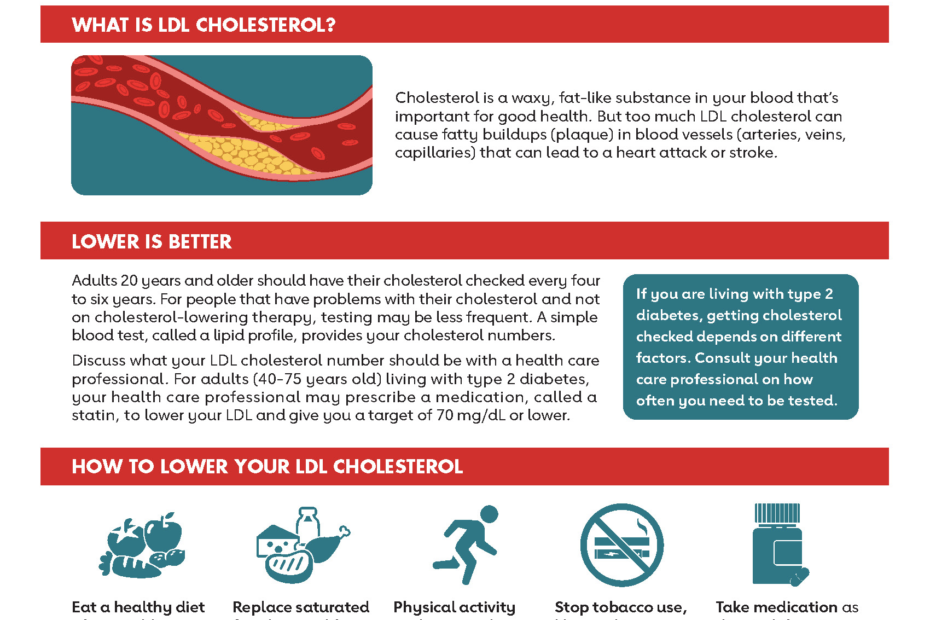
Cholesterol and Type 2 Diabetes: Understanding Diabetic Dyslipidemia and Cardiovascular Risk
🎯 Key Takeaway
The relationship between cholesterol and type 2 diabetes represents a complex, bidirectional connection where insulin resistance drives characteristic lipid abnormalities. Furthermore, diabetic dyslipidemia significantly amplifies cardiovascular risk, consequently requiring intensive management strategies that go beyond traditional cholesterol targets.
The intricate relationship between cholesterol disorders and type 2 diabetes creates one of medicine’s most challenging cardiovascular risk scenarios. Moreover, this bidirectional connection means that diabetes profoundly alters cholesterol metabolism, while dyslipidemia can accelerate the development of diabetic complications. Understanding diabetic dyslipidemia patterns becomes essential for clinicians managing the epidemic of diabetes-related cardiovascular disease.
Recent advances in diabetes management have revealed that traditional approaches to cholesterol control may be insufficient in diabetic populations. Additionally, the emergence of novel antidiabetic medications with significant lipid effects has transformed therapeutic strategies. Comprehensive cholesterol management approaches must now integrate diabetes-specific considerations to achieve optimal cardiovascular protection.
The Bidirectional Nature of Cholesterol and Diabetes
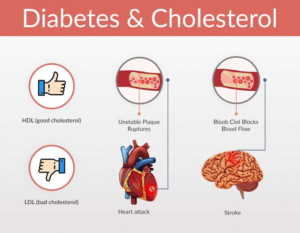
The relationship between cholesterol and type 2 diabetes extends far beyond simple coexistence, representing a complex interplay of metabolic pathways that mutually influence disease progression. Furthermore, American Heart Association research demonstrates that diabetes fundamentally alters lipid metabolism while dyslipidemia accelerates diabetic complications.
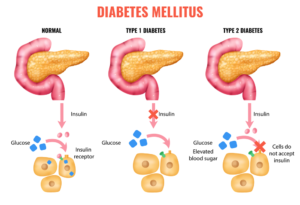
The bidirectional relationship manifests through multiple mechanisms. Specifically, insulin resistance—the hallmark of type 2 diabetes—directly disrupts normal cholesterol metabolism. Conversely, certain cholesterol-lowering medications can impair glucose homeostasis. Recent research published in Frontiers in Cardiovascular Medicine reveals the complex molecular crosstalk between glucose and cholesterol regulatory pathways.
How Diabetes Influences Cholesterol Metabolism
⏳ Diabetes-Driven Cholesterol Abnormalities
Insulin Resistance Effects
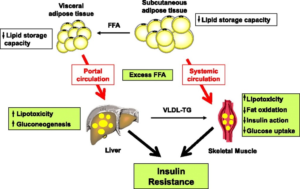
Initially, insulin resistance impairs the suppression of lipolysis in adipose tissue, consequently increasing free fatty acid flux to the liver. Subsequently, this enhanced substrate availability promotes hepatic triglyceride production while reducing HDL cholesterol synthesis.
Small Dense LDL Formation
Additionally, increased triglyceride-rich lipoproteins undergo extensive remodeling through cholesteryl ester transfer protein activity. Therefore, this process generates small, dense LDL particles that demonstrate enhanced atherogenicity compared to normal LDL cholesterol.
HDL Dysfunction Development
Furthermore, chronic hyperglycemia and inflammation impair HDL particle function beyond simple quantity reductions. Consequently, diabetic HDL particles demonstrate reduced reverse cholesterol transport capacity and diminished antioxidant properties.
The metabolic consequences extend beyond simple lipid level changes. Moreover, research published in Nature Reviews Endocrinology indicates that diabetic dyslipidemia represents a qualitative rather than merely quantitative lipid disorder, with profound implications for cardiovascular risk assessment.
Characteristic Patterns of Diabetic Dyslipidemia
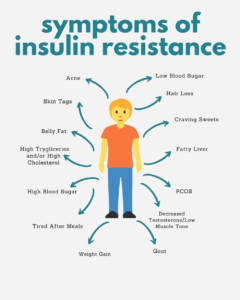
Diabetic dyslipidemia presents distinct patterns that differentiate it from dyslipidemia in non-diabetic populations. Furthermore, these characteristic abnormalities occur even when glucose control appears adequate, highlighting the importance of comprehensive lipid management in diabetes care.
American Diabetes Association research has established the characteristic features of diabetic dyslipidemia. Importantly, while total LDL cholesterol levels may appear normal, the qualitative changes in LDL particle composition significantly increase cardiovascular risk.
The Atherogenic Lipid Profile in Diabetes
| Lipid Parameter | Typical Pattern | Mechanism | Cardiovascular Impact |
|---|---|---|---|
| Triglycerides | Elevated (>150 mg/dL) | Increased hepatic VLDL production | Enhanced remnant particle formation |
| HDL Cholesterol | Reduced (<40 mg/dL men, <50 mg/dL women) | Accelerated HDL catabolism | Impaired reverse cholesterol transport |
| LDL Cholesterol | Normal levels, altered composition | Increased small dense particles | Enhanced oxidation susceptibility |
| Apolipoprotein B | Increased concentration | More atherogenic particles | Better cardiovascular risk predictor |
The progression from normal lipid profiles to diabetic dyslipidemia follows predictable patterns. Additionally, recent NHANES database analysis confirms the strong inverse relationship between HDL cholesterol levels and type 2 diabetes development, supporting the causal role of dyslipidemia in diabetic pathogenesis.
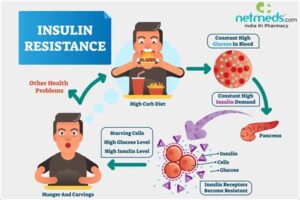
Insulin Resistance: The Central Mechanism
Insulin resistance serves as the primary driver connecting diabetes and dyslipidemia through multiple interconnected pathways. Moreover, understanding these mechanisms enables targeted therapeutic interventions that address both glucose and lipid abnormalities simultaneously.
❌ Common Misconception
Diabetic dyslipidemia primarily results from poor glucose control and improves with intensive diabetes management alone, without requiring specific lipid-targeted interventions.
✅ Scientific Reality
Diabetic dyslipidemia persists even with excellent glucose control due to underlying insulin resistance. Therefore, comprehensive management requires both glucose optimization and targeted lipid therapies for optimal cardiovascular protection.
Research published in Endocrine Reviews demonstrates that insulin resistance creates a cluster of cardiovascular risk factors, collectively termed insulin resistance syndrome, where each component independently contributes to atherosclerotic cardiovascular disease development.
Molecular Mechanisms Linking Insulin Resistance and Dyslipidemia
The molecular pathways connecting insulin resistance to dyslipidemia involve complex interactions between lipid metabolism, inflammatory signaling, and endothelial function. Furthermore, these mechanisms explain why traditional cardiovascular risk prediction models often underestimate risk in diabetic populations.
Insulin resistance fundamentally alters hepatic lipid metabolism, adipose tissue function, and vascular physiology, creating a perfect storm for accelerated atherosclerosis that extends far beyond simple cholesterol elevation.
The hepatic consequences of insulin resistance include enhanced de novo lipogenesis despite hyperglycemia, a phenomenon that contradicts normal metabolic regulation. Additionally, research in Cardiovascular Diabetology reveals that insulin resistance promotes endothelial dysfunction through impaired nitric oxide signaling while simultaneously enhancing inflammatory mediator production.
Key Molecular Pathways in Diabetic Dyslipidemia
Hepatic Lipid Metabolism Disruption
SREBP-1c Activation: Insulin resistance paradoxically maintains SREBP-1c activity despite hyperinsulinemia, promoting continued fatty acid synthesis.
VLDL Overproduction: Enhanced substrate availability and altered hepatic insulin signaling increase VLDL triglyceride secretion rates.
Adipose Tissue Dysfunction
Lipolysis Dysregulation: Impaired insulin suppression of hormone-sensitive lipase increases free fatty acid release from adipocytes.
Inflammatory Cytokine Release: Dysfunctional adipose tissue secretes inflammatory mediators that further impair insulin sensitivity systemically.
The vascular consequences extend beyond traditional lipid effects. Specifically, molecular studies demonstrate that insulin resistance directly impairs endothelial nitric oxide synthase function while promoting vascular smooth muscle proliferation, creating conditions conducive to accelerated atherosclerosis independent of cholesterol levels.
Cardiovascular Risk Amplification in Diabetic Dyslipidemia
The cardiovascular risk associated with diabetic dyslipidemia exceeds the sum of individual risk factors, representing a synergistic interaction that dramatically accelerates atherosclerotic disease progression. Furthermore, traditional risk assessment tools often underestimate the true cardiovascular burden in diabetic populations.
American Diabetes Association 2024 guidelines recognize diabetes as a coronary heart disease equivalent, recommending aggressive cardiovascular risk factor modification. Nevertheless, achieving optimal outcomes requires understanding the unique pathophysiology of diabetic cardiovascular disease.
Enhanced Atherosclerosis Mechanisms
⏳ Accelerated Atherosclerosis in Diabetes
Enhanced LDL Oxidation
Initially, hyperglycemia and advanced glycation end products increase LDL particle susceptibility to oxidative modification. Subsequently, these oxidized LDL particles demonstrate enhanced uptake by macrophages, accelerating foam cell formation and plaque development.
Endothelial Dysfunction Progression
Additionally, chronic hyperglycemia and insulin resistance impair endothelial nitric oxide production while enhancing inflammatory cytokine expression. Therefore, this creates a prothrombotic, pro-inflammatory vascular environment that promotes plaque instability.
Platelet Hyperactivity Development
Furthermore, diabetic patients demonstrate enhanced platelet aggregation and reduced response to antiplatelet therapy. Consequently, this prothrombotic state increases acute cardiovascular event risk even with stable plaque burden.
The temporal relationship between diabetes onset and cardiovascular events demonstrates the rapid acceleration of atherosclerotic processes. Moreover, recent cardiovascular outcome studies reveal that cardiovascular risk reduction strategies must begin immediately upon diabetes diagnosis rather than waiting for traditional risk factor thresholds.
Evidence-Based Management Strategies
Optimal management of diabetic dyslipidemia requires intensive, multifaceted approaches that address both glycemic control and lipid abnormalities simultaneously. Furthermore, recent clinical trials have established that aggressive lipid management provides substantial cardiovascular benefits independent of baseline cholesterol levels.
The foundation of diabetic dyslipidemia management involves high-intensity statin therapy as first-line treatment. Additionally, comprehensive reviews in Endotext demonstrate that statins provide cardiovascular benefits in diabetic populations that extend beyond LDL cholesterol reduction, including anti-inflammatory and plaque-stabilizing effects.
Statin Therapy: The Cornerstone of Treatment
| Statin Intensity | Expected LDL Reduction | Recommended Agents | Diabetic Considerations |
|---|---|---|---|
| High-Intensity | ≥50% reduction | Atorvastatin 40-80mg, Rosuvastatin 20-40mg | Preferred for most diabetic patients |
| Moderate-Intensity | 30-49% reduction | Simvastatin 20-40mg, Pravastatin 40mg | Alternative for statin intolerance |
| Low-Intensity | <30% reduction | Simvastatin 10mg | Rarely appropriate in diabetes |
The diabetogenic potential of statins represents a clinical consideration that should not prevent their use in appropriate patients. Specifically, recent meta-analyses indicate that while high-intensity statins may increase diabetes risk by approximately 12%, the cardiovascular benefits substantially outweigh this modest risk in most populations.
Combination Lipid Therapy Approaches
Many diabetic patients require combination lipid therapy to achieve optimal cardiovascular protection. Furthermore, recent clinical trials have validated specific combination approaches that provide additive benefits beyond statin monotherapy.
✅ Evidence-Based Combination Strategies
- Statin + Ezetimibe: Additional 15-20% LDL reduction with proven cardiovascular benefit
- Statin + PCSK9 inhibitor: Dramatic LDL reductions (>60%) for highest-risk patients
- Statin + Bempedoic acid: Alternative for statin-intolerant patients with cardiovascular benefits
- High-dose EPA: Triglyceride reduction with cardiovascular event reduction in REDUCE-IT trial
- Fibrate therapy: Consideration for severe hypertriglyceridemia (>500 mg/dL)
The timing of combination therapy initiation has evolved based on recent evidence. Moreover, current guidelines increasingly recommend early combination therapy for diabetic patients at highest cardiovascular risk rather than sequential monotherapy approaches that may delay optimal protection.
Novel Diabetes Medications and Lipid Effects
The emergence of SGLT2 inhibitors and GLP-1 receptor agonists has transformed diabetes management while providing unexpected benefits on lipid metabolism and cardiovascular outcomes. Furthermore, these medications demonstrate that effective diabetes management can simultaneously address multiple cardiovascular risk factors.
Recent systematic reviews of lipid effects reveal important differences between medication classes. Specifically, GLP-1 receptor agonists demonstrate more pronounced improvements in traditional diabetic dyslipidemia patterns, while SGLT2 inhibitors provide unique benefits on cardiovascular outcomes through mechanisms beyond lipid modification.
SGLT2 Inhibitors: Cardiovascular Benefits Beyond Glucose
Lipid Profile Effects
LDL Cholesterol: Mild increases (3-8%) primarily in large, buoyant particles with reduced atherogenicity
HDL Cholesterol: Modest improvements (2-5%) with potential functional benefits
Triglycerides: Variable effects depending on baseline levels and specific agent
Cardiovascular Mechanisms
Hemodynamic Effects: Reduced preload and afterload benefiting heart failure patients
Metabolic Benefits: Improved insulin sensitivity and reduced inflammatory markers
Renal Protection: Direct nephroprotective effects independent of glucose lowering
The cardiovascular outcome trials with SGLT2 inhibitors have consistently demonstrated benefits that extend far beyond their modest lipid effects. Additionally, comprehensive analyses suggest that the primary cardiovascular benefits result from hemodynamic improvements and direct cardioprotective mechanisms rather than lipid modification alone.
GLP-1 Receptor Agonists: Comprehensive Metabolic Benefits
GLP-1 receptor agonists provide more substantial improvements in diabetic dyslipidemia patterns while delivering proven cardiovascular benefits in high-risk populations. Moreover, these medications address multiple components of the metabolic syndrome simultaneously.
The cardiovascular benefits of GLP-1 receptor agonists appear to result from a combination of weight loss, improved insulin sensitivity, direct cardiovascular effects, and favorable modifications of the atherogenic lipid profile characteristic of diabetes.
Recent comparative studies demonstrate that GLP-1 receptor agonists significantly improve both the triglyceride/HDL cholesterol ratio and triglyceride-glucose index—two important markers of insulin resistance and cardiovascular risk in diabetic populations.
Lifestyle Interventions and Metabolic Optimization
While pharmacological interventions form the cornerstone of diabetic dyslipidemia management, lifestyle modifications provide synergistic benefits that enhance medication effectiveness while addressing underlying insulin resistance. Furthermore, comprehensive lifestyle approaches can prevent or delay the progression from prediabetes to overt diabetes.
⏳ Evidence-Based Lifestyle Modification Strategy
Structured Weight Management
Initially, even modest weight loss (5-10% of body weight) significantly improves insulin sensitivity and diabetic dyslipidemia patterns. Subsequently, maintained weight reduction provides sustained improvements in cardiovascular risk factors.
Regular Physical Activity
Additionally, both aerobic exercise and resistance training improve insulin sensitivity through distinct mechanisms. Therefore, combined exercise programs provide optimal benefits for glucose control and lipid metabolism.
Dietary Pattern Optimization
Furthermore, Mediterranean-style dietary patterns with emphasis on monounsaturated fats, omega-3 fatty acids, and fiber-rich foods improve both glucose control and lipid profiles simultaneously.
Evidence from diabetes organizations consistently demonstrates that comprehensive lifestyle interventions can achieve meaningful improvements in diabetic dyslipidemia that complement pharmacological treatments. Nevertheless, most patients require medication therapy to achieve optimal cardiovascular protection.
Functional Foods and Targeted Supplements
Emerging evidence supports specific functional foods and supplements that may provide additional benefits for diabetic dyslipidemia management. However, these interventions should complement rather than replace proven pharmacological therapies.
❌ Supplement Limitations
- Plant sterols provide modest cholesterol reductions (5-15%)
- Omega-3 supplements show inconsistent cardiovascular benefits
- Fiber supplements require high doses for meaningful lipid effects
- Antioxidant supplements lack proven cardiovascular benefits
✅ Evidence-Based Approaches
- High-dose prescription omega-3 (icosapent ethyl) reduces cardiovascular events
- Soluble fiber from whole foods improves glucose and lipid control
- Plant sterol-enriched foods provide additive cholesterol benefits
- Probiotics may improve insulin sensitivity and inflammation
The integration of evidence-based lifestyle interventions with appropriate pharmacological therapy provides optimal outcomes for diabetic dyslipidemia management. Moreover, individualized approaches that consider patient preferences, comorbidities, and treatment goals maximize long-term adherence and clinical success.
Future Directions and Emerging Therapies
The field of diabetic dyslipidemia management continues evolving rapidly, with novel therapeutic targets and personalized medicine approaches promising to further improve cardiovascular outcomes. Furthermore, emerging understanding of the gut microbiome, inflammatory pathways, and genetic factors opens new avenues for intervention.
The development of next-generation therapies focuses on addressing the root causes of diabetic dyslipidemia rather than simply treating lipid levels. Additionally, precision medicine approaches using genetic testing, biomarker profiling, and artificial intelligence promise to optimize treatment selection and dosing for individual patients.
Emerging Therapeutic Targets
Advanced Lipid Therapies
Inclisiran: Long-acting siRNA therapy targeting PCSK9 with twice-yearly dosing
Bempedoic Acid: Novel cholesterol synthesis inhibitor with proven cardiovascular benefits
Evinacumab: ANGPTL3 inhibitor for severe dyslipidemia management
Metabolic Modulators
Dual GLP-1/GIP Agonists: Enhanced weight loss and metabolic benefits
FGF21 Analogues: Metabolic hormone replacement therapy
Mitochondrial Modulators: Targeting cellular energy metabolism dysfunction
The future of diabetic dyslipidemia management likely involves increasingly personalized approaches based on individual risk profiles, genetic predisposition, and biomarker patterns. Nevertheless, current evidence-based therapies provide substantial cardiovascular protection when implemented appropriately and maintained consistently.
References
- American Heart Association. (2025). Cholesterol and Diabetes. AHA Patient Education.
- American Diabetes Association. (2024). Cardiovascular Disease and Risk Management: Standards of Care in Diabetes—2024. Diabetes Care, 47(Supplement_1), S179-S218.
- Mooradian, A. D. (2009). Dyslipidemia in type 2 diabetes mellitus. Nature Reviews Endocrinology, 5(3), 150-159.
- American Diabetes Association. (2004). Dyslipidemia Management in Adults With Diabetes. Diabetes Care, 27(suppl_1), s68-s71.
- Reaven, G. M. (2019). Insulin Resistance and Atherosclerosis: Implications for Insulin-Sensitizing Agents. Endocrine Reviews, 40(6), 1447-1467.
- Patti, D., et al. (2022). Updated Understanding of the Crosstalk Between Glucose/Insulin and Cholesterol Metabolism. Frontiers in Cardiovascular Medicine, 9, 879355.
- Abdul-Ghani, M. A., et al. (2018). Association between insulin resistance and the development of cardiovascular disease. Cardiovascular Diabetology, 17, 122.
- Yan, Z., et al. (2024). Association between high-density lipoprotein cholesterol and type 2 diabetes mellitus: dual evidence from NHANES database and Mendelian randomization analysis. Frontiers in Endocrinology, 15, 1272314.
- Feingold, K. R. (2023). Dyslipidemia in Patients with Diabetes. Endotext.
- Cardoso, C. R. L., et al. (2024). Lipid Disorders Management Strategies (2024) in Prediabetic and Diabetic Patients. Journal of Clinical Medicine, 13(4), 1007.
- Pantalone, K. M., et al. (2022). Lipid Profile Changes Associated with SGLT-2 Inhibitors and GLP-1 Agonists in Diabetes and Metabolic Syndrome. Current Diabetes Reports, 22(5), 213-225.
- Sattar, N., et al. (2021). SGLT2 inhibitors and GLP-1 receptor agonists: established and emerging indications. The Lancet, 398(10296), 262-276.
- Diabetes UK. (2024). Cholesterol and diabetes. Diabetes UK Patient Education.
- Korakas, E., et al. (2025). The effects of SGLT2 inhibitors and GLP-1 receptor agonists on the triglyceride to HDL cholesterol ratio and the triglyceride-glucose index. Journal of Diabetes and its Complications, 39(6), 109035.
- Das, S. R., et al. (2022). GLP-1 Receptor Agonists for the Reduction of Atherosclerotic Cardiovascular Risk in Patients With Type 2 Diabetes. Circulation, 146(9), 662-677.
Role Image / Video Source Featured Image AHA/ADA infographic Mechanism Diagram NetMeds or Free Fatty Acids Lipid Profile Diabetes Council graphic Symptoms Visual Diabetes Stages DetsUtah “Stages” image Video Clip Pixabay “Blood Sugar”
Related Articles
Author Bio
The Remedy Verified Team translates complex metabolic science into clear, practical strategies for everyday health.
Disclaimer
This article is for educational purposes only and should not replace professional medical advice. Always consult with qualified healthcare providers before making changes to diabetes or cholesterol management plans. Individual responses to treatments vary significantly, and optimal therapeutic approaches depend on multiple factors including comorbidities, medication interactions, and patient-specific risk profiles. Regular monitoring and professional guidance are essential for safe and effective management of diabetic dyslipidemia.