You’ve blown your nose and noticed green mucus staring back at you. Does this mean bacterial infection? Do you need antibiotics? Should you call your doctor today or wait it out? These questions matter because the answer determines your next steps—and honestly, common advice often conflicts.
Here’s what makes this confusing: you’ve probably heard “green means bacterial infection,” but research shows 80-90% of green snot actually comes from viral infections that won’t respond to antibiotics. The green color signals your immune system is actively working—white blood cells and iron-containing enzymes create that characteristic hue—but color alone can’t reveal whether you’re dealing with a virus or bacteria. That gap between popular belief and clinical reality leaves people genuinely uncertain about when to act.
This guide translates the evidence into a practical decision framework. You’ll learn what green phlegm actually indicates, how to distinguish bacterial from viral patterns, specific criteria for when to contact your provider versus monitoring at home, and which relief strategies have supporting data. We’ll acknowledge where the science is mixed and emphasize coordination with your care team for any treatment decisions. By the end, you’ll have a clear protocol—not marketing promises.
What Does Green Mucus Mean?
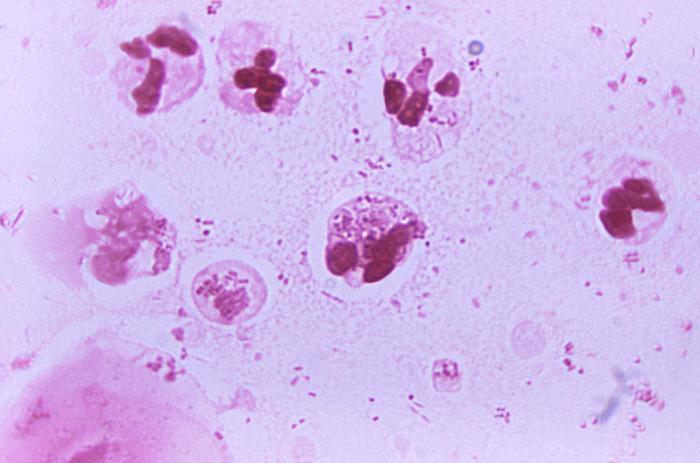
Green mucus occurs when white blood cells and myeloperoxidase—an iron-containing enzyme—accumulate in nasal discharge during immune response. The green color signals active inflammation from either viral or bacterial sources, not infection severity. Most green mucus comes from viral infections that resolve without antibiotics within 7-10 days.
80-90% of green mucus originates from viral infections that will resolve without antibiotics—duration and symptom trajectory matter far more than color intensity.
The progression typically follows a pattern. Clear mucus appears first when irritation begins, then shifts to yellow as white blood cells arrive to fight the trigger. When those white blood cells break down and release myeloperoxidase, the iron in this enzyme creates that characteristic green hue. Think of it as your immune system’s work product—the color indicates activity level, not necessarily what type of invader you’re fighting.
This distinction matters. The widespread belief that “green equals bacterial infection requiring antibiotics” leads to unnecessary prescriptions and contributes to antibiotic resistance. Clinical research shows mucus color alone can’t distinguish bacterial from viral causes. Your provider needs additional clinical findings—symptom duration, fever patterns, facial pain characteristics, examination results—to make that determination.
Here’s something counterintuitive: green snot or green phlegm doesn’t automatically mean you’re more contagious. The early phase of respiratory infections, when mucus is still clear and runny, typically represents peak contagion. By the time secretions turn green, viral shedding often decreases even as the visible immune response becomes more dramatic.
Why Your Mucus Changes from Clear to Yellow to Green

Understanding the color progression helps you interpret what your body’s doing. Normal, healthy mucus is clear and thin—mostly water with proteins, antibodies, and electrolytes that lubricate your respiratory tract and trap particles before they reach your lungs.
When your nasal passages detect irritants—viral particles, bacteria, allergens, pollutants—inflammation begins. Blood vessels dilate to deliver more immune cells. Mucus production increases to flush out invaders. Initially this surge appears as abundant clear discharge, the familiar “runny nose” that starts most colds.
Within 24-48 hours, your immune system recruits neutrophils (white blood cells) to the infection site. As neutrophils accumulate, the discharge becomes cloudier and shifts toward yellow. You’re literally seeing your immune response in action—the yellow coloring comes from the sheer number of white blood cells.
The shift from yellow to green happens as neutrophils break down and release myeloperoxidase, a green-pigmented enzyme containing iron that helps destroy pathogens. When large numbers of these cells die and release this enzyme, mucus takes on that distinctive green color. Thicker, darker green typically means higher concentrations of cellular debris—not necessarily a more dangerous infection.
This progression usually unfolds over 2-5 days. Here’s what matters: the timeline, not color intensity. If you’re trending toward improvement (even with green mucus present), your immune system is winning. If symptoms worsen or plateau beyond 7-10 days, that pattern warrants provider evaluation regardless of mucus color.
Green Mucus: When to Wait vs When to Call Your Doctor
The clinical question isn’t “do I have green mucus?” but rather “does my overall pattern suggest I need intervention?” Color alone won’t answer that. You need a framework considering duration, trajectory, and accompanying symptoms together.
Wait-and-Monitor Criteria: You can safely observe at home when green mucus is your primary symptom, you’re less than 10 days into illness, other symptoms remain mild to moderate, and you notice gradual improvement—even if slow. Most viral upper respiratory infections follow this path. Continue basic supportive measures: adequate hydration, rest, saline nasal irrigation if tolerated, and symptom relief as needed.
Contact Your Provider: Reach out for guidance if green discharge persists beyond 10 days without improvement. Also contact them if you develop high fever (above 101.5°F) lasting more than 3 days, experience severe one-sided facial pain or pressure, or notice the “double-worsening” pattern—initial improvement followed by sudden deterioration. These indicators suggest you may benefit from medical evaluation and possible intervention.
Urgent Care Situations: Some symptoms demand prompt attention. Seek medical care if you develop difficulty breathing or shortness of breath, severe headache with neck stiffness, vision changes or eye swelling, altered mental status, or uncontrolled nose bleeding. These extend beyond typical upper respiratory infections and require timely professional assessment.
Set a mental stopwatch when green mucus first appears. Use 7-10 days as your monitoring window. Not clearly improving by day 10? Schedule a provider visit even if symptoms seem tolerable. This time-boxed approach prevents both premature antibiotic use and delayed treatment of bacterial infections needing medication. Track your symptom trajectory daily—not just mucus color—to give your clinician useful data if evaluation becomes necessary.
⚠️ Important: Coordinate any changes with your care team, especially if you have underlying conditions like asthma, COPD, or immunocompromise. Your baseline health status influences both risk assessment and treatment thresholds. What represents “watch and wait” for otherwise healthy adults may require earlier intervention for people with complicating factors.
How to Tell if Your Green Mucus Is Bacterial or Viral
Here’s the frustrating truth: you can’t definitively distinguish bacterial from viral causes by examining your mucus at home. Research consistently shows that color, consistency, and even odor fail as reliable diagnostic markers. A 2016 systematic review in BMJ found that purulent (green or yellow) nasal discharge predicted bacterial infection no better than chance. Your immune system produces the same colored response whether fighting rhinovirus or Streptococcus pneumoniae.
That said, clinical patterns can shift probability. Understanding these patterns helps you communicate effectively with your provider and make informed decisions about when evaluation makes sense versus continued home monitoring.
Key Insight: Most green mucus (80-90%) originates from viral infections, but the duration and trajectory matter more than color intensity for determining infection type.
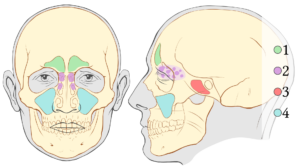
Bacterial Probability Increases With: Symptom duration exceeding 10 days without improvement signals possible bacterial sinusitis—though even this threshold isn’t absolute. The “double-worsening” pattern carries more weight: initial improvement followed by sudden deterioration around day 5-7 suggests a secondary bacterial infection complicating a viral illness. Unilateral facial pain or pressure concentrated over specific sinuses, fever persisting beyond 3-4 days, or severe symptoms from onset also tilt the probability scale.
Viral Patterns Usually Show: Gradual improvement despite persistent green color—you feel incrementally better each day even if mucus remains discolored. Viral infections commonly accompany sore throat, general body aches, and cough, with symptoms peaking around days 3-5 before declining. Yellow-green mucus during this transition phase is typical as your immune response winds down. Bilateral (both sides) congestion rather than focused pressure points suggests viral rhinosinusitis rather than bacterial sinusitis.
Here’s the clinical nuance: acute rhinosinusitis (inflammation of nasal passages and sinuses) is almost always viral and doesn’t require antibiotics. True bacterial sinusitis requires both prolonged symptoms AND blockage of the ostia—small openings connecting sinuses to nasal passages. When those openings remain patent (open), bacteria can’t establish the anaerobic environment needed to cause infection. Your provider’s examination, not home observation, determines this distinction.
“The color of mucus doesn’t indicate whether you need an antibiotic. Duration and progression tell us much more about bacterial involvement.”
— Dr. Michael Benninger, Chairman of Otolaryngology at Cleveland Clinic
The antibiotic decision involves weighing modest potential benefit against real risks: side effects, drug interactions, disruption of healthy gut microbiome, and contribution to antibiotic resistance. Current clinical guidelines recommend antibiotics only when bacterial infection probability justifies intervention—typically symptoms beyond 10 days or severe presentation from onset. Even then, some bacterial sinus infections resolve without antibiotics given sufficient time.
If your provider prescribes antibiotics, set clear expectations together. Define what improvement should look like and when. Establish stop criteria if side effects emerge. Commit to completing the prescribed course if you do start—half-finished antibiotic courses contribute more to resistance than never starting at all.
What Actually Helps Green Mucus Resolve Faster
No intervention makes viral infections disappear overnight—your immune system needs time to clear the pathogen, typically 7-14 days total. But evidence supports specific approaches that can reduce symptom burden and potentially shorten duration. The key? Match your effort to the strength of supporting data rather than chasing every marketed solution.

Proven Approaches with Strong Evidence: Nasal saline irrigation stands out with the most consistent research support. Multiple randomized trials show that flushing nasal passages with isotonic or hypertonic saline 2-3 times daily reduces symptom severity and potentially shortens illness duration by 1-2 days. The mechanism is straightforward: physical removal of mucus, inflammatory mediators, and viral particles from nasal tissues. Use distilled, sterile, or previously boiled water—never tap water—to avoid rare but serious infections.
Evidence Hierarchy: Prioritize interventions with reproducible clinical trial data (saline irrigation, hydration) over those with only mechanistic rationale or weak observational support.
Adequate hydration supports normal mucus consistency and mucociliary clearance—the process by which tiny hairs (cilia) in your respiratory tract sweep mucus and trapped particles toward your throat for removal. Aim for 1.5-2 liters daily from water, herbal tea, or clear broth. You’ll know you’re adequately hydrated when urine is pale yellow; dark urine suggests you need more fluid intake.
Supporting Evidence for Symptom Relief: Steam inhalation provides temporary symptom relief for many people, though data on speeding resolution are limited. If it helps you feel better, use it—just avoid scalding temperatures that could burn respiratory tissues. Warm compresses over sinuses may reduce facial discomfort through vasodilation and muscle relaxation, though again, this treats symptoms rather than shortening illness.
Mixed or Limited Evidence: Guaifenesin (found in Mucinex and generics) thins mucus theoretically, but clinical trials show inconsistent results. Some users report subjective benefit; others notice no difference from placebo. According to pulmonologist Dr. Subinoy Das, “Expectorants like guaifenesin have weak evidence for acute infections—hydration may accomplish the same thinning effect.” If you try it, set a 3-5 day trial window and discontinue if you see no measurable benefit.
Eucalyptus oil in topical preparations may provide aromatic comfort and mild anti-inflammatory effects, but robust data supporting faster mucus clearance don’t exist. Zinc lozenges show mixed results—some trials suggest modest reduction in cold duration if started within 24 hours of symptom onset, while others find no effect. Quality and dosing vary widely between products, making recommendations difficult.
Coordinate Before Adding Supplements: If you take prescription medications, check with your provider or pharmacist before adding even over-the-counter supplements. Interactions exist: zinc can reduce absorption of antibiotics, high-dose vitamin C may interact with blood thinners, and herbal preparations often carry unpredictable drug interaction profiles. This coordination prevents well-intentioned self-treatment from causing new problems.
The evidence-based core remains simple: saline irrigation, adequate hydration, rest when your body signals fatigue, and time for your immune system to complete its work. Additional measures may provide comfort—and comfort has value—but distinguish symptomatic relief from actual disease modification. Most marketed “immune support” supplements lack the quality evidence needed to justify routine use during acute infections.
Green Mucus Myths: What the Evidence Actually Shows
The gap between popular belief and clinical evidence around mucus color remains surprisingly wide. These misconceptions lead to unnecessary antibiotic use, premature provider visits, and anxiety about normal immune processes. Let’s examine what research actually supports versus what sounds plausible but lacks backing.
| Myth | What Evidence Shows |
|---|---|
| “Green mucus means bacterial infection requiring antibiotics” | FALSE. Research shows 80-90% of green mucus originates from viral infections. A 2013 study in JAMA Internal Medicine found no correlation between mucus color and bacterial culture results. Duration and symptom trajectory matter far more than color. |
| “You’re most contagious when mucus turns green” | FALSE. Peak contagion typically occurs during the early “clear runny nose” phase when viral shedding is highest. By the time secretions turn green, you’re usually past maximum infectivity even though symptoms look worse. |
| “Darker green means more serious infection” | MIXED. Darker color indicates higher concentration of white blood cells and myeloperoxidase—cellular activity level, not pathogen severity. Morning mucus often appears darker simply because it’s been accumulating overnight, not because infection worsened. |
| “Green mucus automatically means sinusitis” | FALSE. Acute rhinosinusitis (nasal and sinus inflammation) is almost always viral and doesn’t constitute true bacterial sinusitis. True sinusitis requires ostia blockage trapping bacteria in an anaerobic environment—a clinical diagnosis you can’t make by looking at tissues. |
| “Green phlegm from lungs is more serious than green nasal mucus” | CONTEXT-DEPENDENT. Lower respiratory tract infections producing green sputum may warrant different evaluation thresholds, especially with fever, shortness of breath, or chest pain. But color alone still can’t distinguish bacterial from viral bronchitis—provider examination required. |

The persistence of these myths reflects a pattern: humans seek simple diagnostic rules. “Green equals bacterial equals antibiotics” provides false certainty in an uncertain situation. But clinging to inaccurate heuristics leads to poor decisions—antibiotics when you don’t need them, delayed care when you do, or misplaced worry about normal immune function.
The alternative isn’t complexity paralysis. It’s replacing simplistic color-coding with practical decision frameworks based on symptom duration, trajectory, and accompanying findings. That approach takes slightly more thought but produces significantly better outcomes.
Your 10-Day Green Mucus Protocol (Step-by-Step)
This time-boxed monitoring protocol provides structure without overreaction. You’re not ignoring symptoms, but you’re also not rushing to intervention before giving your immune system a fair chance to resolve viral infections naturally. Use this as a decision-support tool, adjusting based on your baseline health and your provider’s guidance if you have complicating conditions.
Protocol Foundation: Most viral upper respiratory infections resolve within 7-10 days. This window allows natural resolution while catching bacterial infections that warrant intervention.

Days 1-3 (Early Phase): Document your starting point—symptoms present, their severity, and when green mucus first appeared. Begin saline nasal irrigation 2-3 times daily using distilled or sterile water. Increase fluid intake to 1.5-2 liters daily. Get adequate rest and consider over-the-counter symptom relief for discomfort (acetaminophen or ibuprofen if tolerated and appropriate for you). Avoid antihistamines unless you have confirmed allergies, as drying mucus can sometimes worsen congestion.
Days 4-7 (Assessment Window): Track your trajectory daily. Ask yourself: “Am I incrementally better than yesterday?” Small improvements count—even if green mucus persists, you’re looking for reduced congestion, easier breathing, less facial pressure, declining fever, or improved energy. Continue saline irrigation and hydration. If you plateau (neither better nor worse) but remain within tolerable symptom range, continue monitoring through day 10. If you’re clearly worsening—new fever, increasing pain, spreading symptoms—contact your provider without waiting.
Days 8-10 (Decision Point): Not noticeably improving by day 8-10? Schedule a provider visit even if symptoms seem manageable. Persistent symptoms beyond 10 days shift bacterial probability upward enough to warrant professional evaluation. Bring your symptom diary: when symptoms started, how they’ve progressed, what you’ve tried, and current medication list. This data helps your provider make efficient, accurate assessments.
Beyond Day 10 (Provider Evaluation): Your clinician will examine you, possibly including nasal endoscopy or sinus imaging if presentation suggests complicated infection. They’ll weigh whether antibiotics offer sufficient benefit-to-risk ratio for your specific situation. If antibiotics are prescribed, ask: “What improvement should I expect, and by when? What would indicate I should call back?” Clear outcome expectations prevent both premature discontinuation and prolonged ineffective treatment.
Special Circumstances Modifying the Protocol: Immunocompromise, uncontrolled diabetes, asthma, COPD, cystic fibrosis, or recent surgery may warrant earlier evaluation—sometimes days 5-7 rather than day 10. Heart valve abnormalities or indwelling medical devices can change infection risk calculations. Discuss your baseline risk factors with your provider in advance of acute illness so you have a personalized threshold ready when needed.
This structured approach balances appropriate caution with avoiding reflexive antibiotic use. You’re applying clinical reasoning to home monitoring—the same framework your provider uses, adapted for patient application. Most people following this protocol will watch their symptoms resolve without intervention. Those who do need antibiotics will receive them at the right time with clear justification, not based on mucus color alone.
Moving Forward With Green Mucus: Evidence Over Anxiety
Green mucus doesn’t signal emergency or automatic antibiotic need—it reveals your immune system actively working through inflammation. Understanding the mechanism behind the color shift transforms a source of worry into information you can interpret rationally within a broader clinical context.
The key insights that separate evidence-based management from common misconceptions? Color alone can’t distinguish bacterial from viral infections. Duration and trajectory matter far more than shade intensity. Most green mucus resolves without intervention within 10 days.
Your immediate next step: if you currently have green mucus, mark today as day one of your monitoring protocol. Document baseline symptoms, start saline irrigation, ensure adequate hydration, and set your day-10 checkpoint. Track trajectory daily using “better than yesterday” as your metric. Beyond day 10 or experiencing severe symptoms? Contact your provider with the structured information you’ve gathered. You now have a framework that replaces guesswork with clinical reasoning—and that clarity improves outcomes.
Frequently Asked Questions About Green Mucus
Does green mucus always mean I have an infection?
Not always. Green mucus indicates active immune response with white blood cell accumulation, but doesn’t always signal infection. Allergies, irritants, or normal immune surveillance can sometimes produce colored discharge. Duration matters more than color—if symptoms resolve within 3-5 days, infection may never have established.
Can COVID-19 cause green mucus?
Yes. COVID-19 can produce green mucus like other viral respiratory infections. Color won’t distinguish COVID from cold or flu. If you have green mucus alongside fever, loss of taste/smell, or significant breathing difficulty, test for COVID-19 to guide isolation decisions and treatment eligibility.
Should I exercise with green mucus?
Use the “neck check” rule: symptoms above the neck (runny nose, mild congestion) usually permit light exercise if you feel up to it. Symptoms below the neck (chest congestion, body aches, fever) warrant rest. Listen to your body—fatigue signals your immune system needs energy directed toward healing, not performance.
Is green phlegm from coughing different than green nasal mucus?
Green sputum from your lungs (productive cough) may indicate bronchitis or pneumonia, especially with fever, chest pain, or shortness of breath. While similar immune mechanisms create the color, lower respiratory symptoms warrant closer monitoring and possibly earlier provider evaluation than isolated nasal discharge.
References
- Benninger MS, et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngology–Head and Neck Surgery. 2003. PubMed
- Ashworth M, et al. Antibiotic prescribing and patient satisfaction in primary care in England. British Journal of General Practice. 2016. PMC
- Arroll B, Kenealy T. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database of Systematic Reviews. 2013. Cochrane Library
- King D, et al. Saline nasal irrigation for acute upper respiratory tract infections. Cochrane Database of Systematic Reviews. 2015. Cochrane Library
- Cleveland Clinic. Mucus: Phlegm, Causes, Colors & How To Get Rid Of It. 2024. Cleveland Clinic
- Rosenfeld RM, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngology–Head and Neck Surgery. 2015. PubMed
- University of Pittsburgh Medical Center. Why Is My Snot Green? Understanding Nasal Mucus Colors. 2024. UPMC HealthBeat
- The Conversation. Health Check: does green mucus mean you’re infectious and need antibiotics? 2025. The Conversation
About the Author
The Remedy Verified team translates complex medical research into practical, evidence-based guidance for managing chronic conditions. With backgrounds bridging clinical interpretation and health communication, we emphasize coordination with medical care rather than replacement approaches. Our content focuses on helping readers make informed decisions through transparent discussions of research quality, realistic expectations, and structured protocols. Learn more about our editorial standards.
Medical Disclaimer
⚠️ Disclaimer: The information provided in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. Green mucus patterns and respiratory symptoms may indicate various conditions requiring professional evaluation. Always consult a qualified healthcare professional before making decisions about your health—especially if you have fever, difficulty breathing, symptoms lasting beyond 10 days, or underlying medical conditions. Remedy Verified does not provide medical services, and the content shared here should not be considered a substitute for professional medical guidance. Individual responses to infections and treatments vary; this article cannot account for your specific medical history, current medications, or unique risk factors. Use of this website and its information is at your own risk.
Related Articles
- Natural Antibiotics: 12 Evidence-Based Options + Safety Guide
- Tonsils and Adenoids: Symptoms, Treatment & When to Worry
- Omega-3 Supplements Guide: Eicosapentaenoic Acid Benefits and Clinical Evidence
- My Ear Won’t Pop: What to Try After Everything Fails
- Cloudy Urine in Women: Causes, When to Worry & What to Do