Triple Threat Action Plan: Managing High Blood Sugar, High Cholesterol & High Blood Pressure
Understanding Your Metabolic Syndrome Diagnosis
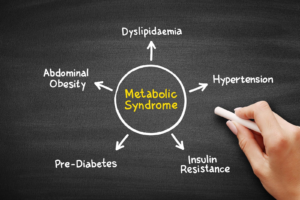
When you have elevated blood sugar, cholesterol, and blood pressure occurring together, you’re dealing with what medical professionals call metabolic syndrome (a cluster of metabolic abnormalities that significantly increase cardiovascular and diabetes risk). This isn’t simply three separate problems—these conditions are interconnected through complex metabolic pathways involving insulin resistance, inflammation, and abdominal obesity.
The encouraging news is that metabolic syndrome responds exceptionally well to comprehensive lifestyle interventions. Studies consistently demonstrate that addressing the root causes simultaneously provides more effective results than treating each condition independently. Furthermore, the same interventions that improve blood sugar often benefit cholesterol and blood pressure levels.
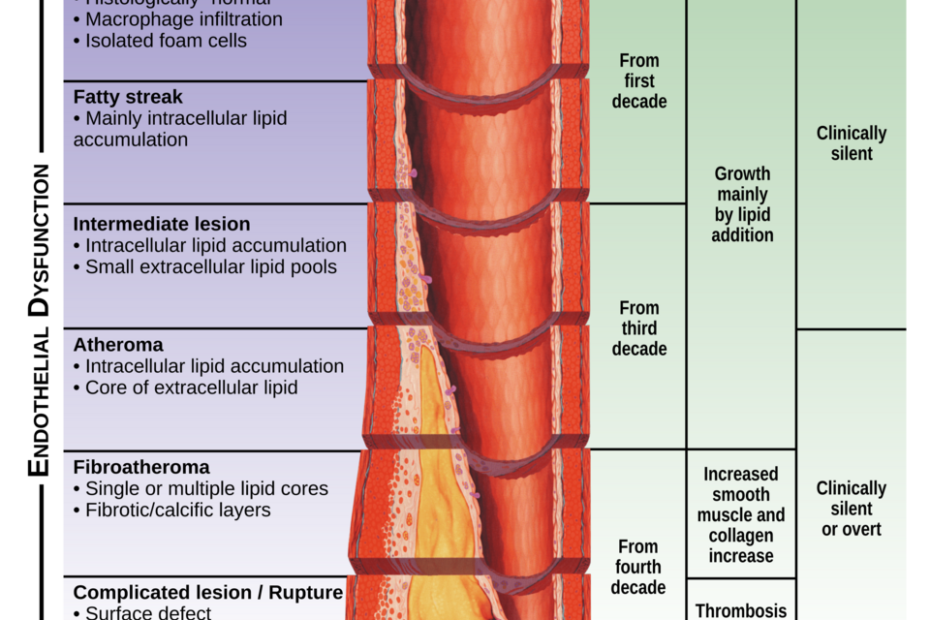
The Interconnected Nature of Your Conditions
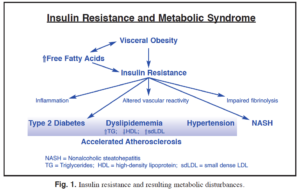
Understanding how these conditions reinforce each other helps explain why a comprehensive approach works best:
Phase 1: Foundation Building (Weeks 1-4)
Your initial phase focuses on establishing sustainable habits while beginning to address all three conditions simultaneously. Research shows that gradual implementation leads to better long-term compliance and more sustainable results.

Dietary Foundation
- Adopt Mediterranean-style eating: Emphasize vegetables, fruits, whole grains, lean proteins, and healthy fats
- Reduce refined carbohydrates: Eliminate sugary drinks, white bread, and processed foods
- Control portions: Use the plate method (½ vegetables, ¼ protein, ¼ whole grains)
- Limit sodium: Aim for less than 2,300mg daily to support blood pressure goals
Movement & Monitoring
- Start walking: Begin with 15-20 minutes daily, gradually increasing duration
- Home monitoring: Check blood pressure and blood sugar as recommended by your healthcare provider
- Sleep hygiene: Aim for 7-9 hours nightly with consistent sleep/wake times
- Stress management: Implement 10-15 minutes daily of deep breathing or meditation
Week 1-2 Specific Actions:
Daily Implementation Checklist:
- Replace one sugary drink with water or unsweetened tea
- Add one extra serving of vegetables to lunch and dinner
- Take a 15-minute walk after meals when possible
- Record blood pressure and blood sugar readings as directed
- Practice 5 minutes of deep breathing before bed
- Plan tomorrow’s meals and snacks in advance

During this initial phase, focus on consistency rather than perfection. Small, sustainable changes compound over time to produce significant health improvements. Additionally, this gradual approach allows your body to adapt while reducing the risk of dramatic blood sugar or blood pressure fluctuations.
Phase 2: Targeted Interventions (Weeks 5-12)
Once your foundation habits are established, Phase 2 introduces more specific interventions targeting the metabolic pathways underlying your conditions. This phase incorporates evidence-based supplements and more structured lifestyle modifications.
Evidence-Based Supplement Protocol
Research supports specific supplements that address multiple aspects of metabolic syndrome simultaneously. However, always consult your healthcare provider before starting any supplement regimen, especially when taking medications for your conditions.
| Supplement | Dosage | Primary Benefits | Evidence Level |
|---|---|---|---|
| Chromium | 200-400 mcg daily | Improved insulin sensitivity, glucose metabolism | Strong |
| Magnesium | 300-400 mg daily | Blood pressure reduction, insulin function | Strong |
| Omega-3 Fatty Acids | 1000-2000 mg EPA/DHA daily | Triglyceride reduction, anti-inflammatory | Very Strong |
| Berberine | 500 mg twice daily | Glucose control, cholesterol management | Strong |
| CoQ10 | 100-200 mg daily | Blood pressure support, cellular energy | Moderate |
Advanced Dietary Strategies

Phase 2 incorporates more sophisticated nutritional approaches based on current metabolic syndrome research:
Intermittent Fasting Protocol
Consider implementing a 12-14 hour eating window (such as eating between 8 AM and 8 PM). Research demonstrates that time-restricted eating (limiting food intake to specific hours each day) can improve insulin sensitivity, reduce inflammation, and support healthy blood pressure levels.
Strategic Carbohydrate Timing
Consume most carbohydrates earlier in the day when insulin sensitivity is naturally higher. Focus on complex carbohydrates paired with protein and healthy fats to minimize blood sugar spikes. Moreover, this approach helps optimize metabolic function throughout the day.
Anti-Inflammatory Food Focus
Emphasize foods rich in polyphenols and antioxidants that combat the chronic inflammation underlying metabolic syndrome. Include berries, leafy greens, fatty fish, nuts, olive oil, and green tea in your daily routine.
Phase 3: Optimization and Fine-Tuning (Weeks 13-26)
Phase 3 focuses on optimizing your progress through more advanced strategies while maintaining the habits established in earlier phases. This phase emphasizes personalization based on your individual responses and progress.
Exercise Progression for Metabolic Health
Research consistently shows that specific exercise protocols provide superior benefits for metabolic syndrome management. The key is combining aerobic activity with resistance training while maintaining consistency.
Week 13-26 Exercise Goals:
- Aerobic Exercise: 150 minutes moderate intensity weekly (brisk walking, swimming, cycling)
- Resistance Training: 2-3 sessions weekly targeting major muscle groups
- High-Intensity Intervals: 1-2 sessions weekly (if cleared by your healthcare provider)
- Daily Movement: 10,000+ steps daily with regular movement breaks
- Flexibility Work: Yoga or stretching 2-3 times weekly for stress management
Advanced Monitoring and Adjustments
Phase 3 introduces more sophisticated monitoring to optimize your interventions based on measurable results. This data-driven approach helps identify which strategies work best for your individual physiology.
Key Biomarkers to Track:
| Measurement | Target Range | Frequency | Significance |
|---|---|---|---|
| Fasting Blood Glucose | <100 mg/dL | Weekly | Direct diabetes risk indicator |
| HbA1c | <5.7% | Every 3 months | Long-term blood sugar control |
| Blood Pressure | <130/80 mmHg | Daily | Cardiovascular risk assessment |
| Total Cholesterol | <200 mg/dL | Every 2-3 months | Overall lipid status |
| Triglycerides | <150 mg/dL | Every 2-3 months | Metabolic syndrome marker |
| Waist Circumference | <40″ (men), <35″ (women) | Weekly | Visceral fat assessment |
Personalization Strategies
By Phase 3, you should have enough data to personalize your approach based on which interventions provide the most significant improvements for your specific situation.
Long-Term Maintenance and Troubleshooting
Successful long-term management of metabolic syndrome requires ongoing attention, periodic adjustments, and strategies for handling setbacks. Research demonstrates that sustained lifestyle changes provide the most significant long-term benefits.
Common Challenges and Solutions
Blood Sugar Plateaus
If blood sugar improvements stall, consider adjusting meal timing, increasing fiber intake, or consulting with your healthcare provider about alpha-lipoic acid supplementation. Sometimes rotating between different approaches prevents metabolic adaptation.
Blood Pressure Resistance
Persistent high blood pressure may require evaluating stress management techniques, sleep quality improvement, or discussing potassium-rich foods with your healthcare provider. Additionally, some individuals benefit from meditation or other stress-reduction practices.
Cholesterol Management
Stubborn cholesterol levels often respond to increasing soluble fiber intake, adding plant sterols, or incorporating more omega-3 fatty acids. Furthermore, resistance training can significantly improve HDL cholesterol levels.
Seasonal Adjustments
Your management plan may need seasonal modifications to maintain effectiveness year-round. Winter months might require indoor exercise alternatives and vitamin D supplementation, while summer demands careful hydration management and heat-related precautions during exercise.
Medical Integration and Safety Considerations
Throughout your journey, maintaining close communication with your healthcare team remains essential. Metabolic syndrome management often involves medication adjustments as lifestyle improvements take effect.
Essential Medical Coordination:
- Regular Check-ins: Schedule follow-ups every 3-4 months initially, then every 6 months
- Medication Reviews: Discuss potential dose reductions as biomarkers improve
- Supplement Clearance: Review all supplements for interactions with medications
- Emergency Plans: Know when to contact healthcare providers for concerning changes
- Specialist Referrals: Consider endocrinologist, cardiologist, or registered dietitian consultations
- Annual Assessments: Comprehensive metabolic panels and cardiovascular risk evaluations
Success Metrics and Realistic Expectations
Setting realistic expectations helps maintain motivation while recognizing meaningful progress. Research shows that even modest improvements in metabolic syndrome components significantly reduce long-term health risks.
Timeline for Expected Improvements
Celebrating Milestones
Recognize and celebrate non-scale victories that indicate improving metabolic health. These might include better energy levels, improved sleep quality, reduced medication needs, enhanced mood, or increased physical capabilities. These improvements often precede measurable biomarker changes and represent meaningful progress.
References
- Frontiers in Pharmacology. (2024). Research advances in the therapy of metabolic syndrome. https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1364881/full
- NCBI. (2024). Metabolic Syndrome – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK459248/
- PMC. (2024). Metabolic syndrome – a new definition and management guidelines. https://pmc.ncbi.nlm.nih.gov/articles/PMC9479724/
- Circulation. Diagnosis and Management of the Metabolic Syndrome. https://www.ahajournals.org/doi/10.1161/circulationaha.105.169404
- Sage Journals. (2024). Metabolic Syndrome: An Updated Review on Diagnosis and Treatment for Primary Care Clinicians. https://journals.sagepub.com/doi/10.1177/21501319241309168
- Medscape. (2024). Metabolic Syndrome Treatment & Management. https://emedicine.medscape.com/article/165124-treatment
- Frontiers in Physiology. (2024). Physical activity in metabolic syndrome. https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2024.1365761/full
- Molecular Medicine. (2024). The interplay of factors in metabolic syndrome: understanding its roots and complexity. https://molmed.biomedcentral.com/articles/10.1186/s10020-024-01019-y
- International Diabetes Federation. The IDF consensus worldwide definition of the Metabolic Syndrome. https://idf.org/media/uploads/2023/05/attachments-30.pdf
- Journal of Clinical and Translational Hepatology. (2024). Guideline for the Prevention and Treatment of Metabolic Dysfunction-associated Fatty Liver Disease. https://www.xiahepublishing.com/2310-8819/JCTH-2024-00311
Medical Disclaimer
This action plan is for educational purposes only and does not constitute medical advice. Metabolic syndrome, high blood sugar, high cholesterol, and high blood pressure are serious medical conditions requiring professional medical supervision. Always consult with qualified healthcare providers before implementing any aspect of this plan, starting supplements, or making changes to medications. Individual results may vary, and this information should complement, not replace, professional medical care. Monitor your conditions closely and seek immediate medical attention if you experience concerning symptoms.