Plant Sterols: Complete Evidence-Based Guide to Cholesterol Management
Plant sterols, scientifically known as phytosterols, constitute a diverse family of naturally occurring compounds that fundamentally challenge cholesterol absorption in the human digestive system. Moreover, these remarkable substances have evolved alongside human dietary patterns for millennia, yet contemporary Western diets provide dramatically reduced phytosterol exposure compared to ancestral nutritional patterns. Consequently, understanding plant sterols becomes crucial for individuals seeking evidence-based approaches to cardiovascular health optimization.
The significance of plant sterols extends far beyond simple cholesterol management, encompassing complex biochemical interactions that influence multiple aspects of lipid metabolism. Furthermore, Cleveland Clinic recognizes that phytosterols are natural compounds found in plants that can help safely lower cholesterol levels to avoid cardiovascular risks. Additionally, understanding plant sterols becomes essential within comprehensive high cholesterol management strategies, while the rigorous scientific foundation supporting plant sterol efficacy has earned recognition from major regulatory agencies, including comprehensive FDA approval for specific health claims.
Understanding Plant Sterols and Stanols Structure
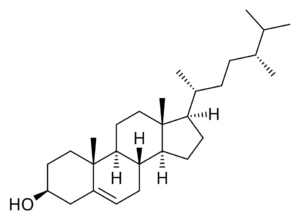
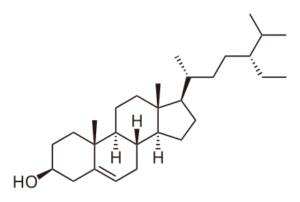
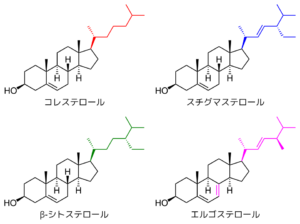
Chemically, plant sterols share remarkable structural similarity to cholesterol, differing primarily in side chain modifications that dramatically alter their biological behavior. Specifically, these molecular differences enable plant sterols to compete directly with cholesterol for absorption while remaining largely unabsorbed themselves. Meanwhile, plant stanols represent hydrogenated derivatives of sterols, characterized by enhanced stability and slightly different absorption characteristics.
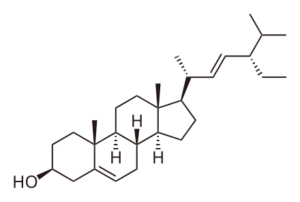
Research has identified more than 250 distinct plant sterol varieties, though the most clinically relevant include beta-sitosterol, campesterol, stigmasterol, beta-sitostanol, and campestanol. Furthermore, scientific investigations demonstrate that absorption rates vary significantly among different plant sterol types, with stanols showing consistently lower absorption than their sterol counterparts. Consequently, understanding these molecular distinctions becomes essential for optimizing therapeutic protocols.
Mechanism of Cholesterol Reduction
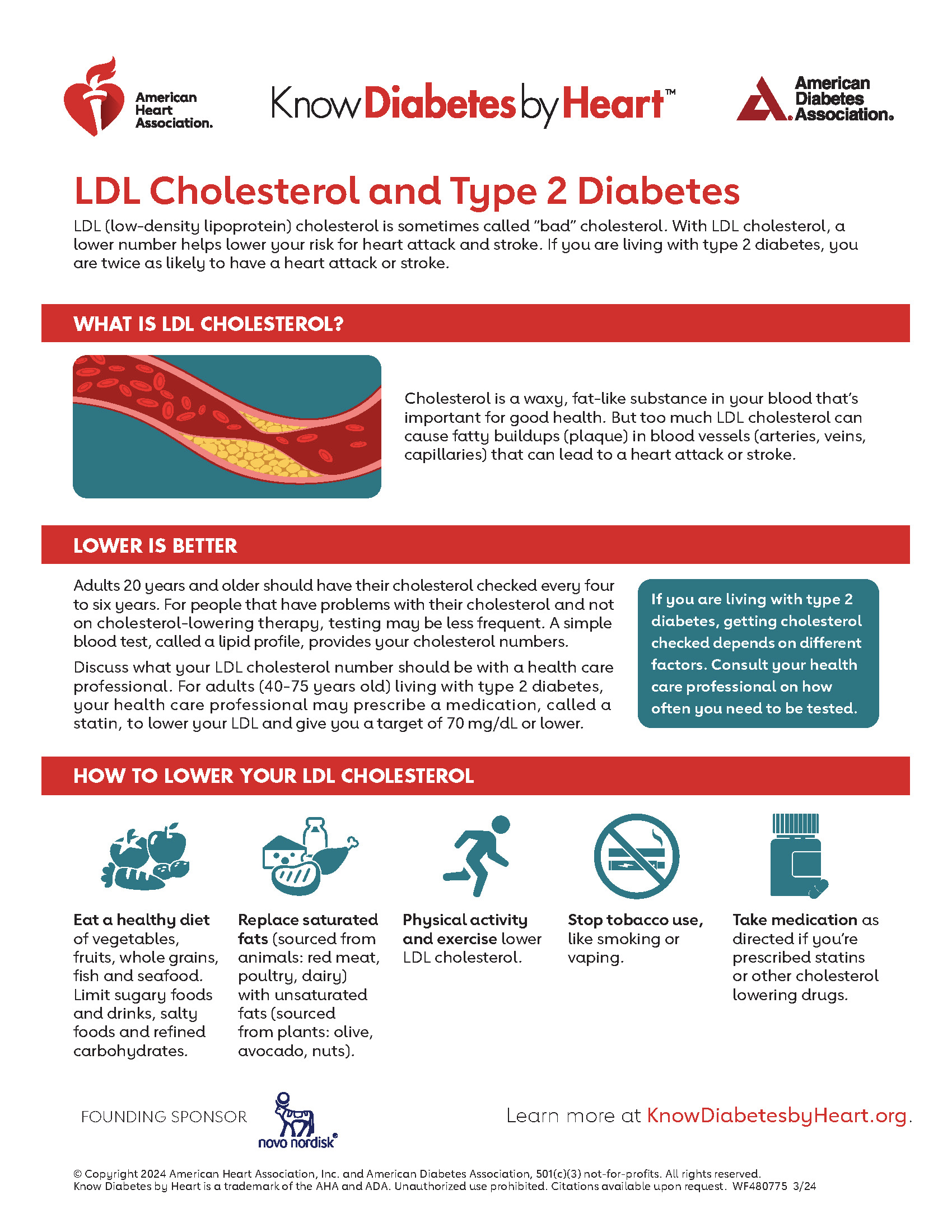
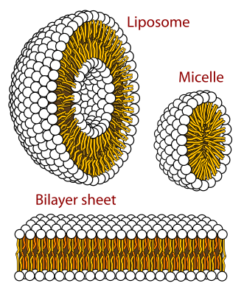
The cholesterol-lowering mechanism of plant sterols operates through sophisticated competitive inhibition at the intestinal level. Initially, plant sterols displace cholesterol from mixed micelles, the molecular vehicles responsible for cholesterol absorption in the small intestine. Subsequently, this displacement forces cholesterol elimination through fecal excretion rather than systemic absorption.
⏳ Plant Sterol Mechanism Timeline:
Advanced research reveals that ATP-binding cassette transporters ABCG5 and ABCG8 play critical roles in plant sterol elimination, explaining why these compounds remain largely unabsorbed despite structural similarity to cholesterol. Moreover, genetic studies demonstrate that individuals with ABCG5/G8 mutations develop sitosterolemia, characterized by dangerous plant sterol accumulation. Therefore, understanding these transport mechanisms illuminates both therapeutic potential and safety considerations for plant sterol supplementation.
Clinical Evidence and Efficacy Data
Extensive clinical research spanning decades consistently demonstrates plant sterol effectiveness for cholesterol reduction across diverse populations. Specifically, meta-analyses incorporating hundreds of studies reveal remarkably consistent results, with optimal dosing protocols achieving meaningful LDL cholesterol reductions. Furthermore, the quality of evidence supporting plant sterols exceeds that available for most dietary supplements, establishing them as evidence-based therapeutic interventions.
| Study Type | Participants | Daily Dose | LDL Reduction | Duration |
|---|---|---|---|---|
| Meta-analysis (Ras et al.) | 6,900+ | 2.1g average | 8-12% | 3-52 weeks |
| Mayo Clinic Review | 4,200+ | 2.0g | 10% | 4-12 weeks |
| DESCO Trial | 116 | 2.5g | 9.2% | 6 weeks |
| Cleveland Clinic | 190 | 1.3g | No significant effect | 28 days |
However, recent high-quality trials present conflicting results that challenge traditional assumptions about plant sterol efficacy. Notably, a 2023 single-center randomized trial involving 190 participants found that plant sterols showed no significant LDL cholesterol decrease compared to placebo. Nevertheless, this contradicts decades of positive research, highlighting the complexity of individual responses and the importance of proper formulation and dosing protocols.
FDA Approval and Regulatory Status
Plant sterols hold the distinction of being among the few dietary supplements with explicit FDA approval for cardiovascular health claims. Specifically, the FDA authorized health claims for plant sterol/stanol esters and reduced risk of coronary heart disease based on significant scientific agreement among qualified experts. Moreover, this approval process required extensive documentation of safety and efficacy data, distinguishing plant sterols from less regulated supplement categories.
“The scientific evidence establishes that including plant sterol/stanol esters in the diet helps to lower blood total and LDL cholesterol levels.”
The FDA’s regulatory framework specifies precise requirements for plant sterol health claims, including minimum dosing thresholds and consumption protocols. Additionally, federal regulations require that plant sterol products contain at least 0.65g per serving for sterols or 1.7g per serving for stanols to qualify for cardiovascular health claims. Furthermore, approved products must meet specific purity standards and consumption guidelines to ensure optimal effectiveness and safety.
Plant Sterols Supplement Formulations
Contemporary plant sterols supplement development incorporates sophisticated formulation strategies designed to maximize bioavailability and cholesterol-lowering efficacy. Initially, early supplement forms often failed to achieve therapeutic benefits due to poor solubilization and inadequate absorption enhancement. However, modern formulations address these limitations through advanced delivery systems and optimal carrier matrices.
Effective plant sterols supplement formulations typically incorporate lecithin complexes, specialized emulsifiers, or esterified forms to enhance solubility and absorption. Moreover, timing and meal consumption patterns significantly influence supplement effectiveness, with optimal protocols requiring consumption during meals containing dietary fat. Consequently, Mayo Clinic research demonstrates that plant sterol supplements work best when taken twice daily with meals to maximize cholesterol displacement effects.
Optimal Dosing Protocols and Administration
Determining optimal plant sterols dosing requires careful consideration of individual factors, baseline cholesterol levels, and concurrent interventions. Generally, research supports daily intakes between 1.5-3.0 grams for meaningful cholesterol reduction, with higher doses providing diminishing returns due to saturation effects. Furthermore, dividing total daily intake across multiple meals enhances effectiveness compared to single-dose administration.
✅ Optimal Plant Sterol Administration Protocol:
- Consume 0.8-1.5g plant sterols with breakfast and dinner
- Take supplements during meals containing at least 10g dietary fat
- Maintain consistent daily timing for maximum effectiveness
- Allow 4-6 weeks for full cholesterol-lowering effects to develop
- Monitor cholesterol levels every 8-12 weeks during initial treatment
- Consider combination with other evidence-based interventions
Research reveals that meal composition significantly influences plant sterol effectiveness, with fat-containing meals providing optimal conditions for cholesterol displacement. Additionally, clinical studies demonstrate that consuming plant sterols with main meals produces superior LDL reduction compared to between-meal administration. Therefore, strategic timing and dietary coordination become essential elements of successful plant sterol protocols.
Food Sources vs. Supplement Considerations
Natural plant sterol sources include vegetable oils, nuts, seeds, whole grains, and legumes, though achieving therapeutic doses through whole foods requires substantial dietary modifications. Specifically, typical Western diets provide only 150-450mg daily of naturally occurring phytosterols, far below the 2-3 gram therapeutic threshold. Conversely, vegetarian diets, particularly vegan approaches, naturally provide higher phytosterol intakes through diverse plant food consumption.
Natural Food Sources:
- Unrefined vegetable oils (highest concentration)
- Nuts and seeds (moderate levels)
- Whole grains and legumes
- Fruits and vegetables (lower levels)
Fortified Food Options:
- Plant sterol-enriched margarines
- Fortified orange juice products
- Enhanced yogurt formulations
- Specialized functional foods
Fortified foods represent a middle ground between natural sources and concentrated supplements, offering enhanced convenience while maintaining food matrix benefits. Moreover, research suggests that foods containing added plant stanols or sterols may be more effective than isolated supplements due to improved bioavailability and consumption patterns. Nevertheless, achieving consistent therapeutic dosing often requires supplemental approaches for optimal cardiovascular benefits.
Safety Profile and Contraindications
Plant sterols demonstrate excellent safety profiles for most healthy individuals, with minimal adverse effects reported across extensive clinical trials. Typically, the most common side effects include mild gastrointestinal symptoms such as loose stools or minor digestive discomfort, particularly during initial supplementation periods. However, certain populations require special consideration due to genetic predispositions or medical conditions that may contraindicate plant sterol use.
Research indicates that plant sterols may reduce absorption of fat-soluble vitamins and carotenoids, though clinical significance remains debated among experts. Specifically, studies demonstrate that plant sterols can diminish fat-soluble vitamins, particularly in women, suggesting potential need for nutritional monitoring during long-term supplementation. Furthermore, pregnant and lactating women should exercise caution with plant sterol supplements due to limited safety data in these populations.
Interaction with Medications and Other Supplements
Plant sterols generally demonstrate minimal drug interactions, making them compatible with most cardiovascular medications and other therapeutic interventions. Importantly, research suggests that plant sterols may enhance the effectiveness of statin medications rather than interfering with their action. Moreover, combination approaches utilizing both pharmaceutical and nutraceutical interventions often produce synergistic cholesterol-lowering effects exceeding either intervention alone.
Studies reveal that combining plant sterols with established cholesterol-lowering medications can provide additive benefits without increasing adverse event rates. Additionally, clinical evidence shows that adding sterols or stanols to statin medication is more effective than doubling the statin dose for achieving target cholesterol levels. Therefore, plant sterols represent valuable adjunctive therapies for individuals requiring intensive cholesterol management.
Individual Response Variability
Clinical experience reveals substantial individual variability in plant sterol responses, with some individuals achieving dramatic cholesterol reductions while others demonstrate minimal benefits. Genetic factors, baseline cholesterol levels, dietary patterns, and gut microbiome composition all influence treatment outcomes. Furthermore, controlled clinical trials show LDL-cholesterol response variability ranging from -33% to +38% among participants receiving identical plant sterol interventions.
“The response variability can be caused by the food matrix and some other food-intake factors, but other metabolic-related and nutrigenomic factors may also determine plant sterol absorption and cardioprotective efficiency.”
Understanding response variability becomes crucial for setting realistic expectations and optimizing treatment protocols for individual patients. Moreover, factors such as age, gender, baseline cholesterol absorption efficiency, and genetic polymorphisms in sterol transport proteins all contribute to therapeutic outcomes. Consequently, monitoring cholesterol levels during initial treatment periods helps identify responders and guides dosing adjustments or alternative interventions when necessary.
Comparison with Other Cholesterol-Lowering Interventions
When evaluated against other natural cholesterol-lowering approaches, plant sterols consistently demonstrate superior efficacy and scientific validation. Specifically, plant sterols achieve more significant LDL reductions than most dietary supplements while maintaining excellent safety profiles. However, pharmaceutical interventions typically produce more dramatic cholesterol changes than any nutraceutical approach, including plant sterols.
| Intervention | LDL Reduction | Evidence Quality | FDA Status |
|---|---|---|---|
| Plant Sterols (2g) | 8-12% | Strong | Approved Health Claim |
| Statin (Low-dose) | 25-40% | Very Strong | FDA Approved Drug |
| Psyllium Fiber | 5-10% | Moderate | Health Claim |
| Red Yeast Rice | 15-25% | Limited* | Unregulated |
Cost-effectiveness analyses reveal that plant sterols occupy a unique position in cholesterol management, providing meaningful benefits at moderate expense compared to pharmaceutical alternatives. Additionally, the favorable safety profile and lack of prescription requirements make plant sterols accessible first-line interventions for individuals with mild to moderate cholesterol elevation. Nevertheless, recent research confirms that statins remain more effective than plant sterols for cardiovascular risk reduction in high-risk populations requiring intensive intervention.
Quality Control and Product Selection
The plant sterols supplement market encompasses significant quality variations, making informed product selection crucial for achieving therapeutic outcomes. Manufacturing processes, raw material sources, formulation approaches, and quality control standards all influence final product effectiveness. Furthermore, third-party testing and certification programs provide valuable quality assurance for consumers navigating complex supplement markets.
✅ Plant Sterols Product Quality Criteria:
- Third-party testing for purity and potency verification
- Clear labeling of sterol/stanol content per serving
- Appropriate formulation with absorption enhancers
- GMP (Good Manufacturing Practice) certification
- Expiration dating and stability testing documentation
- Transparency regarding raw material sources and processing
Regulatory oversight for plant sterol supplements remains limited compared to pharmaceutical products, placing greater responsibility on consumers to evaluate product quality independently. Moreover, price variations often reflect differences in manufacturing quality, formulation sophistication, and testing standards rather than simple market competition. Therefore, investing in higher-quality products may provide superior therapeutic outcomes despite increased initial costs.
Future Research Directions
Emerging research explores novel plant sterol applications beyond traditional cholesterol management, including anti-inflammatory effects, cancer prevention potential, and metabolic syndrome interventions. Specifically, studies suggest that plant sterols possess anti-cancer, anti-inflammatory, anti-atherogenic, and antioxidant activities that may provide benefits even for individuals without elevated cholesterol. Furthermore, personalized medicine approaches may eventually optimize plant sterol protocols based on individual genetic profiles and metabolic characteristics.
Advanced delivery systems, including organogels, steryl glucosides, and nanotechnology applications, represent promising frontiers for enhancing plant sterol bioavailability and effectiveness. Additionally, research into optimal plant sterol combinations, timing protocols, and synergistic interventions continues expanding therapeutic possibilities. Consequently, future developments may significantly improve both the efficacy and practical applications of plant sterol-based cardiovascular interventions.
Practical Implementation Strategies
Successfully implementing plant sterol protocols requires careful attention to dietary patterns, lifestyle factors, and realistic expectation setting. Initially, individuals should establish baseline cholesterol levels and cardiovascular risk assessment before beginning supplementation. Subsequently, gradual introduction of plant sterols with systematic monitoring helps optimize dosing while minimizing potential side effects.
⏳ Plant Sterol Implementation Timeline:
Long-term success with plant sterol supplementation often requires integration with comprehensive lifestyle modifications, including dietary optimization, regular physical activity, and stress management. Moreover, combining plant sterols with other evidence-based interventions frequently produces superior outcomes compared to single-intervention approaches. Therefore, viewing plant sterols as one component of comprehensive cardiovascular risk reduction strategies optimizes both short-term cholesterol improvements and long-term health outcomes.
Cost-Benefit Analysis
Economic evaluations of plant sterol supplementation reveal favorable cost-effectiveness ratios for cardiovascular risk reduction, particularly in intermediate-risk populations. Typically, high-quality plant sterol supplements cost between $20-50 monthly, representing modest expenses compared to prescription medications or advanced medical interventions. Furthermore, preventing cardiovascular events through proactive cholesterol management provides substantial long-term economic benefits beyond immediate supplement costs.
Insurance coverage for plant sterol supplements remains limited, requiring most individuals to bear costs directly. However, flexible spending accounts and health savings accounts often cover qualified plant sterol products when prescribed by healthcare providers. Additionally, considering the potential for reduced future medical expenses through cardiovascular risk reduction, plant sterol supplementation may provide positive long-term return on investment for health-conscious individuals.
Clinical Decision-Making Guidelines
Healthcare providers increasingly recognize plant sterols as valuable tools in comprehensive cardiovascular risk management strategies. Typically, plant sterols serve as appropriate first-line interventions for individuals with mild to moderate cholesterol elevation who prefer natural approaches or experience statin intolerance. Moreover, plant sterols complement lifestyle modifications and may delay or reduce the need for pharmaceutical interventions in appropriate candidates.
Clinical decision-making regarding plant sterol supplementation should incorporate individual risk factors, treatment goals, medication history, and patient preferences. Furthermore, regular monitoring and outcome assessment help optimize treatment protocols and identify individuals who may benefit from alternative or combination approaches. Consequently, collaborative decision-making between patients and healthcare providers typically produces the most effective and sustainable cholesterol management strategies.
References
- Plant Sterols and Plant Stanols in Cholesterol Management and Cardiovascular Prevention. Nutrients. 2023.
- Cleveland Clinic. Plant Sterols: How They Help Manage Cholesterol. 2025.
- Mayo Clinic Proceedings. Efficacy and Safety of Plant Stanols and Sterols in the Management of Blood Cholesterol Levels. 2003.
- National Center for Complementary and Integrative Health. High Cholesterol and Natural Products: What the Science Says.
- LDL-Cholesterol Lowering of Plant Sterols and Stanols—Which Factors Influence Their Efficacy? Nutrients. 2018.
- FDA Code of Federal Regulations. Health claims: plant sterol/stanol esters and risk of coronary heart disease.
- Linus Pauling Institute, Oregon State University. Phytosterols. 2014.
- Plant sterols: factors affecting their efficacy and safety as functional food ingredients. Lipids Health Dis. 2004.
- Diversity of Plant Sterols Metabolism: The Impact on Human Health, Sport, and Accumulation of Contaminating Sterols. Nutrients. 2021.
- Plant Sterols and Stanols: Their Role in Health and Disease. Curr Atheroscler Rep. 2008.
Related Articles
Author Bio
The Remedy Verified Team translates complex metabolic science into clear, practical strategies for everyday health. About the Author
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider before starting any supplement regimen, especially if you have existing medical conditions or take medications. Plant sterols may interact with certain medications and are not appropriate for individuals with sitosterolemia or other genetic sterol metabolism disorders.