective at lowering cholesterol compared to statins. 2022.
- Mayo Clinic. Cholesterol-lowering supplements may be helpful. 2022.
- Cleveland Clinic. Cleveland Clinic Trial Finds Six Widely Used Dietary Supplements Do Not Lower Cholesterol. 2022.
- Cleveland Clinic. Plant Sterols: How They Help Manage Cholesterol. 2022.
- Grant JK, et al. Supplements for Lipid Lowering: What Does the Evidence Show? Curr Atheroscler Rep. 2023.
- Houston MC. The Role of Nutraceutical Supplements in the Treatment of Dyslipidemia. J Clin Hypertens. 2012.
- Cleveland Clinic. Why Taking Niacin for Cholesterol May Be Harmful. 2024.
- Related
- High Cholesterol: Complete Guide to Understanding and Managing High LDL Levels
- The Ultimate Guide to Natural Diabetes Support
- Plant Sterols: Natural Effective Supplements for Cholesterol
- Can Oatmeal Lower Cholesterol? The Science Behind Oats vs. Statins
- Which is Better for Diabetes, Berberine or Metformin?
Author Bio
The Remedy Verified Team translates complex metabolic science into clear, practical strategies for everyday health. About The Author
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider before starting any supplement regimen or making changes to your cholesterol management plan. Individual results may vary, and supplements should not replace prescribed medications without medical supervision.