You’ve noticed excess fat or loose skin above your pubic bone—what many call FUPA (fatty upper pubic area)—and you’re wondering if it’s normal, why it’s there, and whether diet and exercise will actually work. The reality: it’s more common than you think, and the solutions depend entirely on whether you’re dealing with fat, loose skin, or both.
This guide differs from generic FUPA articles because we won’t sell you on “targeted exercises” that can’t work or ignore the fact that genetics and hormones largely determine where your body stores fat. You’ll get evidence-based answers on what causes pubic area fat accumulation, realistic expectations for lifestyle changes, and honest assessments of when medical intervention becomes necessary.
Whether you’re dealing with postpartum changes, weight loss aftermath, or your body’s natural fat distribution pattern, you’ll learn why your pubic area looks the way it does and what your real options are—no fitness industry myths, just verified information for informed decisions.
What Is FUPA? (The 60-Second Answer)

FUPA (fatty upper pubic area) refers to fat accumulation above the pubic bone in the mons pubis region. It’s anatomically normal—this fatty cushion protects your pubic bones. However, excess fat or loose skin here can develop from genetics, pregnancy, significant weight changes, or aging, affecting both men and women.
The mons pubis naturally contains protective fat covered by skin and pubic hair. Problems arise when this area becomes noticeably enlarged from weight gain, hormonal shifts, or skin elasticity loss after pregnancy or major weight loss.
Critical reality: you cannot spot-reduce fat from your pubic area through targeted exercises. Your body decides where it stores and loses fat based on genetics and hormones. Those “FUPA-melting exercises” online might strengthen your core but won’t specifically eliminate fat from this region.
You have legitimate options: overall body fat reduction through sustainable calorie deficit, or medical interventions like liposuction, monsplasty (pubic lift), or abdominoplasty (tummy tuck). The right approach depends on whether you’re dealing with excess fat, loose skin, or both—and your individual biology’s response to lifestyle changes.
Why Your Body Stores Fat in the Pubic Area (And Why It’s Normal)
Your mons pubis exists for a reason. This fatty pad sits directly over your pubic bones (specifically where the two halves of your pelvis meet at the pubic symphysis) and serves as natural cushioning during physical activities, including sexual intercourse. Some fat here is protective and healthy.
The problem starts when your body stores significantly more fat in this area than the baseline protective amount. And this is where individual biology becomes critical: genetic factors determine not just how much total body fat you carry, but specifically where your body preferentially stores it.
Research on fat distribution patterns shows that some people are genetically predisposed to store excess fat in the lower abdominal and pubic regions, regardless of their overall body weight. This explains why you can be at a healthy BMI and still have a pronounced FUPA, or why some individuals who lose substantial weight everywhere else still retain fat above their pubic bone.
Hormones play an equally significant role. Estrogen influences fat deposition patterns in women, particularly in the hips, thighs, and pubic area. As estrogen levels fluctuate during pregnancy, perimenopause, and menopause, fat distribution shifts—often increasing in the abdominal and pubic regions. For men, declining testosterone levels with age can similarly alter where the body stores fat, making the pubic area more prominent.
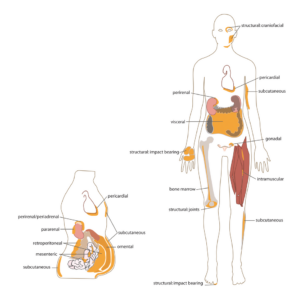
The medical distinction matters: FUPA refers to fat and loose skin in the mons pubis area (also called the pubic mound), while “panniculus” or “apron belly” describes hanging skin and fat extending from below the belly button down over the pubic area. These are related but distinct conditions requiring different treatments.
7 Science-Backed Causes of FUPA (Beyond “Just Lose Weight”)
Understanding why FUPA develops in your specific case matters because the cause influences which solutions will actually work. Here are the evidence-based reasons fat accumulates or skin becomes loose in your pubic area.
1. Genetic Fat Distribution Patterns
Your genes determine where your body preferentially stores fat. Some people store it predominantly in their thighs and buttocks (gynoid distribution), others in their abdomen (android distribution), and many store significant amounts in the pubic region regardless of overall body composition. You can’t change your genetic blueprint through lifestyle modifications alone.
This explains the frustrating reality of being relatively lean everywhere except your pubic area. Your body isn’t malfunctioning—it’s following its genetic programming for fat storage location.
2. Pregnancy and Postpartum Changes
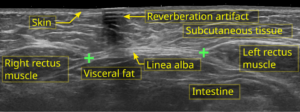
Pregnancy causes multiple permanent changes to your abdominal and pelvic anatomy. Your body naturally accumulates fat in the pubic area to support fetal development. Your abdominal muscles separate (diastasis recti), your skin stretches dramatically, and your pelvic floor weakens.
After delivery, some of these changes reverse partially or completely, but many don’t. The fat accumulated during pregnancy may persist. The stretched skin may lack sufficient elasticity to fully retract. The separated abdominal muscles may not return to their pre-pregnancy position, altering how your lower abdomen and pubic area appear.
C-section deliveries add another layer: scar tissue formation can create adhesions that change the appearance and contour of your lower abdomen and pubic mound. This surgical scar tissue doesn’t behave like normal tissue and can contribute to a more pronounced FUPA appearance.
3. Significant Weight Loss
Losing substantial weight—particularly 50 pounds or more—is an impressive health achievement. But it often leaves excess skin that won’t “snap back” no matter how much weight you lose or how fit you become.
Skin elasticity decreases with age, duration of obesity, and the amount of weight carried. If you were significantly overweight for years, your skin stretched to accommodate that size. Once the fat is gone, the stretched skin remains. In the pubic area, this creates a hanging or sagging appearance that diet and exercise cannot fix because it’s not fat—it’s loose skin.
4. Hormonal Changes
Hormones dictate where your body stores fat and how efficiently it mobilizes stored fat for energy. Multiple hormonal shifts can increase pubic area fat:
Menopause causes estrogen levels to drop, shifting fat storage from hips and thighs to the abdomen and pubic region. Male aging reduces testosterone, which similarly alters fat distribution toward the midsection and pubic area. Cortisol elevation from chronic stress signals your body to store fat preferentially in the abdominal region, including the pubic mound.
Polycystic ovary syndrome (PCOS) creates hormonal imbalances that promote central obesity, including pubic area fat accumulation. Thyroid disorders slow metabolism and can contribute to overall weight gain that includes the pubic region.
5. Natural Aging Process
Aging brings multiple changes that contribute to FUPA development. Your metabolism naturally slows, making it easier to gain fat and harder to lose it. Muscle mass decreases, reducing your body’s baseline calorie burn. Skin loses collagen and elasticity, making it more prone to sagging.
Fat distribution patterns shift even if your weight stays constant. The fat you carried in your thighs at 25 might relocate to your abdomen and pubic area by 55.
6. Weight Fluctuations
Repeated cycles of weight gain and loss (yo-yo dieting) damage skin elasticity more than maintaining a steady weight—even if that steady weight is higher. Each time your skin stretches and contracts, it loses some elastic fibers. Eventually, it won’t fully retract after fat loss.
The pubic area is particularly vulnerable because skin there is relatively thin and subjected to significant stretching during weight gain.
7. Post-Surgical Changes
Previous abdominal surgeries can contribute to FUPA in unexpected ways. A tummy tuck that removes fat and tightens skin above the pubic area but doesn’t address the mons pubis itself can make the pubic mound appear more prominent by comparison.
If you gain weight after a tummy tuck that removed fat cells from your abdomen, your body might preferentially store new fat in the untreated pubic area simply because there are more fat cells remaining there. It’s not that the surgery caused FUPA, but it can alter fat distribution patterns in a way that makes the pubic area more noticeable.
Evidence-Based FUPA Reduction: Separating Facts from Fitness Industry Fiction
Let’s address the most marketed myth first: you cannot spot-reduce fat from your pubic area through targeted exercises. This isn’t opinion—it’s established physiology. Your body mobilizes fat for energy from all storage sites simultaneously, prioritizing areas based on genetics and hormonal signals, not which muscles you’re exercising.
The same principle applies to your pubic area: strengthening your lower abs through planks and leg raises might build muscle definition, but it won’t specifically eliminate FUPA.
The fitness industry sells targeted FUPA exercises because it’s easier than admitting the truth: general fat loss requires consistent calorie deficits maintained over months, and even then, your pubic area might be the last place you lose fat—or you might never fully lose it there due to genetic fat distribution patterns.
What Overall Fat Loss Can (and Can’t) Achieve
Creating a calorie deficit through diet modifications and increased physical activity can reduce total body fat. For some people, this will noticeably reduce FUPA. For others, it won’t—at least not proportionally to fat loss elsewhere.
Here’s the critical variable: whether your FUPA is primarily fat or primarily loose skin. If you’re carrying excess fat throughout your body, overall fat loss will likely reduce the pubic area somewhat. But if you’ve already lost significant weight and you’re dealing with stretched skin rather than fat, no amount of additional fat loss will tighten that skin.
Realistic timeline expectations matter. If lifestyle changes are going to work for your FUPA, you’re looking at a minimum of 6-12 months of consistent effort before seeing noticeable changes. Your pubic area will likely be one of the last places you see fat reduction because it’s often where your body preferentially stores fat.
The Skin Elasticity Problem
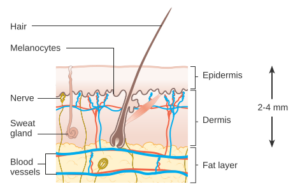
Skin elasticity determines whether fat loss reveals a toned physique or leaves excess sagging skin. Unfortunately, elasticity decreases with age, duration of obesity, smoking, sun exposure, and genetics.
If you’re under 30 and lost weight after a relatively short period of weight gain, your skin might retract reasonably well. If you’re over 40 and lost 80+ pounds after years of obesity, your skin elasticity is likely too compromised to fully bounce back, particularly in areas like the pubic region where skin is thinner and more delicate.
No cream, supplement, or non-invasive treatment will restore lost skin elasticity enough to eliminate significant loose skin. Collagen supplements, retinol creams, and radiofrequency treatments might provide marginal improvements, but they won’t produce the dramatic tightening required to resolve loose skin FUPA.
What Actually Helps: The Honest Assessment
Strength training improves core stability and posture, which may make your lower abdomen appear flatter. But this is muscle tone, not fat reduction—your FUPA remains, just with better underlying support.
Prevention strategies during pregnancy or weight loss can minimize severity: avoid excessive pregnancy weight gain beyond medical recommendations, and lose weight gradually (1-2 pounds weekly) to preserve skin elasticity better than rapid loss.
When Lifestyle Changes Won’t Work
You need to hear this clearly: for some people, diet and exercise will never eliminate FUPA. If you fall into any of these categories, lifestyle modifications might reduce the severity but won’t fully resolve the issue:
- You’ve lost 50+ pounds and have significant loose skin in the pubic area
- You’re over 40 and dealing with age-related skin elasticity loss
- You have genetic fat distribution patterns that concentrate fat storage in the pubic region
- You’ve had multiple pregnancies with substantial abdominal muscle separation
- You’ve had previous abdominal surgeries that altered your anatomy
Acknowledging this isn’t defeatist—it’s realistic. Spending years pursuing natural FUPA reduction when your specific situation requires medical intervention wastes time and creates frustration. Understanding when lifestyle changes have reached their limit lets you make informed decisions about whether medical treatments align with your goals and values.
FUPA Treatment Options: From Non-Invasive to Surgical Solutions
Medical interventions for FUPA range from non-invasive fat reduction technologies to comprehensive surgical procedures. The right option depends on whether you’re dealing with excess fat, loose skin, or both—and how much change you want to achieve.
Non-Surgical Treatments: What the Evidence Actually Shows

CoolSculpting (Cryolipolysis) uses controlled cooling to freeze and destroy fat cells in targeted areas. For FUPA, this means placing applicators on the pubic mound to reduce fat volume without surgery.
Cost: $700-$1,500 per treatment area; most people need 2-3 sessions. Results appear gradually over 2-3 months. Fat reduction is permanent for destroyed cells, but weight gain can enlarge remaining fat cells.
Radiofrequency and laser treatments claim to tighten skin and reduce fat through heat energy. Evidence quality for these claims is mixed at best. A 2017 review in Dermatologic Surgery found radiofrequency treatments produced “modest” skin tightening in some patients, but results were highly variable and far less dramatic than surgical options.
Cost: $2,000-$4,000 for multiple treatment sessions. Realistic expectation: marginal improvement, not transformation. These work best for mild skin laxity, not significant loose skin or substantial fat deposits.
Non-surgical treatments are marketed heavily because they’re profitable, not because they’re highly effective. For mild FUPA, they might provide noticeable improvement. For moderate to severe FUPA, they’re unlikely to produce results you’ll consider worth the cost.
Surgical Options: Permanent Solutions with Trade-offs
Monsplasty (Pubic Lift) specifically targets the mons pubis, removing excess fat and skin while lifting and reshaping the pubic mound. The surgeon makes a horizontal incision along the pubic hairline (similar to a C-section scar location), removes fat and skin, then tightens the remaining tissue.
Who it’s for: People with both excess fat and loose skin in the pubic area, particularly after significant weight loss or multiple pregnancies. Most effective when you’re at or near your goal weight, as future weight fluctuations can compromise results.
Recovery: Plan for 1-2 weeks off work for desk jobs, 3-4 weeks for physically demanding jobs. No sexual activity or strenuous exercise for 4-6 weeks. Swelling persists for 6-8 weeks; final results visible at 3-6 months. Cost: $4,000-$8,000 as a standalone procedure, often less when combined with abdominoplasty.
Permanence: Results are permanent unless you gain significant weight or become pregnant. The removed skin and fat cells don’t regenerate.
Liposuction removes fat through small incisions using a cannula (thin tube) that suctions out fat cells. For pubic area liposuction, surgeons typically use tumescent technique—injecting fluid to minimize bleeding and bruising—then removing fat through tiny incisions in the groin creases.
Critical limitation: Liposuction removes fat but doesn’t address loose skin. If your skin has decent elasticity, it will contract after fat removal. If you have poor skin elasticity (common over age 40 or after significant weight loss), liposuction can worsen the appearance by creating hollow areas or making skin sag more visibly.
Your surgeon should assess skin elasticity before recommending liposuction. If they suggest liposuction despite obvious skin laxity, seek another opinion. Recovery: 3-7 days before returning to work, 2-3 weeks before exercise. Final results at 3-4 months after swelling resolves. Cost: $3,000-$6,000 for pubic area treatment.
Abdominoplasty (Tummy Tuck) addresses the entire lower abdomen, including the pubic area. The surgeon makes a horizontal incision from hip to hip, removes excess skin and fat, tightens separated abdominal muscles, and repositions the remaining tissue.
When combined with specific attention to the mons pubis (which should be standard practice but isn’t always), a tummy tuck can significantly reduce FUPA while creating a flatter overall abdominal profile. Many surgeons recommend combining abdominoplasty with monsplasty or pubic liposuction for comprehensive results.
Recovery is more intensive than isolated monsplasty: 2-4 weeks off work, no heavy lifting or strenuous activity for 6-8 weeks, compression garment worn continuously for weeks. Cost: $8,000-$15,000 depending on technique complexity and geographic location.
Panniculectomy is specifically for removing hanging skin (panniculus) after massive weight loss. Unlike a tummy tuck, which includes muscle tightening and cosmetic contouring, panniculectomy focuses solely on removing excess skin that creates functional problems.
This distinction matters for insurance coverage: panniculectomy may be covered if the hanging skin causes chronic infections, rashes, or mobility limitations. Abdominoplasty for cosmetic purposes is almost never covered. Documentation of medical necessity—photos of rashes, records of infections, physical therapy notes about mobility restrictions—strengthens insurance claims.
Insurance Coverage: When Treatment Might Be Covered
Most FUPA treatments are considered cosmetic and aren’t covered by insurance. However, coverage is possible when you can document medical necessity:
Chronic or recurrent skin infections in the folds caused by excess tissue. Documented rashes that don’t respond to conservative treatment. Mobility limitations affecting daily activities. Buried penis in men causing urinary dysfunction or hygiene difficulties.
You’ll need extensive documentation: photos, dermatology records, failed conservative treatment attempts (prescription creams, weight loss efforts), and sometimes letters of medical necessity from multiple providers. Even with documentation, approval isn’t guaranteed. Many insurers require proof that you’ve maintained stable weight for 6-12 months before approving surgical intervention.
Gender-Specific Considerations
Women typically develop FUPA after pregnancy or during menopause due to hormonal fat redistribution. Treatment often addresses stretched abdominal muscles (diastasis recti) alongside pubic area concerns. Timing matters: if you plan future pregnancies, wait until you’re done having children before pursuing surgical treatment.
Men may develop “buried penis” when pubic fat obscures the penis, making it appear shorter and creating functional urinary difficulties. This condition creates both cosmetic and medical concerns. Treatment priorities differ: reducing the pubic fat pad to restore normal penile appearance and function, rather than aesthetic contouring alone.
Medical Concerns: When FUPA Needs Professional Attention
Most FUPA discussions focus exclusively on appearance, but there are legitimate medical reasons to seek professional evaluation. Here’s how to distinguish between a cosmetic concern you can address on your own timeline and a medical issue requiring intervention.
Physical Symptoms Requiring Medical Attention
Seek medical evaluation if you experience any of these issues:
Chronic or recurrent skin infections in the folds of the pubic area that don’t resolve with improved hygiene and over-the-counter treatments. You’re looking for patterns: infections that keep returning despite treatment, or rashes that persist for weeks. Document these with photos and dates—you’ll need this evidence if you pursue insurance coverage for treatment.
Persistent rashes, sores, or skin breakdown where skin folds rub together. The constant moisture and friction in these areas creates an environment prone to fungal infections, bacterial infections, and skin maceration (tissue breakdown from excessive moisture). If topical treatments don’t resolve these within 2-3 weeks, you need medical assessment.
Mobility limitations affecting daily activities. Can you walk comfortably? Bend over to tie shoes? Exercise without the pubic area causing pain or significant restriction? If excess tissue physically interferes with movement, that crosses from cosmetic to functional impairment.
Hygiene difficulties making it challenging to adequately clean the area. This isn’t about mild inconvenience—it’s about whether the anatomy prevents proper hygiene despite reasonable effort, creating ongoing infection risk.
Buried Penis: A Male-Specific Medical Concern
For men, buried penis represents a distinct medical condition where excess pubic fat obscures the penis, creating both functional and psychological consequences. Medical criteria include difficulty urinating while standing, recurrent urinary tract infections, difficulty achieving or maintaining erections, pain during erections, or inability to have penetrative intercourse.
This isn’t vanity—it’s legitimate urological dysfunction. If you’re experiencing these symptoms, consult a urologist, not just a plastic surgeon. Treatment might involve coordinated care between urology and plastic surgery specialties.
Psychological Impact: When It Becomes a Quality of Life Issue
Body image concerns exist on a spectrum from mild preference (“I wish this looked different”) to severe distress affecting daily functioning and mental health. Here’s how to assess where you fall:
Mild concern: You notice your FUPA and would prefer it looked different, but it doesn’t significantly impact your life choices, relationships, or emotional state. Moderate concern: You actively avoid certain clothing, situations (swimming, intimacy), or activities because of self-consciousness about your pubic area. This creates some life restrictions but isn’t overwhelming. Severe distress: Thoughts about your FUPA dominate your mental energy, you avoid relationships or intimacy entirely because of it, you experience anxiety or depression directly linked to this concern, or you’re engaging in extreme behaviors trying to fix it.
Severe distress warrants professional mental health support alongside any physical treatments you pursue. Body dysmorphic disorder (BDD) can fixate on any body part, including the pubic area. If surgical intervention won’t address the underlying psychological pattern, it won’t resolve your distress—and you might develop fixation on a different perceived flaw post-surgery.
A qualified therapist can help you determine whether your distress is proportional to the physical reality and whether pursuing treatment aligns with healthy motivations. This isn’t about talking you out of treatment—it’s about ensuring treatment actually improves your quality of life.
Questions to Ask Your Doctor
When consulting a physician about FUPA, come prepared with specific questions that reveal their expertise and approach:
- “What’s causing my specific FUPA—excess fat, loose skin, or both?” This determines appropriate treatment. If a surgeon recommends liposuction without assessing skin quality, that’s a red flag.
- “What are realistic outcomes for my age, skin quality, and anatomy?” Beware promises of perfection. Realistic surgeons discuss limitations alongside benefits.
- “What happens if I gain weight after treatment? Or become pregnant?” Understanding result durability matters for informed decision-making.
- “What are the specific risks for someone with my medical history?” Generic risk discussions aren’t sufficient. How do your particular health conditions affect complication rates?
- “How many of these specific procedures have you performed?” You want a surgeon who regularly performs the exact procedure you’re considering, not just general plastic surgery experience.
Finding Qualified Specialists
Board certification matters: look for American Board of Plastic Surgery certification for surgical procedures. “Cosmetic surgeon” isn’t a regulated term—anyone with a medical license can claim it. Verify credentials through official board websites, not the surgeon’s marketing materials.
For non-surgical treatments, expertise varies widely. Dermatologists, plastic surgeons, and medical spas all offer CoolSculpting and radiofrequency treatments, but training and experience differ significantly. Ask about provider-specific experience with pubic area treatments, not just general device experience.
Red flags in consultations: Pressure to decide immediately or “limited time” discount offers. Dismissing your questions or concerns as unimportant. Promising results that sound unrealistic compared to before/after photos. Downplaying risks or recovery requirements. Recommending procedures without thorough examination and assessment.
5 FUPA Myths That Keep You from Real Solutions
The fitness and cosmetic surgery industries have created a mythology around FUPA that obscures evidence-based reality. Let’s dismantle the most persistent and damaging myths.
Myth 1: Targeted Exercises Eliminate FUPA
❌ The Myth
Specific exercises—leg raises, reverse crunches, pelvic tilts—will “melt” or “blast” fat from your pubic area.
✓ The Reality
Spot reduction is physiologically impossible. Your body doesn’t preferentially burn fat from areas you exercise. A comprehensive 2013 review in the Journal of Obesity concluded: “targeted exercise does not preferentially reduce adipose tissue in the trained body part.”
Why this myth persists: The fitness industry profits from selling false hope through exercise programs. It’s psychologically appealing to believe you can control exactly where you lose fat. And strengthening underlying muscles can create a modest visual improvement that gets falsely attributed to fat loss.
What to do instead: If you want to reduce FUPA through natural methods, focus on overall fat loss through calorie deficit and full-body exercise. Your pubic area will reduce if and when your genetics permit, not because you targeted it.
Myth 2: Only Overweight People Get FUPA
❌ The Myth
FUPA is simply a result of being overweight. Lose weight and it disappears.
✓ The Reality
Genetic fat distribution patterns mean some people at healthy body weights store disproportionate fat in the pubic area. Hormonal factors—particularly in perimenopause and menopause for women, or with declining testosterone in aging men—redistribute fat to the pubic region regardless of total body weight.
Post-pregnancy anatomical changes, including permanent muscle separation and stretched skin, create FUPA appearance even in women who return to their pre-pregnancy weight. Previous significant weight loss often leaves loose skin that persists despite current healthy weight.
Individual biology determines fat distribution more than total body weight. You can be lean overall and still have a pronounced FUPA because your body preferentially stores fat there—and that’s a genetic reality, not a personal failure.
Myth 3: FUPA Always Goes Away with Weight Loss
The claim: Weight loss automatically eliminates FUPA.
The reality: Weight loss reduces total body fat, but it doesn’t guarantee proportional reduction in the pubic area. Your body loses fat from storage sites based on genetics, hormones, and metabolic factors you can’t control through willpower.
Furthermore, if your FUPA involves loose skin rather than fat—common after significant weight loss or pregnancy—additional weight loss won’t tighten that skin. You can become dangerously underweight chasing FUPA elimination when the issue is skin laxity, not excess fat.
The data shows this clearly: bariatric surgery patients who lose 100+ pounds often require reconstructive surgery to address excess skin in multiple areas, including the pubic region. Weight loss solved their obesity but created loose skin issues requiring different interventions.
Myth 4: All Non-Surgical Treatments Work Equally Well
The claim: CoolSculpting, radiofrequency, laser treatments, and various other non-invasive options all deliver comparable FUPA reduction.
The reality: Evidence quality varies dramatically across non-surgical treatments. CoolSculpting has the strongest research support, with multiple peer-reviewed studies documenting average fat reduction of 20-25% in treated areas. But even this works only on fat, not skin laxity, and produces modest rather than dramatic results.
Radiofrequency and laser treatments for skin tightening show inconsistent results in research, with most studies reporting “modest improvement” that may or may not be worth the cost to individual patients. Many newer devices and treatments have minimal independent research—just manufacturer-funded studies with obvious bias.
Marketing materials show cherry-picked best-case results. Average outcomes are far less impressive. A treatment that works well for mild FUPA in someone with good skin elasticity might produce negligible results for moderate FUPA with poor elasticity.
Myth 5: FUPA Is Purely Cosmetic
❌ The Myth
FUPA only affects appearance and self-esteem, with no real medical implications.
✓ The Reality
While many FUPA cases are primarily cosmetic concerns, significant excess tissue in the pubic area can create legitimate medical problems: chronic skin infections from moisture and friction, buried penis in men creating urological dysfunction, mobility restrictions affecting physical activity, and hygiene difficulties increasing infection risk.
Mobility restrictions from large panniculus affect physical activity and quality of life. Hygiene difficulties increase infection risk and create practical daily challenges.
Dismissing all FUPA concerns as vanity ignores these functional problems. Conversely, treating purely cosmetic concerns as medical emergencies misrepresents the situation. The distinction matters for insurance coverage, treatment priorities, and realistic outcome expectations.
Context determines whether your FUPA is cosmetic (you’d prefer it looked different but it doesn’t impair function) or medical (it creates physical symptoms requiring treatment). Both are valid concerns, but they lead to different treatment pathways and coverage possibilities.
The Bottom Line on FUPA
FUPA isn’t a personal failure—it’s the result of genetics, hormones, and anatomical changes largely outside your control. Understanding whether you’re dealing with excess fat, loose skin, or both determines which solutions will actually work for your situation.
Your immediate next step: assess honestly whether you have excess fat (feels soft, jiggles, may reduce with weight loss) or loose skin (feels thin, hangs or sags, won’t improve with fat loss). If uncertain, schedule a consultation with a board-certified plastic surgeon for professional assessment—you’re not committing to surgery, just getting clarity. From there, pursue lifestyle modifications if your anatomy suggests they’ll work, or explore medical options if your situation requires them. You now have evidence-based information instead of fitness industry mythology—use it to make decisions aligned with your actual biology.
References
- Vispute SS, Smith JD, LeCheminant JD, Hurley KS. The effect of abdominal exercise on abdominal fat. Journal of Strength and Conditioning Research. 2011;25(9):2559-2564. Available at: https://journals.lww.com/nsca-jscr/fulltext/2011/09000/the_effect_of_abdominal_exercise_on_abdominal_fat.27.aspx
- Zelickson B, Egbert BM, Preciado J, et al. Cryolipolysis for noninvasive fat cell destruction: initial results from a pig model. Plastic and Reconstructive Surgery. 2015;135(6):1691-1700. Available at: https://journals.lww.com/plasreconsurg/fulltext/2015/06000/cryolipolysis_for_fat_reduction_and_body.13.aspx
- Epel ES, McEwen B, Seeman T, et al. Stress and body shape: stress-induced cortisol secretion is consistently greater among women with central fat. Psychoneuroendocrinology. 2000;25(7):645-673. Available at: https://pubmed.ncbi.nlm.nih.gov/16353426/
- Mayo Clinic. Polycystic ovary syndrome (PCOS) – Symptoms and causes. Available at: https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439
- Mayo Clinic. Body dysmorphic disorder – Symptoms and causes. Available at: https://www.mayoclinic.org/diseases-conditions/body-dysmorphic-disorder/symptoms-causes/syc-20353938
- American Board of Plastic Surgery. Find a Surgeon. Available at: https://www.abplasticsurgery.org/
Medical Disclaimer
This article is for informational purposes only and does not constitute medical advice. The information provided should not be used to diagnose or treat any health condition. Always consult with a qualified healthcare provider before making decisions about your health, especially regarding surgical procedures or medical treatments.
Individual results vary based on genetics, age, overall health, and adherence to treatment protocols. No outcomes can be guaranteed. The cost estimates, recovery timelines, and treatment descriptions provided are general ranges and may differ significantly based on your location, provider, and individual circumstances.
This content is not intended to replace professional medical consultation, diagnosis, or treatment. If you have concerns about FUPA or related conditions, schedule an appointment with a board-certified physician for personalized assessment and recommendations.
Image Credits:
- Skin & Subcutaneous Fat Layers diagram — © Cancer Research UK,
Wikimedia Commons,
licensed under CC BY-SA 4.0. - Ultrasonography of Diastasis Recti (annotated) — © User:Domdomegg,
Wikimedia Commons,
licensed under CC BY-SA 4.0.