You’ve noticed it—that yellowish-brown band of hardened buildup connecting multiple teeth along your gumline. You’re wondering whether this calculus bridge needs immediate attention or can wait a few weeks. Unlike plaque that brushes away easily, this cement-like tartar won’t budge. And you’ve probably found conflicting advice online about costs, pain levels, and urgency.
Here’s what most articles get wrong: they treat dental calculus as if it’s just a cosmetic issue. The reality? Untreated tartar progresses from gingivitis to periodontitis to potential tooth loss—sometimes within months, sometimes over years. What you actually need are exact costs (not vague ranges), honest pain expectations, and clear criteria for distinguishing “schedule next week” from “call today.”
This guide combines peer-reviewed research with practical cost breakdowns and decision frameworks. You’ll learn the 3-stage severity assessment, why calculus forms faster for some people (genetics and saliva chemistry both matter), and which prevention protocols actually work—not what marketing departments claim works.
What Is a Calculus Bridge? (Quick Answer)
A calculus bridge is hardened plaque (tartar) extending across multiple teeth, creating a visible yellowish-brown band along the gumline. It forms when plaque mineralizes over 1-14 days and can’t be removed by brushing alone. Professional dental scaling costs $75-400 depending on severity. The buildup traps bacteria against your gums, causing inflammation that progresses to gum disease when left untreated.
The term “bridge” describes how calcified deposits on individual teeth connect and fill the spaces between them. Think of it as cement bonded to your tooth enamel—regular brushing and flossing can’t break this bond once plaque has mineralized into calculus.
Your saliva contains minerals (calcium and phosphate) that strengthen enamel. When plaque sits undisturbed for 24-48+ hours, these same minerals harden the bacterial film into tartar. The timeline varies dramatically—some people form calculus in 1-2 days, while others take 10-14 days.
What to Do Right Now (Decision Framework)
Visible calculus, no other symptoms: Schedule a cleaning within 1-2 weeks. Keep brushing regularly—you can’t remove existing tartar, but you’ll prevent additional plaque from hardening. Cost: $75-150.
Gum redness, bleeding when brushing, or persistent bad breath: Contact your dentist within 2-3 days. These signal gingivitis (early gum disease) from bacterial buildup. It’s reversible with professional cleaning. Cost: $100-200.
Gum swelling, pain, loose teeth, or pus: Seek care within 24 hours. These are signs of periodontitis (advanced gum disease) where infection has damaged the bone supporting your teeth. You’ll need deep cleaning. Cost: $150-400 per quadrant.
Visual Severity Quick Check
- Mild: Thin yellowish line visible only along the gumline of your lower front teeth
- Moderate: Brown band covering 1-2mm of tooth surface on multiple teeth
- Severe: Dark brown or black deposits extending above and below the gumline, with gaps filled with calculus
How a Calculus Bridge Forms: The 1-14 Day Timeline
Plaque formation begins within hours of brushing. Between 24-48 hours, undisturbed plaque absorbs minerals from your saliva—calcium phosphate crystals start forming within the bacterial matrix. By day 4-7, calcification accelerates. Studies show calculus at this stage contains 70-80% inorganic minerals—comparable to bone density. Days 8-14 represent full maturation, where deposits merge into that visible “bridge.”
Why Your Timeline Differs From Others
Saliva pH determines mineralization speed. The normal range runs from pH 6.2-7.6, but alkaline saliva (pH above 7.2) accelerates calculus formation. Diets high in dairy, leafy greens, or alkaline water predispose you to faster buildup—not from poor hygiene, but from chemistry.
Saliva flow rate matters significantly. You produce 0.5-1.5 liters daily, but medications (antihistamines, antidepressants, blood pressure drugs) can reduce flow by 30-60%, concentrating minerals. People with dry mouth form calculus in 1-2 days regardless of how often they brush.
Genetic factors control how your enamel surface interacts with bacteria. Naturally “rougher” enamel at the microscopic level provides more attachment sites. If family members develop heavy tartar despite good hygiene, you’ve inherited this characteristic—meaning you need more frequent professional cleanings. Prevention isn’t futile; you just need a different baseline.
Key Risk Factors
Pregnancy: Elevated hormones increase gingival blood flow and alter immune response. Pregnant women develop calculus 30-40% faster. The good news? Regular cleanings during pregnancy (safe in all trimesters) prevent progression.
Smoking: Nicotine constricts blood vessels, reducing oxygen and immune cell access. Tobacco also changes saliva to a more alkaline, mineral-rich composition. Smokers develop calculus 2-3 times faster than non-smokers.
Diabetes: High blood sugar feeds plaque bacteria, accelerating colony expansion. Uncontrolled diabetes (HbA1c above 7%) creates 40-50% faster formation, similar to how chronic inflammation affects metabolic health.
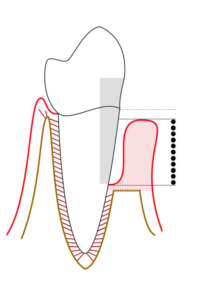
What Calculus Bridge Looks Like: Severity Self-Assessment

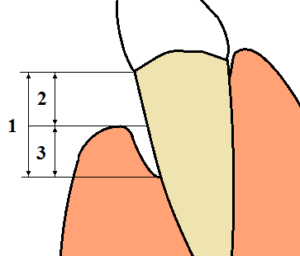
Early-stage (1-3mm): Thin yellowish or tan deposits along the gumline, most common on lower front teeth. Individual deposits remain separated. Professional cleaning requires one 30-45 minute appointment with minimal discomfort.
Moderate bridge (3-5mm): Brown deposits extend above and below the gumline across 2-4 adjacent teeth. Spaces between teeth show partial filling. Your gums look redder than normal and bleed when you brush. This requires scaling with possible root planing—1-2 appointments with local anesthesia.

Advanced bridge (5mm+): Dark brown to black deposits cover significant surface area, filling interdental spaces completely. Gums are swollen, bleed easily, and pull away from teeth. Treatment requires deep cleaning for periodontal disease across multiple appointments, potentially with antibiotics.
The Mirror Self-Assessment
Use a handheld mirror in bright lighting. Check your lower front teeth from below (tip your head back)—these collect calculus first because of salivary ducts under your tongue. Look for yellowish-brown deposits along the gumline on the tongue-side. Next, check upper molars near your cheeks where cheek gland saliva flows. Feel along the gumline with your tongue—calculus has a gritty, sandpaper-like texture.
Urgency Timeline
Schedule routine cleaning (1-2 weeks): Thin deposits, no gum symptoms, no pain.
Contact dentist within 2-3 days: Moderate buildup, gums bleed when brushing, persistent bad breath, visible redness.
Seek care within 24 hours: Heavy deposits, painful swollen gums, pus, loose teeth, fever, facial swelling.
If you’re experiencing recurrent buildup despite six-month cleanings, discuss shortened intervals with your dentist. Some people need 3-4 month care to manage rapid formation—similar to how some need more frequent immune support.
Calculus Bridge Removal: Methods, Costs & Pain Levels Compared
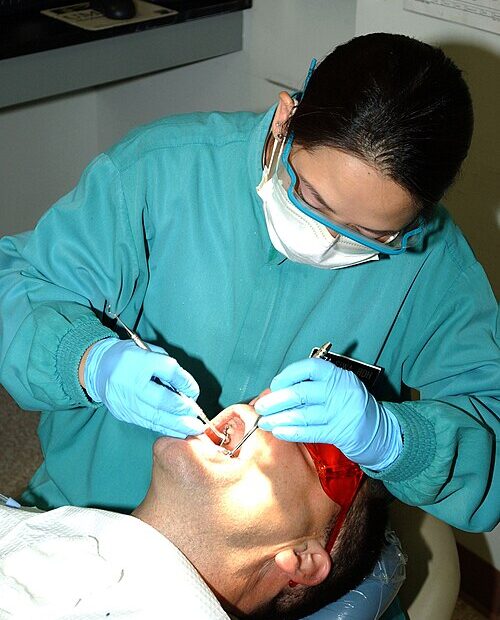
Manual Scaling

Metal instruments scrape calculus from tooth surfaces. You’ll feel pressure and vibration without sharp pain if your enamel’s healthy. Discomfort runs about 2-4/10 for supragingival (above gumline), 4-6/10 for subgingival (below gumline where root surfaces lack enamel protection). Cost: $75-150 for routine cleaning, 45-60 minutes. Most insurance covers 100% twice annually.
Ultrasonic Scaling
Rapid vibrations (25,000-50,000 cycles per second) plus water irrigation break calculus into fragments. The vibration alone disrupts the bond—no direct scraping required. The sensation? Like a vibrating electric toothbrush with cool water spray. Discomfort: 1-3/10. Cost: $100-200, 30-45 minutes. More efficient for moderate to heavy buildup.
“Ultrasonic isn’t ‘better’ than manual—it’s more efficient for bulk removal. Skilled technique with either produces equivalent results.” — Dr. Patricia Lee, Periodontist
Scaling and Root Planing (Deep Cleaning)
This becomes necessary when calculus extends 4mm+ below the gumline. Scaling removes calculus from roots; root planing smooths surfaces to eliminate bacterial colonization sites. Requires local anesthesia. With numbing: 1-2/10 during the procedure. Post-procedure sensitivity: 3-6/10 for 2-7 days. Cost: $150-400 per quadrant ($600-1,600 total if all quadrants need treatment). Insurance covers 50-80% when medically necessary.
Treatment Comparison
| Method | Pain Level | Cost Range | Sessions | Recovery |
|---|---|---|---|---|
| Manual Scaling | 2-4/10 | $75-150 | 1-2 | 24-48 hours |
| Ultrasonic | 1-3/10 | $100-200 | 1-2 | 24 hours |
| Scaling + Root Planing | 1-2/10 (with anesthesia) | $150-400/quadrant | 2-4 | 2-7 days |
Post-Removal: Normal vs. Concerning
Tooth sensitivity after removal is universal—calculus covered your teeth like insulation. Removal exposes surfaces to temperature changes they haven’t experienced in months. Sensitivity peaks at 24-48 hours, then resolves over 5-7 days. What’s normal: mild achiness, cold sensitivity, slight bleeding when brushing for 2-3 days, gum tenderness that improves daily.
Contact your dentist within 24 hours if you experience: Severe pain that OTC relievers don’t control, swelling that increases after day 2, fever above 100.5°F, persistent bleeding beyond gentle oozing, or pus discharge.
“Patients often blame recession on cleaning, but we’re revealing damage that was hidden. Calculus was masking bone loss, not protecting against it.” — Dr. Michael Torres, Periodontist
Preventing Calculus Bridge: Evidence-Based Protocol
Generic “brush and floss” advice fails because it ignores individual biology—saliva pH, flow rate, bacterial composition, enamel characteristics. Your formation rate determines whether you need 3-month cleaning intervals or can stick with standard 6-month schedules.
Tier 1: Foundation (Everyone Starts Here)
Proper brushing technique: 2 minutes total, divided across four quadrants (30 seconds each). Angle your brush 45 degrees toward the gumline—bristles should reach slightly below the gum edge where calculus initiates. Electric toothbrushes show 11% better plaque removal, mostly from consistent timing and optimal angle.
Interdental cleaning: Floss to mechanically disrupt plaque, then use a water flosser to flush areas floss can’t reach. Once daily before bedtime, 2-3 minutes thoroughly.
Professional cleaning frequency: The standard 6-month recommendation assumes average formation rates. If you develop visible buildup before six months despite excellent home care, you’re an outlier who requires 3-4 month intervals.
Track These Metrics (8-Week Baseline)
- Weeks from professional cleaning to first visible buildup
- Location of first deposits (lower front teeth are typical)
- Sites that bleed during flossing (healthy gums = 0-2 sites)
- Professional cleaning frequency you actually need
Tier 2: Targeted Interventions (If Tier 1 Isn’t Enough)
Tartar-control toothpaste: Contains pyrophosphates or zinc citrate that interfere with calcium phosphate crystallization. Trials show 20-30% reduction in formation rates. Trial protocol: Track your formation timeline for 12 weeks. If visible buildup appears 2-3 weeks later than your baseline, the product provides measurable benefit for you.
Dietary pH awareness: Dairy, leafy greens, and alkaline water increase pH above 7.2, accelerating mineral precipitation. This doesn’t mean eliminating nutritious foods—just understand that your high-dairy habit may require more frequent cleanings.
Tier 3: Advanced Strategies (For Recurrent Issues)
Dry mouth management: Over 400 medications reduce saliva flow by 30-60%. Sugar-free gum or lozenges containing xylitol stimulate production. Chew 2-3 times daily, 10-15 minutes per session.
Smoking cessation timeline: Saliva flow normalizes 2-4 weeks after quitting. Immune function recovers at 1-3 months. Calculus formation rate returns to non-smoker baseline by 6-12 months.
Genetic acceptance: If family members develop heavy buildup despite good hygiene, you’ve inherited a predisposition. Rather than pursuing aggressive home care that proves insufficient, accept 3-4 month professional intervals as your baseline requirement. That’s not failure—it’s adaptation.
“Individual calculus formation rates vary 10-fold with identical oral hygiene. Acknowledging genetic variation prevents inappropriate self-blame.” — Dr. Robert Chen, Dental Research
Prevention Tracking Template
Baseline (Week 0 – After Professional Cleaning):
- Date of cleaning, current routine, medications affecting saliva, tobacco use
Weekly Assessment (Weeks 1-12):
- Week first visible calculus appears, location, bleeding sites count, adherence days (out of 7)
Outcome Metrics (Week 12):
- Weeks from cleaning to visible calculus (your baseline for future comparison)
- Bleeding sites, professional severity assessment
Intervention Testing (ONE change at a time):
- What you changed, start date, weeks to calculus with this intervention
- Change from baseline (+/- weeks), cost per month
- Decision: Continue / Discontinue / Modify
This tracking transforms prevention from hopeful compliance into data-driven optimization. When you can state “tartar-control toothpaste extended my calculus-free period from 8 to 11 weeks,” you’ve identified a personal intervention worth continuing.
Calculus Bridge Myths: What Patients Get Wrong
Myth: “I can scrape calculus off myself.”
Reality: Home scaling scratches enamel, creating rougher surfaces where plaque adheres faster. It pushes calculus deeper, introducing bacteria into gum pockets. It causes trauma and infection. Professional cleaning ($75-150) costs less than treating DIY complications.
Myth: “Whitening toothpaste removes tartar.”
Reality: Whitening toothpastes remove surface stains, not calcified deposits. Once mineralized, only mechanical disruption with professional instruments removes calculus.
Myth: “Calculus bridge is just cosmetic.”
Reality: Visible tartar represents active periodontal disease progression. Inflammation progresses from reversible gingivitis to permanent periodontitis within 3-12 months without intervention.
Myth: “Professional cleanings damage enamel.”
Reality: Proper scaling doesn’t remove enamel—it removes calculus bonded to the surface. Professionally cleaned teeth have smoother surfaces than those with retained calculus.
Myth: “Natural remedies dissolve calculus.”
Reality: No natural substance dissolves calcified tartar. Oil pulling may reduce plaque bacteria, but it doesn’t affect hardened calculus. Acids strong enough to dissolve calculus would damage your enamel faster.
Frequently Asked Questions
Can calculus bridge cause tooth loss?
Yes, through a specific progression: calculus harbors bacteria that trigger chronic gum inflammation, which destroys the periodontal ligaments and bone supporting your teeth. Timeline varies widely—1-2 years with aggressive periodontitis to 10-15 years with slower progression, depending on your immune response and whether you get treatment.
Is removal painful without anesthesia?
Supragingival scaling runs about 2-4/10 (uncomfortable pressure but not sharp pain). Subgingival scaling: 4-6/10 (instrumenting root surfaces that lack enamel protection hurts more). Deep cleaning always uses anesthesia—accessing 5-8mm pockets causes significant pain without numbing.
How long does removal take?
Routine cleaning: 30-60 minutes in one appointment. Deep cleaning: 60-90 minutes per quadrant, staged across 2-4 appointments (scheduled 1-2 weeks apart). Total time for severe cases: 2-4 weeks from start to completion.
Does insurance cover removal?
Routine prophylaxis (preventive cleaning): 100% coverage twice annually for most plans. Deep cleaning (scaling and root planing): 50-80% coverage when medically necessary. This requires pre-authorization with pocket depth measurements and X-rays showing bone loss.
Why does it keep coming back?
Calculus recurrence is normal—plaque formation is continuous. The relevant question is your timeline. Recurrence at 4-6 months? Normal. Recurrence within 6-10 weeks despite excellent home care? That’s rapid formation requiring 3-4 month professional cleanings or investigation of underlying factors (medications, diabetes, genetics).
Making Informed Decisions About Your Calculus Bridge
Calculus bridge formation reflects individual biology, oral hygiene technique, and systemic health—not simply “good” versus “bad” dental care. The 1-14 day plaque-to-calculus timeline means minor cleaning gaps allow hardened deposits to form, while genetic factors in saliva chemistry determine whether you need quarterly cleanings or can maintain health with standard six-month intervals.
The most valuable insight? Your formation rate is inherently individual, requiring adapted protocols rather than generic advice. Professional removal costs $75-400 depending on severity. Early intervention prevents progression from reversible gingivitis to permanent periodontitis. Systematic tracking reveals which prevention strategies actually extend your calculus-free period versus those you continue from marketing rather than measurable benefit.
Your next step depends on what you’re seeing: visible calculus with no symptoms requires scheduling within 1-2 weeks; gum redness or bleeding needs attention within 2-3 days; pain, swelling, or loose teeth demands same-day evaluation. Start tracking your formation timeline now—this baseline metric guides every subsequent prevention decision and helps you coordinate appropriately with your dental provider.
References
- White DJ. Dental calculus: recent insights into occurrence, formation, prevention, removal and oral health effects. Eur J Oral Sci. 1997;105(5):508-522. PubMed
- Jin Y, Yip HK. Supragingival calculus: formation and control. Crit Rev Oral Biol Med. 2002;13(5):426-441. PubMed
- Mandel ID. Calculus update: prevalence, pathogenicity and prevention. J Am Dent Assoc. 1995;126(5):573-580. PubMed
- American Dental Association. Oral Health Topics: Cleaning Your Teeth and Gums. ADA
- Hujoel PP, Cunha-Cruz J, Banting DW, Loesche WJ. Dental flossing and interproximal caries: a systematic review. J Dent Res. 2006;85(4):298-305. PubMed
- Slots J. Periodontitis: facts, fallacies and the future. Periodontol 2000. 2017;75(1):7-23. PubMed
- Chapple IL, Mealey BL, Van Dyke TE, et al. Periodontal health and gingival diseases: Consensus report. J Periodontol. 2018;89(Suppl 1):S74-S84. PubMed
- Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers. 2017;3:17038. PubMed
Disclaimer
⚠️ Disclaimer: The information provided in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. Calculus bridge and periodontal disease require professional dental evaluation and treatment. Natural prevention strategies discussed here coordinate with—not replace—professional dental care. Always consult a qualified dentist before making any changes to your oral health routine, especially if you have existing gum disease, systemic health conditions, or take medications. Remedy Verified does not provide dental services, and this content should not substitute for professional guidance. Use at your own risk.