High Blood Pressure Management: Evidence-Based Guide to Supplements, Foods & Medications
Understanding High Blood Pressure and Its Impact
High blood pressure (hypertension) represents one of the most significant preventable risk factors for cardiovascular disease and all-cause mortality worldwide. Currently, approximately 1.39 billion people globally have hypertension, making it a critical public health concern that demands comprehensive management strategies.
Blood pressure readings consist of two numbers: systolic pressure (when your heart beats) and diastolic pressure (when your heart rests between beats). Normal blood pressure is defined as less than 120/80 mmHg, while elevated blood pressure begins at 130/80 mmHg according to current guidelines.
When blood pressure remains elevated over time, it forces your heart to work harder to pump blood throughout your body. Consequently, this increased workload can damage arteries, reducing their ability to deliver adequate blood to vital organs. Furthermore, persistent high blood pressure leads to hypertension-mediated organ damage affecting the heart, brain, kidneys, blood vessels, and eyes.
The Mechanism Behind Blood Pressure Regulation
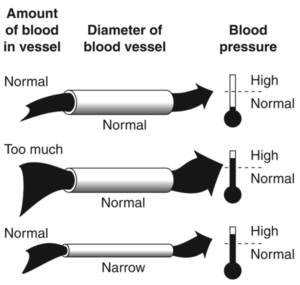
Blood pressure regulation involves a complex interplay between multiple systems in your body. The renin-angiotensin-aldosterone system (RAAS) plays a central role by controlling sodium balance and blood vessel constriction. Additionally, your sympathetic nervous system influences heart rate and vessel tone, while your kidneys regulate fluid balance.
Understanding these mechanisms proves essential because different treatment approaches target specific pathways. Moreover, this knowledge helps explain why combination therapies often work more effectively than single interventions.
Evidence-Based Supplements for Blood Pressure Management
Research has identified several supplements with demonstrated efficacy for lowering blood pressure. However, it’s crucial to understand that supplements work best as part of a comprehensive approach rather than standalone treatments.
Magnesium: The Mineral for Vessel Relaxation
Magnesium supplementation has shown consistent blood pressure-lowering effects in multiple studies. Magnesium deficiency (when cells don’t have adequate magnesium for optimal function) contributes to high blood pressure by affecting calcium regulation in blood vessels and heart muscle.
How Magnesium Lowers Blood Pressure:
Clinical studies demonstrate that magnesium supplementation reduces both systolic and diastolic blood pressure. Specifically, research shows reductions of approximately 2-3 mmHg systolic and 1-2 mmHg diastolic pressure with consistent supplementation.
Potassium: The Sodium Balancer
Potassium may be the best-known nutritional supplement for blood pressure regulation. It works by helping sodium leave your body through urine while promoting blood vessel relaxation. Research consistently shows that increasing potassium intake through food or supplements helps reduce high blood pressure levels.
The mechanism involves potassium’s role in the sodium-potassium pump, which maintains proper fluid balance inside and outside cells. Additionally, potassium helps counteract sodium’s blood pressure-raising effects by promoting vasodilation.
| Supplement | Typical Dosage | Blood Pressure Effect | Key Benefits |
|---|---|---|---|
| Magnesium | 500-1000 mg daily | -2.8/-1.6 mmHg | Vessel relaxation, inflammation reduction |
| Potassium | 2000-4000 mg daily | -2.1 mmHg systolic | Sodium balance, vasodilation |
| CoQ10 | 100-300 mg daily | -3 to -7 mmHg | Cellular energy, antioxidant effects |
| Vitamin C | 300-1000 mg daily | -2 to -4 mmHg | Antioxidant protection, nitric oxide support |
Coenzyme Q10: Cellular Energy for Heart Health
Coenzyme Q10 (CoQ10) is a vitamin-like molecule that helps cells produce energy while acting as a powerful antioxidant. Recent research demonstrates that CoQ10 supplements significantly reduce systolic blood pressure, with some studies showing reductions of 3-7 mmHg.
CoQ10 works by improving endothelial function (the inner lining of blood vessels) and supporting cellular energy production in heart muscle. Furthermore, its antioxidant properties help protect blood vessels from oxidative damage that contributes to hypertension.
Vitamin C: Antioxidant Protection for Vessels
Vitamin C supplementation shows modest but consistent blood pressure-lowering effects. In studies involving people with high blood pressure, taking 300-1000 mg daily of vitamin C significantly reduced their levels. The mechanism involves vitamin C’s role in protecting blood vessel linings from damage while supporting nitric oxide production.
Vitamin C deficiency represents a risk factor for high blood pressure. The antioxidant activity of vitamin C helps protect the lining of blood vessels from damage and increases nitric oxide, which helps relax arterial walls.
Emerging Supplements with Promise
Several other supplements show potential for blood pressure management, though research remains ongoing:
- Beetroot extract: Contains nitrates that convert to nitric oxide, promoting vasodilation
- Omega-3 fatty acids: Support endothelial function and reduce inflammation
- Probiotics: May influence blood pressure through gut-brain-heart axis
- Melatonin: Shows modest blood pressure reductions, particularly in people with elevated levels
DASH Diet: The Gold Standard for Blood Pressure Nutrition
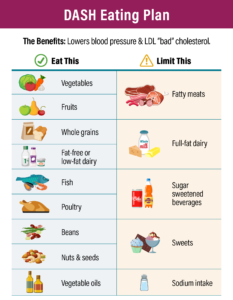
The Dietary Approaches to Stop Hypertension (DASH) diet represents the most extensively studied and proven dietary approach for blood pressure management. Developed through rigorous clinical trials, DASH has consistently demonstrated significant blood pressure reductions while providing additional cardiovascular benefits.
Core Principles of the DASH Diet
The DASH eating plan emphasizes foods naturally rich in potassium, calcium, magnesium, and fiber while limiting sodium, saturated fat, and added sugars. Research shows that these nutrient-dense foods work synergistically to support healthy blood pressure levels.
Unlike restrictive diets, DASH provides a balanced, sustainable approach to eating that includes foods from all major food groups. Furthermore, the diet promotes portion control and emphasizes minimally processed, whole foods over packaged alternatives.
DASH Diet Food Group Recommendations (2000 calories daily):
Specific Foods That Lower Blood Pressure
Certain foods demonstrate particular efficacy for blood pressure reduction based on their nutrient profiles and bioactive compounds:
Potassium-Rich Foods
Foods high in potassium help counteract sodium’s effects while supporting proper fluid balance. Excellent sources include bananas, oranges, spinach, sweet potatoes, and white beans. These foods provide potassium along with other beneficial nutrients like magnesium and fiber.
Magnesium-Rich Options
Magnesium-containing foods support blood vessel relaxation and proper heart rhythm. Top sources include dark leafy greens, nuts, seeds, whole grains, and dark chocolate. Additionally, these foods often provide other heart-healthy nutrients.
Nitric Oxide Boosters
Foods that support nitric oxide production help blood vessels relax and improve circulation. Beetroot, dark leafy greens, and pomegranates are particularly effective. Moreover, these foods contain antioxidants that protect blood vessels from damage.
The Sodium Connection
Sodium reduction plays a crucial role in blood pressure management for most people. The DASH diet recommends limiting sodium to 2,300 mg daily, with even greater benefits at 1,500 mg daily. This represents a significant reduction from the typical American intake of over 3,400 mg daily.
Processed foods account for approximately 70% of dietary sodium intake. Therefore, focusing on whole, unprocessed foods naturally reduces sodium while increasing beneficial nutrients. Additionally, gradually reducing sodium allows taste preferences to adapt over time.
Blood Pressure Medications: Proven Pharmaceutical Options
When lifestyle modifications and supplements aren’t sufficient to achieve target blood pressure levels, medications provide proven effectiveness for reducing cardiovascular risk. Modern blood pressure medications work through different mechanisms, allowing healthcare providers to tailor treatment to individual needs.
ACE Inhibitors: Blocking the Pressure System
Angiotensin-converting enzyme (ACE) inhibitors work by blocking an enzyme that produces angiotensin II, a powerful blood vessel constrictor. By reducing angiotensin II production, these medications help blood vessels relax and lower blood pressure effectively.
ACE inhibitors offer benefits beyond blood pressure reduction. They provide kidney protection, reduce heart failure risk, and may prevent certain cardiovascular events. Common examples include lisinopril, enalapril, and captopril.
Most people tolerate ACE inhibitors well, though some develop a dry cough due to increased bradykinin levels. This side effect typically resolves when switching to an alternative medication class.
ARBs: Blocking the Receptors
Angiotensin receptor blockers (ARBs) prevent angiotensin II from binding to receptors on blood vessels, achieving similar effects to ACE inhibitors through a different mechanism. ARBs often cause fewer side effects, particularly the dry cough associated with ACE inhibitors.
Recent large-scale studies demonstrate that ARBs provide equivalent cardiovascular protection to ACE inhibitors while offering better tolerability. This makes ARBs an excellent first-line option for many patients starting blood pressure treatment.
Diuretics: Reducing Fluid Volume
Diuretics, commonly called “water pills,” help the kidneys remove excess sodium and water from the body. This reduces blood volume, which in turn lowers blood pressure. Different types of diuretics work at various locations in the kidney.
Thiazide and thiazide-like diuretics are preferred for blood pressure treatment because they provide cardiovascular protection while causing fewer electrolyte imbalances than other diuretic types. Examples include hydrochlorothiazide and chlorthalidone.
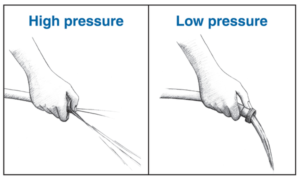
Calcium Channel Blockers: Relaxing Blood Vessels
These medications prevent calcium from entering heart and blood vessel cells, which helps blood vessels relax and reduces heart workload. Two main types exist: dihydropyridines (affecting mainly blood vessels) and non-dihydropyridines (affecting both heart and blood vessels).
Calcium channel blockers work particularly well in certain populations and can be combined safely with other blood pressure medications for enhanced effectiveness.
| Medication Class | How It Works | Common Examples | Key Benefits |
|---|---|---|---|
| ACE Inhibitors | Block angiotensin II production | Lisinopril, Enalapril | Kidney protection, heart failure prevention |
| ARBs | Block angiotensin II receptors | Losartan, Valsartan | Similar to ACE inhibitors, fewer side effects |
| Diuretics | Remove excess sodium and water | Hydrochlorothiazide, Chlorthalidone | Proven cardiovascular protection |
| Calcium Channel Blockers | Relax blood vessels | Amlodipine, Nifedipine | Effective in diverse populations |
Beta-Blockers: Slowing Heart Rate
Beta-blockers reduce blood pressure by blocking the effects of adrenaline on the heart and blood vessels. This slows heart rate and reduces the force of heart contractions, ultimately lowering blood pressure.
While not typically first-line treatments for uncomplicated hypertension, beta-blockers provide excellent options for people with heart failure, previous heart attacks, or certain heart rhythm disorders.
Lifestyle Modifications That Make a Difference
Beyond supplements, diet, and medications, several lifestyle factors significantly impact blood pressure levels. These modifications often provide the foundation for successful blood pressure management while potentially reducing medication needs.
Exercise: The Natural Blood Pressure Medicine
Regular physical activity ranks among the most effective non-pharmacological interventions for blood pressure reduction. Aerobic exercise (sustained activity that increases heart rate and breathing) provides the most consistent benefits, though resistance training also contributes to blood pressure improvement.
Exercise lowers blood pressure through multiple mechanisms: improving heart efficiency, promoting weight loss, reducing inflammation, and enhancing insulin sensitivity. Furthermore, regular activity helps blood vessels maintain flexibility and responsiveness.
Effective Exercise Guidelines for Blood Pressure:
- Aim for at least 150 minutes of moderate-intensity aerobic activity weekly
- Include 2-3 resistance training sessions per week
- Start gradually if sedentary, building up to recommended levels
- Choose activities you enjoy to maintain long-term consistency
- Monitor blood pressure response, especially if taking medications
Weight Management: Reducing the Load
Excess weight increases blood pressure by requiring the heart to pump blood to additional tissue while potentially affecting kidney function and hormone regulation. Studies show that losing just 5-10 pounds can produce meaningful blood pressure reductions.
Weight loss benefits blood pressure through multiple pathways: reducing cardiac workload, improving insulin sensitivity, decreasing inflammation, and supporting better sleep quality. Moreover, sustainable weight management often involves adopting other heart-healthy habits.
Stress Management: Calming the System
Chronic stress contributes to elevated blood pressure through multiple mechanisms, including increased cortisol production, sympathetic nervous system activation, and promotion of unhealthy behaviors. Therefore, effective stress management represents a crucial component of comprehensive blood pressure control.
Research supports various stress-reduction techniques for blood pressure improvement, including meditation, deep breathing exercises, yoga, and regular physical activity. Additionally, adequate sleep and social connection contribute to stress resilience.
Sleep Quality: Restoration and Recovery
Poor sleep quality and insufficient sleep duration independently increase blood pressure risk. During sleep, blood pressure naturally decreases, providing cardiovascular recovery time. Disrupted sleep patterns can interfere with this natural rhythm.
Sleep apnea represents a particularly important condition affecting both sleep quality and blood pressure. This condition causes repeated breathing interruptions during sleep, leading to oxygen fluctuations and stress hormone release that elevate blood pressure.
Integrative Approaches: Combining Strategies Effectively
The most effective blood pressure management typically involves combining multiple evidence-based approaches rather than relying on any single intervention. This comprehensive strategy addresses the multifactorial nature of hypertension while maximizing potential benefits.
The Synergistic Effect
When lifestyle modifications, dietary changes, supplements, and medications work together, their combined effects often exceed the sum of individual components. For example, the DASH diet enhances medication effectiveness while exercise improves supplement absorption and utilization.
This synergistic approach also allows for lower medication doses in some cases, potentially reducing side effects while maintaining therapeutic benefits. Furthermore, comprehensive approaches address underlying causes rather than just symptoms.
Building Your Comprehensive Blood Pressure Plan:
Monitoring and Adjustment

Successful blood pressure management requires ongoing monitoring and periodic adjustments to your approach. Home blood pressure monitoring provides valuable information about treatment effectiveness while helping identify patterns related to diet, exercise, stress, and medication timing.
Regular healthcare provider consultations ensure that your management plan remains optimal as your health status changes. Additionally, periodic laboratory tests can identify potential side effects or the need for dosage adjustments.
Personalization Considerations
Individual responses to blood pressure interventions vary significantly based on factors including genetics, age, underlying health conditions, and lifestyle factors. Therefore, personalizing your approach based on these factors improves both effectiveness and sustainability.
Some people respond better to sodium reduction, while others benefit more from potassium increases. Similarly, certain supplements work more effectively in specific populations or with particular medication combinations.
Special Considerations and Precautions
While the strategies discussed provide safe, effective options for most people, certain situations require special consideration or medical supervision. Understanding these circumstances helps ensure safe, appropriate blood pressure management.
Medication Interactions
Several supplements can interact with blood pressure medications, potentially causing excessive blood pressure reduction or affecting medication absorption. For example, potassium supplements can be dangerous when combined with ACE inhibitors or ARBs, as both increase potassium levels.
Always inform healthcare providers about all supplements, herbs, and over-the-counter medications you’re taking. This information helps prevent dangerous interactions while optimizing treatment effectiveness.
Pregnancy and Blood Pressure
Blood pressure management during pregnancy requires specialized approaches, as some medications and supplements can affect fetal development. Pregnant women should work closely with healthcare providers to ensure safe, effective treatment.
Gestational hypertension and preeclampsia represent serious conditions requiring immediate medical attention. However, lifestyle modifications like the DASH diet can often help manage milder blood pressure elevations during pregnancy.
Age-Related Considerations
Blood pressure management strategies may need adjustment based on age-related factors. Older adults often have more complex medication regimens and may be more sensitive to blood pressure changes, requiring careful monitoring and gradual adjustments.
Conversely, younger adults may benefit more from lifestyle-focused approaches before requiring medications. Age-appropriate exercise recommendations and supplement dosages help optimize safety and effectiveness across different life stages.
Future Directions in Blood Pressure Management
Emerging research continues to expand our understanding of blood pressure regulation and treatment options. Digital health technologies, personalized medicine approaches, and novel therapeutic targets show promise for improving blood pressure management outcomes.
Digital Health Integration
Smartphone apps, wearable devices, and remote monitoring systems increasingly support blood pressure management through improved tracking, medication reminders, and lifestyle coaching. These technologies can enhance adherence while providing healthcare providers with more comprehensive patient data.
Research demonstrates that digital therapeutics can produce meaningful blood pressure reductions when combined with traditional approaches. Furthermore, these tools can help identify patterns and triggers that might otherwise go unnoticed.
Personalized Medicine Advances
Genetic testing and biomarker analysis may eventually guide treatment selection, helping identify which interventions work best for individual patients. This precision medicine approach could reduce trial-and-error periods while optimizing treatment effectiveness.
Research into gut microbiome influences on blood pressure also shows promise for developing targeted probiotic therapies. Additionally, studies of circadian rhythm effects may lead to optimized medication timing strategies.
References
- Healthline. (2025). 11 Supplements That May Help Lower Blood Pressure. https://www.healthline.com/nutrition/supplements-lower-blood-pressure
- GoodRx. (2024). 10 Best Supplements to Help Lower High Blood Pressure. https://www.goodrx.com/conditions/hypertension/best-high-blood-pressure-supplements
- PMC. (2023). Vitamins and Minerals for Blood Pressure Reduction in the General, Normotensive Population. https://pmc.ncbi.nlm.nih.gov/articles/PMC10574336/
- WebMD. (2024). What to Know About Herbal Supplements and Blood Pressure. https://www.webmd.com/hypertension-high-blood-pressure/what-to-know-about-herbal-supplements-and-blood-pressure
- NHLBI. DASH Eating Plan. https://www.nhlbi.nih.gov/education/dash-eating-plan
- Mayo Clinic. (2024). High blood pressure (hypertension): Diagnosis & treatment. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/diagnosis-treatment/drc-20373417
- American Heart Association. Two types of blood pressure meds prevent heart events equally, but side effects differ. https://newsroom.heart.org/news/two-types-of-blood-pressure-meds-prevent-heart-events-equally-but-side-effects-differ
- Nature. (2025). Hypertension research 2024 update and perspectives: blood pressure management. https://www.nature.com/articles/s41440-025-02130-1
- American Heart Association. Types of Blood Pressure Medications. https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
- NCBI. (2023). DASH Diet To Stop Hypertension – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK482514/
- European Heart Journal. (2024). 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. https://academic.oup.com/eurheartj/article/45/38/3912/7741010
- American Heart Association. Managing Blood Pressure with a Heart-Healthy Diet. https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/managing-blood-pressure-with-a-heart-healthy-diet
Medical Disclaimer
This article is for informational purposes only and does not constitute medical advice. High blood pressure is a serious medical condition that requires professional medical supervision. Always consult with a qualified healthcare provider before making changes to your blood pressure management plan, starting new supplements, or adjusting medications. Individual results may vary, and this information should not replace professional medical guidance.
Tags: high blood pressure, hypertension, blood pressure supplements, DASH diet, ACE inhibitors, ARBs, magnesium, potassium, CoQ10, cardiovascular health, heart health, natural blood pressure remedies, blood pressure medications, lifestyle modifications, blood pressure management