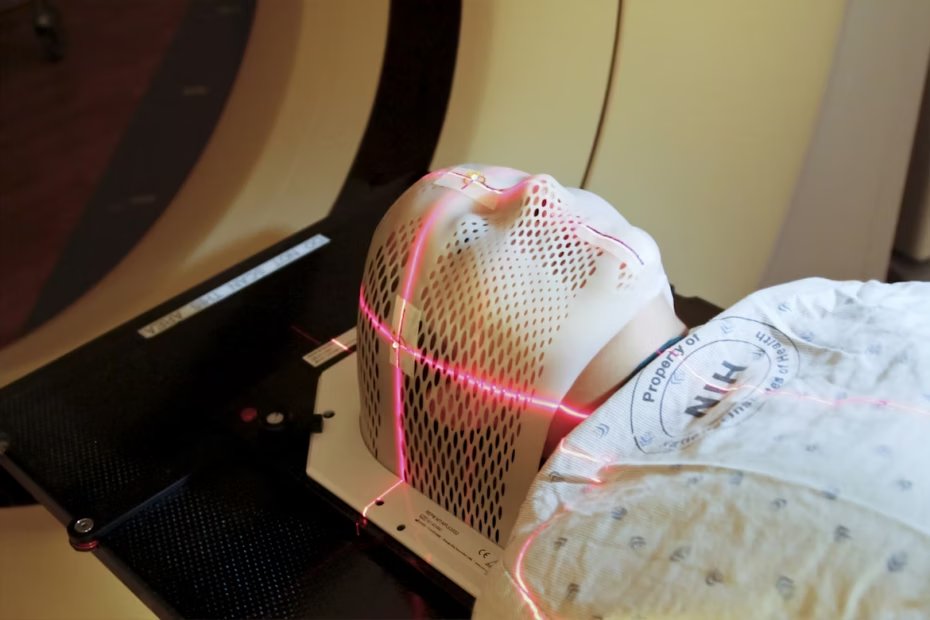
You’ve got an MRI scheduled, and now you’re wondering: can you eat before an MRI, or do you need to fast? The answer depends entirely on which type of scan you’re having—and honestly, the preparation instructions you’ll find online often contradict each other, leaving you more confused than when you started.
Here’s what matters: Most MRIs for the brain, spine, or joints let you eat and drink normally beforehand. But five specific scenarios—abdominal imaging, scans using contrast dye, certain gastrointestinal procedures, MRCP, and MRIs requiring sedation—do require fasting for 4 to 8 hours. The challenge? Protocols vary by imaging facility, and what applies to one scan type doesn’t necessarily apply to another.
This guide walks you through the evidence behind each fasting requirement, explains exactly when and why dietary restrictions matter for image quality and safety, and gives you a clear framework for verifying your specific preparation needs. You’ll also learn what to do if you’ve accidentally eaten before a scan that required fasting—a common scenario that rarely results in cancellation. By the end, you’ll know precisely how to prepare for your MRI based on your scan type, not guesswork.
Can You Eat Before an MRI? The Short Answer
For most MRIs—including brain, spine, and joint scans—you can eat and drink normally beforehand. However, you’ll need to fast for 4 to 8 hours before abdominal or pelvic MRIs, scans using contrast dye, gastrointestinal imaging, MRCP procedures, and MRIs requiring sedation. Always follow your imaging facility’s specific preparation instructions, since protocols can vary.
Quick Reference: MRI Fasting Requirements by Scan Type
| MRI Type | Fasting Required? | Duration | Can Drink Water? |
|---|---|---|---|
| Brain MRI | No | None | Yes |
| Spine MRI | No | None | Yes |
| Joint/Extremity MRI | No | None | Yes |
| Abdominal MRI | Yes | 4-6 hours | Small sips until 2 hours before |
| Pelvic MRI | Yes | 4-6 hours | Small sips until 2 hours before |
| MRI with contrast | Varies by facility | 2-4 hours (if required) | Verify with facility |
| MRCP | Yes | 4-6 hours | Small sips until 2 hours before |
| GI investigation | Yes | 6-8 hours | Limited; verify protocol |
| MRI with sedation | Yes (mandatory) | 6-8 hours (solids), 2 hours (clear liquids) | Only until 2 hours before |
Here’s what most preparation sheets won’t tell you: If you’ve already eaten and your scan requires fasting, call your imaging facility immediately rather than assuming your appointment will be cancelled. Many facilities can delay your scan time by a few hours or proceed with modified protocols, depending on what you ate and when. Cancellations are less common than you’d think.
Why Fasting Matters for Certain MRI Scans

MRI fasting requirements aren’t about the magnetic field or the machine itself—they’re about what’s happening inside your body during the scan and how that affects the images or your safety.
When you eat or drink, your digestive system activates peristalsis: rhythmic muscle contractions that move food through your stomach and intestines. These movements are involuntary and continuous. For MRIs focused on your abdomen or pelvis, peristalsis creates what radiologists call “motion artifacts”—blurring or distortion that can obscure tumors, lesions, or other abnormalities your doctor’s trying to detect. Studies on abdominal MRI quality have quantified this impact: digestive motion can reduce diagnostic accuracy by creating false signals or masking real pathology. Fasting for 4 to 6 hours significantly reduces peristaltic activity, giving radiologists clearer images of organs like your liver, pancreas, and gallbladder.
The second reason for fasting relates to contrast agents—specifically gadolinium-based dyes injected through an IV to enhance visibility of blood vessels, tumors, or inflamed tissue. These contrast agents can cause nausea or vomiting in some patients, with reported incidence rates varying from 1% to 5% depending on the formulation and patient factors. When you’re lying flat inside an MRI scanner—often for 30 to 60 minutes—vomiting poses a genuine safety risk due to potential airway obstruction.
Fasting for 2 to 4 hours before contrast administration reduces both the likelihood of nausea and the severity if it does occur. That said, protocols vary: not all imaging facilities require fasting for contrast, particularly for patients with no history of nausea or gastrointestinal sensitivity.
The third category is safety-critical: sedation and anesthesia. If you need medication to manage claustrophobia or anxiety—or if you’re a child who needs general anesthesia to remain still—fasting becomes non-negotiable. The risk is aspiration: inhaling stomach contents into your lungs if you vomit while sedated. Anesthesia safety guidelines from the American Society of Anesthesiologists specify fasting windows of 6 to 8 hours for solid foods and 2 hours for clear liquids. These aren’t suggestions; they’re evidence-based protocols designed to prevent a potentially life-threatening complication.
Fasting requirements exist for measurable reasons—image clarity or patient safety—not as blanket rules. Your specific MRI type determines whether dietary restrictions apply to you.
5 Situations That Require Fasting Before Your MRI
These five scenarios account for the majority of MRIs that require dietary restrictions. Each has specific fasting windows and evidence-based rationales.
1. Abdominal or Pelvic MRI Scans
Typical fasting window: 4 to 6 hours before your scan
Organs commonly imaged: Liver, pancreas, gallbladder, kidneys, intestines, bladder, reproductive organs
If your MRI focuses on any abdominal or pelvic organ, expect to fast. The reason is purely mechanical: peristalsis—the wave-like muscle contractions that move food through your digestive tract—creates motion during image acquisition. This motion shows up as blurring, streaking, or ghosting artifacts in the final images. For a radiologist trying to identify a small liver lesion or assess pancreatic inflammation, these artifacts can obscure critical diagnostic details or create false positives.
Fasting doesn’t stop peristalsis entirely, but it significantly reduces its intensity and frequency. Research on MRI artifact reduction shows that a 4-hour fast decreases bowel motion artifacts enough to improve diagnostic confidence. Most facilities will allow small sips of water up to 2 hours before your scan to prevent dehydration—confirm this when you schedule.
Here’s a detail competitors miss: fatty or greasy foods can extend digestion time beyond the standard fasting window. If you eat a heavy meal 6 hours before an abdominal MRI, residual gastric contents may still interfere with imaging. Light, easily digestible meals in the 12 to 24 hours before your scan give better results.
2. MRI with Contrast (Gadolinium-Based Agents)

Typical fasting window: 2 to 4 hours (facility protocols vary)
Why contrast is used: To enhance visibility of blood vessels, tumors, inflammation, or abnormal tissue
Approximately 25% of MRI scans use intravenous contrast agents—most commonly gadolinium-based compounds. These agents improve image contrast by altering the magnetic properties of tissues, making abnormalities easier to detect. The injection itself takes seconds and occurs while you’re positioned in the scanner.
The fasting requirement for contrast is more variable than for abdominal scans. Some facilities require it universally; others only recommend it for patients with a history of nausea, motion sickness, or gastrointestinal sensitivity. The evidence base is mixed: gadolinium nausea rates are low (1% to 5%), but the consequences of vomiting while lying flat in an enclosed space are significant enough that many radiologists prefer the precaution.
Here’s what to verify with your imaging center: whether their protocol requires fasting for all contrast MRIs or only for specific patient populations. If you have no history of nausea and you’ve had contrast scans before without issues, some facilities will clear you to eat normally. Others enforce blanket fasting policies. Know your facility’s stance before your appointment.
3. MRCP (Magnetic Resonance Cholangiopancreatography)

Typical fasting window: 4 to 6 hours
What it images: Bile ducts, pancreatic ducts, and gallbladder
MRCP is a specialized MRI technique used to visualize the biliary and pancreatic duct systems—often ordered when doctors suspect gallstones, duct obstruction, or pancreatic abnormalities. This scan has unique preparation requirements beyond standard abdominal imaging.
Fasting serves three purposes for MRCP: First, it reduces peristalsis artifacts in the adjacent stomach and duodenum. Second, it minimizes fluid secretions in the upper digestive tract that can obscure duct visualization. Third—and most important—fasting promotes gallbladder distension. When you haven’t eaten for several hours, your gallbladder fills with bile and expands, making it easier to see both the gallbladder itself and any stones or sludge within it. A contracted, post-meal gallbladder is significantly harder to image accurately.
Some MRCP protocols also involve drinking a contrast solution (like diluted pineapple juice or commercial oral contrast) to further suppress bowel signal. Your facility will specify this when scheduling.
4. Gastrointestinal Condition Investigation
Typical fasting window: 6 to 8 hours; may include 24-hour dietary modifications
Common indications: Suspected GI bleeding, bowel obstruction, Crohn’s disease, intestinal inflammation
When your MRI is specifically investigating digestive symptoms or suspected gastrointestinal pathology, preparation often extends beyond simple fasting. You may be asked to follow a low-residue diet for 24 hours before the scan—avoiding high-fiber foods, raw vegetables, nuts, seeds, and whole grains—to minimize bowel contents and gas production.
An empty GI tract lets radiologists assess bowel wall thickness, detect inflammation patterns, identify strictures or obstructions, and locate sources of bleeding without interference from stool, gas, or undigested food. Some protocols include bowel preparation similar to colonoscopy prep, though less intensive. Others involve drinking large volumes of oral contrast solution to distend the intestines for better visualization (called MR enterography).
Verify the complete preparation protocol with your ordering physician or imaging facility, since requirements vary significantly based on what’s being investigated. A Crohn’s disease assessment may need different prep than a suspected obstruction workup.
5. MRI with Sedation or Anesthesia
Typical fasting window: 6 to 8 hours for solid foods; 2 hours for clear liquids
Who needs sedation: Patients with severe claustrophobia, anxiety disorders, movement disorders, or young children
If your MRI requires conscious sedation or general anesthesia—whether for claustrophobia management or because you’re unable to remain still for 30 to 90 minutes—fasting becomes a safety mandate, not a recommendation. The risk is aspiration pneumonia: if you vomit while sedated or under anesthesia, stomach contents can enter your lungs, causing serious respiratory complications.
Anesthesia fasting guidelines are standardized and evidence-based. The American Society of Anesthesiologists recommends no solid foods for 6 to 8 hours before sedation and no clear liquids for 2 hours before. These windows are based on gastric emptying times and aspiration risk studies. Violating them can result in your procedure being cancelled outright, since the safety risk outweighs the imaging benefit. The FDA provides comprehensive safety information on MRI procedures including sedation considerations.
If you’re scheduled for sedation, you’ll also need to arrange transportation home—you won’t be cleared to drive for 24 hours after receiving sedative medications. Coordinate medication timing with both your imaging facility and your primary care provider, particularly if you take diabetes medications or other time-sensitive prescriptions.
“MRI preparation requirements exist to optimize diagnostic accuracy and patient safety. When patients understand the rationale behind fasting protocols, compliance improves significantly.”
— American College of Radiology Committee on MR Safety
What If You Have Diabetes, Accidentally Ate, or Other Concerns?
Real-world MRI preparation rarely follows the textbook script. Here’s how to handle the most common complications and special circumstances that standard preparation sheets don’t adequately address.
If You Accidentally Ate Before a Fasting MRI
This is far more common than you’d think—and it rarely results in automatic cancellation. Call your imaging facility immediately when you realize the mistake. Provide specific details: what you ate, how much, and exactly when. A small snack 5 hours before an abdominal MRI has different implications than a full meal 2 hours before contrast administration.
Most facilities have protocols for this scenario. Options include: delaying your scan time by 2 to 4 hours to allow additional fasting, proceeding with the scan if you only consumed clear liquids or a very light snack, or rescheduling if you ate a substantial meal too close to a sedation-required scan.
The exception? Sedation. If you’ve eaten within the required fasting window and your scan requires anesthesia or conscious sedation, facilities cannot proceed due to aspiration risk. That’s a safety line they won’t cross. But for image-quality fasting (abdominal scans, contrast), there’s usually flexibility.
Managing Diabetes and Fasting Requirements
The intersection of MRI fasting and diabetes medication creates a timing challenge that requires coordination between your imaging facility and your diabetes care team. Here’s the framework to discuss with both providers.
If you take insulin or sulfonylureas (glyburide, glipizide, glimepiride), fasting without adjusting your medication dose can trigger hypoglycemia. The standard approach: reduce or skip your short-acting insulin dose before the fasting period, or take your oral diabetes medication after the scan with food. For morning scans with 4 to 6 hour fasting requirements, many patients schedule early appointments (7 to 8 AM), fast from midnight, skip or reduce their morning diabetes medications, and eat immediately after the scan.
If you use a continuous glucose monitor (CGM) or insulin pump, verify MRI compatibility before your appointment. Most modern CGMs must be removed before entering the MRI room due to the magnetic field, though some newer models are MRI-conditional under specific parameters. Insulin pumps are never MRI-safe and must be disconnected and removed—work with your endocrinologist to plan temporary basal rate adjustments or alternative insulin delivery during your scan.
The critical principle: never fast without a medication plan. Communicate your diabetes management regimen when scheduling your MRI, verify the fasting requirement and duration, and get explicit guidance from your diabetes care team on medication timing. Document the plan and bring glucose tablets or a rapid-acting carbohydrate source to consume immediately after scanning if needed.
Pediatric Fasting Modifications
Fasting windows for children are significantly shorter than adult protocols, scaled by age to account for smaller gastric volumes and faster metabolism. Standard pediatric anesthesia guidelines recommend: no solid foods for 6 hours, no breast milk for 4 hours, and no clear liquids for 2 hours before sedation or anesthesia.
For non-sedated pediatric MRIs (older children or adolescents having brain, spine, or extremity scans), fasting is typically not required unless the scan falls into one of the five categories above. When it is required—such as for abdominal imaging—the fasting window is usually 4 hours rather than 6 to 8, with clear liquids permitted up to 2 hours before.
Coordinate closely with your pediatrician or the imaging facility’s child life specialist when preparing a young child for an MRI. The combination of fasting and scan anxiety can be challenging; some facilities offer morning appointment priority for fasting-required pediatric scans to minimize the distress of prolonged food restriction.
Pregnancy Considerations
MRI is generally considered safe during pregnancy—unlike CT scans, there’s no ionizing radiation. However, gadolinium-based contrast agents are typically avoided during pregnancy unless the diagnostic benefit clearly outweighs potential fetal risk, based on American College of Radiology guidance. Most pregnancy-related MRIs (placental assessment, fetal imaging, maternal organ evaluation) don’t use contrast.
Fasting requirements during pregnancy follow the same logic as for non-pregnant patients: if you’re having an abdominal, pelvic, or contrast-enhanced scan, expect to fast for 4 to 6 hours. If you’re having a brain or spine MRI, eating is usually permitted. The added consideration is nausea management—pregnancy-related nausea can make lying flat in an MRI scanner uncomfortable. Some facilities recommend scheduling scans during your typical low-nausea window and bringing anti-nausea medication approved by your obstetrician.
Medication Management During Fasting
Most medications can and should be taken as prescribed, even during MRI fasting periods. Take your regular medications with small sips of water unless your imaging facility or prescribing physician specifically instructs otherwise. This applies to blood pressure medications, thyroid medications, antidepressants, and most other maintenance drugs.
The exceptions: diabetes medications (addressed above), and certain bowel medications or supplements that might affect abdominal imaging. If you take medications that slow or speed gastric motility, ask your ordering physician whether timing adjustments are needed. For most patients, the instruction is straightforward: continue your regular medication schedule with minimal water, regardless of fasting status.
Beyond Fasting: Complete MRI Preparation Protocol
Dietary preparation is only one component of MRI readiness. These additional requirements apply to virtually all MRI scans, regardless of fasting status. For comprehensive safety information, the American College of Radiology provides detailed MR safety resources for patients and healthcare professionals.
Essential MRI Preparation Checklist:
- Remove all metal objects: jewelry, watches, piercings, hearing aids, dentures, hairpins
- Wear metal-free clothing: no zippers, buttons, snaps, or underwire bras
- Skip cosmetics: no makeup, deodorant, hair products, or lotions on scan day
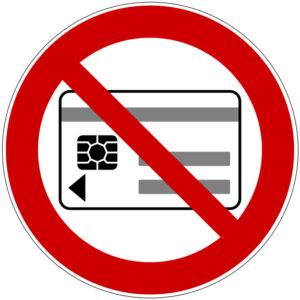
- Secure valuables: leave credit cards and magnetic-stripe cards in your car (MRI will erase them)
- Arrive 30-45 minutes early for paperwork and safety screening
Metal Object Removal: More Than Just Jewelry
The MRI’s magnetic field is extraordinarily powerful—typically 1.5 to 3 Tesla, which translates to 30,000 to 60,000 times stronger than Earth’s magnetic field. Any ferromagnetic object can become a dangerous projectile or cause serious burns from induced electrical currents. The National Institute of Biomedical Imaging and Bioengineering explains how MRI technology works and why these safety precautions are essential.
Remove before entering the MRI room: all jewelry (including body piercings), watches, eyeglasses, hearing aids, removable dental work, hairpins or clips, underwire bras, clothing with metal zippers or buttons, belts with metal buckles, and shoes (most contain metal in the soles or eyelets). Most facilities provide metal-free lockers and hospital gowns for changing.
Less obvious hazards: credit cards, hotel key cards, and other magnetic stripe cards will be permanently erased by the MRI field—leave them in your car or locker, not your pocket “just in case.” Some tattoos and permanent makeup contain metallic pigments (iron oxide, titanium dioxide) that can heat during scanning; inform the technologist about any tattoos, particularly around your eyes. Nicotine patches, pain relief patches, and medicated skin patches may contain metal backing and must be removed.
Cosmetics and Personal Care Products
This requirement surprises many patients: avoid wearing makeup, deodorant, antiperspirant, hair gel, mousse, hairspray, lotions, and sunscreen to your MRI appointment. The reason? Trace metal content—many cosmetics contain iron oxide, zinc oxide, or titanium dioxide for color, opacity, or UV protection.
When exposed to the MRI’s radiofrequency pulses, these metal particles can heat significantly, causing skin burns or irritation. Case reports in radiology literature document first- and second-degree burns from eye makeup, mascara, and metallic-based foundation during head and neck MRIs. The risk is highest for scans of the head, face, and neck, but many facilities enforce a no-cosmetics policy universally to eliminate the variable.
Deodorants and antiperspirants often contain aluminum compounds. These won’t cause burns but can create image artifacts that obscure anatomy near the axilla (armpit), which matters for breast MRI, chest MRI, or shoulder imaging. Come to your appointment clean but product-free, or bring unscented, non-metallic wipes to remove products before scanning.
Clothing Strategy
Wear or bring loose, comfortable clothing without metal components. Ideal: athletic wear, sweatpants, cotton T-shirts, sports bras (no underwire), and slip-on shoes. Avoid: jeans with metal rivets or zippers, shirts with snaps or buttons, bras with underwire or metal clasps, and any clothing with metallic threads or embellishments.
Many facilities provide hospital gowns for all patients; others allow you to wear your own metal-free clothing if it’s appropriate for the body region being scanned. Ask when you schedule your appointment so you can plan accordingly. If you’re having an extremity MRI (knee, ankle, wrist), you may be able to wear street clothes and only remove jewelry and shoes.
Hydration Timing
Unless you’re fasting for one of the five scenarios above, stay well-hydrated in the 24 hours before your MRI. Good hydration improves vein visibility and makes IV placement easier if you need contrast. However, avoid drinking excessive fluids in the 2 hours immediately before your scan—you’ll be lying still in the scanner for 30 to 90 minutes with no bathroom access.
If you are fasting, small sips of water are usually permitted up to 2 hours before the scan to prevent dehydration. Verify this with your facility. For morning appointments, many patients find it easier to schedule the scan as early as possible, fast from midnight, and drink normally after the procedure rather than managing prolonged restriction.
Arrival Time and Check-In

Plan to arrive 30 to 45 minutes before your scheduled scan time. This buffer allows for paperwork, changing into a gown if required, reviewing the safety screening questionnaire, and starting an IV line if contrast is ordered. MRI scheduling is typically tight—late arrival may result in scan cancellation and rescheduling.
Bring your insurance card, photo ID, and any previous imaging CDs or reports if this MRI is for comparison to prior studies. If you’re using sedation, confirm you have a designated driver, since facilities won’t release you to drive yourself home or use public transportation alone.
Your Step-by-Step Pre-MRI Verification Protocol
Most MRI preparation confusion stems from a mismatch between generic instructions and your specific scan requirements. Standard preparation sheets are written broadly to cover all scenarios, which means they often include restrictions that don’t apply to you—or worse, fail to mention restrictions that do. Here’s a systematic framework for getting clarity before your appointment.
Phase 1: When You Schedule (Week Before Your MRI)
This is your primary opportunity to gather accurate, personalized preparation instructions. Ask these specific questions—not “what do I need to do?” but targeted queries that elicit useful answers:
Why this matters: “Abdominal MRI” could mean liver-focused imaging (requires fasting) or kidney/adrenal imaging (may not require fasting). Document the specific anatomical focus, not just “abdomen” or “pelvis.”
Why this matters: Contrast protocols vary by facility. Get your facility’s specific policy, not general guidance. If fasting is required, ask the minimum duration—2 hours versus 4 hours makes a significant difference.
Why this matters: “Fasting” can mean different things. Clarify whether small sips of water for medications are permitted and up to what time.
Why this matters: Most medications continue as prescribed, but certain drugs interact with contrast agents or affect imaging quality.
Document the scheduler’s answers in writing. Read them back for confirmation before ending the call. This creates a paper trail if confusion arises later and gives you confidence you’ve captured the requirements accurately.
Phase 2: The 48-Hour Confirmation (Two Days Before Your MRI)
Preparation instructions occasionally change based on insurance authorization details, physician clarifications, or scheduling modifications. Call your imaging facility 48 hours before your appointment to reconfirm fasting requirements, arrival time, and whether your ordering physician sent any special preparation instructions.
Use this call to disclose information that might affect your scan or preparation:
- Metal implants or devices: Pacemakers, defibrillators, cochlear implants, insulin pumps, neurostimulators, implanted ports, surgical clips or mesh, joint replacements, or any foreign body. Most modern implants are MRI-conditional (safe under specific parameters), but the facility needs to verify compatibility before your appointment.
- Claustrophobia or anxiety history: If you anticipate difficulty tolerating the enclosed space, ask about sedation options now rather than discovering on scan day that sedation requires additional fasting and scheduling changes.
- Pregnancy or possibility of pregnancy: MRI is generally safe during pregnancy, but contrast agents are typically avoided. Early disclosure lets the facility coordinate with your obstetrician and adjust protocols if needed.
- Kidney disease history: Gadolinium contrast requires functioning kidneys for elimination. Patients with impaired renal function may need pre-scan blood work (creatinine and GFR) to assess safety. Ask whether labs are required and, if so, the timeframe for completing them before your scan.
- Previous adverse reactions: If you’ve had allergic reactions to contrast agents, IV medications, or anesthesia in the past, the facility may need to pre-medicate you or modify the protocol. Provide specific details: what substance caused the reaction, what symptoms you experienced, and how it was managed.
This confirmation call takes 5 minutes but prevents day-of surprises that could delay or cancel your scan.
Phase 3: Day-of Decision Points
If something goes wrong on the morning of your MRI—you accidentally ate, you forgot to stop a medication, you’re feeling ill—call the facility immediately upon recognizing the problem. Provide specific facts: “I ate two pieces of toast at 6 AM, and my scan’s scheduled for 11 AM” gives them the information needed to decide whether to proceed, delay, or reschedule.
The earlier you call, the more options they have. A call at 6 AM about eating before an 11 AM scan may result in pushing your appointment to 2 PM. A call at 10:45 AM leaves no flexibility. Most facilities would rather adjust your schedule than have you arrive, complete check-in paperwork, and then discover a disqualifying issue that forces last-minute cancellation.
If you arrive at the facility and feel uncomfortable with any aspect of the preparation or procedure—the informed consent document includes risks you weren’t aware of, the technologist’s instructions contradict what you were told when scheduling, or you’re uncertain whether you disclosed all relevant medical history—ask to speak with the supervising radiologist or lead technologist before proceeding. It’s always appropriate to seek clarification or request time to contact your referring physician for guidance before signing consent and entering the MRI room.
Common MRI Fasting Myths Debunked: Evidence vs. Assumptions
Standard preparation instructions often perpetuate misconceptions. Here’s what the evidence actually shows versus what many patients assume or are told.
| Myth | Evidence |
|---|---|
| “All MRIs require fasting” | False. Only ~30% of MRI scans require dietary restrictions, primarily abdominal/pelvic imaging, contrast-enhanced studies at some facilities, and sedation cases. Brain, spine, joint, and extremity MRIs typically allow normal eating. |
| “Drinking water breaks the fast for MRI” | Depends on scan type and facility protocol. Most fasting MRIs permit small sips of water for medications up to 2 hours before the scan. Clear liquids in moderation are often acceptable for image-quality fasting (abdominal scans) but restricted for sedation safety. Always verify your facility’s specific guideline. |
| “If I accidentally eat, my scan will automatically be cancelled” | Rarely true for image-quality fasting. Most facilities can delay scan time by 2-4 hours if you’ve eaten a light meal or snack. Full cancellation is typically reserved for violation of sedation fasting protocols or consuming a large meal immediately before an abdominal scan. Call immediately when you realize the error. |
| “Fasting improves all MRI image quality” | False. Fasting only matters when digestive activity affects the region being imaged (abdomen, pelvis) or when safety concerns exist (contrast nausea, sedation aspiration risk). Fasting before a knee MRI or brain MRI provides no benefit and may cause unnecessary discomfort, lightheadedness, or hypoglycemia. |
| “Contrast always requires fasting before MRI” | Variable by facility. Some imaging centers require 2-4 hour fasting before all contrast administration; others only recommend it for patients with nausea history or gastrointestinal sensitivity. The evidence shows gadolinium nausea rates of 1-5%, which some facilities consider low enough to make fasting optional. Know your facility’s protocol. |
| “I can’t take any medications when fasting for MRI” | False. Most maintenance medications should be taken as prescribed with small sips of water, even during fasting periods. Exceptions include diabetes medications that require food to prevent hypoglycemia and certain bowel-related medications that might affect abdominal imaging. Verify with both your prescribing physician and imaging facility. |
| “The 4-hour fasting rule is universal” | False. Fasting windows vary by scan type: 4-6 hours for abdominal/pelvic MRIs, 2-4 hours for some contrast protocols, 6-8 hours for sedation (solid foods), and 2 hours for clear liquids before sedation. Pediatric fasting windows are shorter. The “4-hour rule” is an approximation, not a standard. |
You’ll notice a pattern: MRI preparation requirements are more variable and contextual than most generic instruction sheets suggest. What works: verify your specific requirements for your specific scan type at your specific facility rather than relying on general guidelines or assumptions based on someone else’s MRI experience.
What to Eat Before an MRI (When Fasting Is Required)
If your MRI requires fasting, what you eat in the 12-24 hours before your fasting period begins can affect both your comfort and image quality. Strategic meal planning makes fasting easier and improves scan outcomes.
The Day Before Your Fasting MRI
Choose easily digestible foods that won’t extend gastric emptying time or create excessive gas. Light proteins (chicken, fish, eggs), simple carbohydrates (white rice, plain pasta, toast), and cooked vegetables without skins digest more predictably than heavy, fatty, or high-fiber meals.
Avoid these in the 24 hours before fasting begins if you’re having abdominal or pelvic imaging: fatty or greasy foods (fried items, heavy sauces, full-fat dairy), cruciferous vegetables (broccoli, cauliflower, cabbage, Brussels sprouts—they produce gas), beans and legumes (gas production), carbonated beverages, and high-fiber whole grains in large quantities. These foods either slow digestion or create intestinal gas that can interfere with image clarity.
For morning MRIs with overnight fasting: eat a moderate dinner by 7 PM, then nothing after midnight except approved medications with small sips of water. For afternoon MRIs with 4-6 hour fasting: eat a light breakfast (toast with peanut butter, banana, yogurt) by 7-8 AM if your scan’s at 2 PM.
During the Fasting Window
Take your regular medications as prescribed with minimal water unless specifically instructed otherwise. Small sips—defined as 1-2 ounces total—are typically permitted up to 2 hours before non-sedation scans for medication administration and preventing dehydration-related lightheadedness.
If you’re diabetic and adjusting insulin or oral medications during fasting, follow your endocrinologist’s protocol precisely. Bring a rapid-acting carbohydrate source (glucose tablets, juice box, crackers) to consume immediately after your scan to prevent post-fasting hypoglycemia, particularly if you’ve reduced your medication doses.
After Your MRI
Unless you received sedation, you can eat immediately after your scan’s complete. Start with easily digestible foods rather than a large, heavy meal—particularly if you’ve been fasting for 6+ hours. Your digestive system restarts gradually; gentle refeeding prevents discomfort.
If you received contrast, increase fluid intake for 24 hours after your scan to help your kidneys eliminate the gadolinium. Water, herbal tea, diluted juice, and clear broths all support hydration and contrast clearance.
Frequently Asked Questions About Eating Before an MRI
How long do you have to fast before an MRI?
Fasting duration depends on your scan type: 4 to 6 hours for abdominal or pelvic MRIs, 2 to 4 hours for MRIs with contrast at facilities that require it, 4 to 6 hours for MRCP, 6 to 8 hours for gastrointestinal investigations, and 6 to 8 hours for solid foods (2 hours for clear liquids) if sedation’s required. Most brain, spine, and joint MRIs don’t require any fasting. Verify your specific timeframe with your imaging facility when scheduling.
Can you drink water before an MRI?
Yes, in most cases. For non-fasting MRIs (brain, spine, joints), drink water normally. For fasting MRIs, small sips of water for medications are usually permitted up to 2 hours before your scan. The exception is sedation protocols, which typically restrict all intake—including water—for 2 hours before the procedure. Always confirm your facility’s specific water policy when you schedule your appointment.
What happens if you eat before an abdominal MRI?
If you eat before an abdominal MRI that requires fasting, the digestive process creates peristalsis—muscle contractions that move food through your intestines. These movements create motion artifacts (blurring, streaking, or distortion) in the MRI images, potentially obscuring tumors, lesions, or other abnormalities your doctor’s trying to detect. However, eating doesn’t automatically cancel your scan. Call your imaging facility immediately when you realize the error; many can delay your appointment by 2 to 4 hours to allow additional fasting time, particularly if you only ate a small amount.
Can you take medications before an MRI?
Yes, most medications should be taken as prescribed with small sips of water, even during MRI fasting periods. This includes blood pressure medications, thyroid medications, antidepressants, and other maintenance drugs. The exceptions are diabetes medications (insulin, sulfonylureas, metformin) that may require dose adjustments during fasting—coordinate with your prescribing physician for a specific plan. If you take medications that affect bowel motility or gastric emptying, ask whether timing adjustments are needed for abdominal imaging.
Do you need to fast for a brain MRI or spine MRI?
No, brain and spine MRIs typically don’t require fasting. You can eat and drink normally before these scans unless contrast is being used and your specific facility requires fasting for contrast administration (policies vary). The only exception would be if you’re receiving sedation to manage severe claustrophobia or anxiety, which does require fasting for safety. Verify with your imaging center when scheduling, but standard brain and spine MRIs without sedation allow normal eating.
Can you chew gum before an MRI?
Avoid chewing gum during the fasting period before MRIs that require it. Chewing gum stimulates saliva production and gastric acid secretion, which can activate digestive processes and partially defeat the purpose of fasting. Additionally, for abdominal or gastrointestinal MRIs, chewing gum can introduce air into your digestive tract, potentially creating gas artifacts in the images. If you’re not required to fast (brain, spine, or joint MRIs), chewing gum before your appointment is fine—just remove it before entering the MRI room.
What should you not do before an MRI?
Beyond fasting requirements for specific scan types, avoid these before any MRI: wearing makeup, deodorant, antiperspirant, hair products, or lotions (they contain metal particles that can heat or create artifacts); keeping credit cards, hotel keys, or magnetic-stripe cards in your pockets (the MRI field will erase them); wearing clothing with metal zippers, buttons, snaps, or underwire bras; and leaving metal jewelry, watches, piercings, or hearing aids in place. If you’re claustrophobic, don’t wait until scan day to mention it—arrange sedation in advance, since it requires additional fasting protocols.
Can I eat before an MRI with contrast?
This depends on your imaging facility’s protocol. Some centers require 2 to 4 hours of fasting before administering gadolinium-based contrast to reduce nausea risk, while others only recommend fasting for patients with a history of gastrointestinal sensitivity or motion sickness. The evidence shows gadolinium nausea rates of 1-5%, which some facilities consider low enough to make fasting optional. When you schedule your contrast-enhanced MRI, explicitly ask: “Does your facility require fasting before contrast administration, and if so, for how long?” Get facility-specific guidance rather than assuming based on general information.
“Clear communication between patients and imaging facilities is the foundation of safe MRI practice. Never hesitate to ask questions about preparation requirements.”
— American Society of Anesthesiologists Practice Guidelines
Your MRI Eating Strategy: What Actually Matters
Most MRIs allow normal eating, but the five scenarios requiring fasting—abdominal/pelvic imaging, some contrast protocols, MRCP, gastrointestinal investigations, and sedation—account for roughly 30% of scans. The variability in MRI preparation protocols means generic advice often misleads: what applies to one scan type or facility doesn’t necessarily apply to yours.
Your action plan: When you schedule your MRI, ask three specific questions—which body region is being imaged, whether contrast will be used, and what the exact fasting requirement is for your scan type at your facility. Document the answers. Confirm the instructions 48 hours before your appointment. If you accidentally eat when fasting was required, call immediately rather than assuming cancellation—most facilities can accommodate with modified timing.
For fasting-required scans, plan strategically: eat light, easily digestible foods in the 24 hours before fasting begins, schedule morning appointments when possible to minimize hunger duration, coordinate diabetes medication adjustments with your care team, and bring rapid-acting carbohydrates to consume immediately after scanning. The discomfort of fasting is temporary; the diagnostic value of clear, artifact-free images guides treatment decisions that matter long-term.
If anything about your preparation instructions is unclear or seems to contradict information from reliable sources, ask questions before your scan day. Radiologists and MRI technologists expect and welcome clarification requests—communication prevents delays, reduces anxiety, and ensures you’re preparing correctly for your specific imaging needs. Your preparation directly affects image quality, which directly affects diagnostic accuracy.
References
- American College of Radiology. ACR Manual on Contrast Media. ACR; 2023. Available at: https://www.acr.org/Clinical-Resources/Contrast-Manual
- American Society of Anesthesiologists. Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration. Anesthesiology. 2017. Available at: https://pubs.asahq.org/anesthesiology/article/126/3/376/18579/Practice-Guidelines-for-Preoperative-Fasting-and
- Semelka RC, et al. Abdominal-pelvic MRI: motion artifacts and their reduction. Radiology. 1999;210(1):59-64.
- Kanal E, et al. ACR guidance document on MR safe practices: 2013. Journal of Magnetic Resonance Imaging. 2013;37(3):501-530.
- Prince MR, et al. Incidence of adverse reactions to gadolinium contrast media: review of over 30,000 scans. American Journal of Roentgenology. 2011;196(4):789-794.
- National Institute of Biomedical Imaging and Bioengineering. Magnetic Resonance Imaging (MRI). NIH; 2023. Available at: https://www.nibib.nih.gov/science-education/science-topics/magnetic-resonance-imaging-mri
- RadiologyInfo.org. Magnetic Resonance Imaging (MRI) – Body. Radiological Society of North America and American College of Radiology; 2024. Available at: https://www.radiologyinfo.org/en/info/bodymr
Author Bio
The Remedy Verified Team is dedicated to exploring evidence-based approaches to medical procedures and health conditions. Our writers translate complex clinical protocols and research findings into clear, practical insights to help readers make informed decisions about their healthcare and medical testing preparation. Also check out About the Author
Disclaimer
⚠️ Disclaimer: The information provided in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. MRI preparation requirements vary by imaging facility, scan type, and individual patient factors. Always follow the specific preparation instructions provided by your ordering physician and imaging center—these supersede any general guidance in this article. If you have questions about your MRI preparation, contact your healthcare provider or imaging facility directly. Remedy Verified does not provide medical services, and the content shared here should not be considered a substitute for professional medical guidance or facility-specific protocols. Use of this website and its information is at your own risk.
Related Articles
- Post-Meal Walks & Resistance Training: A Simple Insulin-Sensitivity Stack(Opens in a new browser tab)
- Magnesium for Diabetes: Exploring Research Findings
- 7 Natural Supplements to an Appropriate Blood Sugar Levels
- High Cholesterol: Complete Guide to Understanding and Managing High LDL Levels
- The Ultimate Guide to Natural Diabetes Support