The Hidden Hypoglycemia Crisis: Why Your Energy Crashes May Signal Serious Health Issues
Jessica thought her daily 3 PM energy crash was just part of being a busy working mom. The shakiness, brain fog, and sudden irritability that hit like clockwork every afternoon seemed normal in her hectic life. It wasn’t until she collapsed during her daughter’s soccer practice that she discovered the truth: she was experiencing severe reactive hypoglycemia that had been silently damaging her metabolism for years.
Jessica’s story isn’t unique. Cleveland Clinic research reveals that up to 25% of adults experience some form of hypoglycemia, yet most dismiss their symptoms as stress, fatigue, or just “getting older.” The reality? These energy crashes often signal underlying metabolic dysfunction that can progress to serious health complications if left unaddressed.
What Exactly Is Hypoglycemia? (It’s Not What You Think)
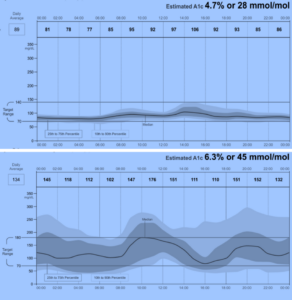
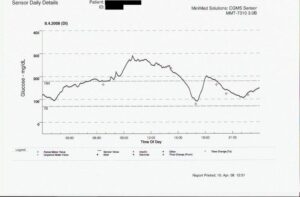
Most people think hypoglycemia only affects diabetics taking too much insulin. That’s completely wrong. NIH research shows that hypoglycemia occurs when blood glucose drops below 70 mg/dL in diabetics or 55 mg/dL in non-diabetics, but symptoms can start appearing at much higher levels—especially if your blood sugar drops rapidly.
Here’s what makes hypoglycemia so tricky: your brain consumes about 20% of your daily glucose despite being only 2% of your body weight. Unlike your muscles, which can burn fat for energy, your brain is almost entirely dependent on glucose. When levels drop, your brain literally starts malfunctioning—affecting everything from your mood to your ability to think clearly.
What You Feel
Early Signs:
- Sudden fatigue
- Difficulty concentrating
- Irritability or mood swings
- Feeling “hangry”
What’s Really Happening
Your Body’s Response:
- Emergency adrenaline release
- Stress hormone activation
- Brain glucose starvation
- Metabolic alarm system triggered
“Hypoglycemia symptoms are your body’s fire alarm—they seem dramatic, but they’re trying to save your life by forcing you to eat.”
The Three Hidden Types of Hypoglycemia Nobody Talks About
Here’s where it gets interesting. There are actually three distinct types of hypoglycemia that affect people differently, and most doctors don’t explain the differences. Understanding which type you have is crucial for effective treatment.
🕐 Reactive Hypoglycemia
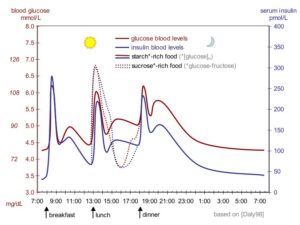
What it is: Blood sugar crashes 2-4 hours after eating, especially after high-carb meals.
Why it happens: Your pancreas overreacts to food, producing too much insulin.
Common triggers: White bread, pasta, sugary drinks, processed foods.
🌙 Fasting Hypoglycemia
What it is: Low blood sugar when you haven’t eaten for 8+ hours, often worst in the morning.
Why it happens: Your liver can’t maintain glucose production overnight.
Warning signs: Morning headaches, night sweats, waking up exhausted.
Why Reactive Hypoglycemia Is Your Body’s Cry for Help
Let me tell you about Marcus, a 41-year-old software engineer who came to understand reactive hypoglycemia the hard way. Every day at 2 PM, after his usual lunch of a sandwich and chips, he’d hit a wall. Brain fog so thick he couldn’t code. Energy so low he’d consider calling in sick. Sound familiar?
Advanced research published in PMC reveals that reactive hypoglycemia often signals the earliest stage of insulin resistance—your body’s warning that you’re on the path to prediabetes and type 2 diabetes. Here’s the scary part: it can happen for years before standard blood tests show any problems.
| Time After Eating | What’s Happening | How You Feel | Significance |
|---|---|---|---|
| 30-60 minutes | Normal glucose rise | Satisfied, energized | Healthy response |
| 2-3 hours | Insulin overshoots | Tired, unfocused | Early insulin resistance |
| 4-5 hours | Severe glucose drop | Shaky, irritable, desperate for food | High diabetes risk |
The Dangerous Symptoms Everyone Ignores
Here’s the problem: hypoglycemia symptoms are sneaky. They mimic other conditions so perfectly that most people spend years treating the wrong thing. Mayo Clinic data shows the average person experiences symptoms for 3-7 years before getting properly diagnosed.
The Progressive Symptom Pattern Most People Miss
Hypoglycemia symptoms follow a predictable pattern, but most people only recognize the obvious late-stage signs. Here’s what really happens, step by step:
Click to Expand: The Complete Hypoglycemia Symptom Timeline
- Stage 1 (Mild, 60-70 mg/dL): Subtle hunger, mild fatigue, slight difficulty concentrating—easily mistaken for normal daily fluctuations
- Stage 2 (Moderate, 50-60 mg/dL): Noticeable shakiness, sweating, rapid heartbeat, anxiety—your fight-or-flight system activates
- Stage 3 (Severe, 40-50 mg/dL): Confusion, slurred speech, mood changes, coordination problems—your brain starts malfunctioning
- Stage 4 (Critical, below 40 mg/dL): Seizures, unconsciousness, potentially life-threatening—requires emergency intervention
Night-Time Hypoglycemia: The Silent Health Destroyer
Sarah had no idea her restless sleep and morning headaches were connected until her doctor suggested checking her blood sugar at 3 AM. The results shocked everyone: 38 mg/dL—dangerously low levels that were occurring every single night without her knowing.
Nocturnal hypoglycemia is particularly dangerous because you can’t recognize the symptoms while sleeping. Research from Mayo Clinic indicates that nighttime episodes can cause:
Signs You Might Be Having Night-Time Blood Sugar Crashes:
- ✓ Waking up with sheets soaked in sweat, even when the room is cool
- ✓ Vivid nightmares or night terrors that wake you up feeling panicked
- ✓ Morning headaches that go away after breakfast
- ✓ Feeling more tired when you wake up than when you went to bed
- ✓ Blood sugar readings that are unusually high first thing in the morning (rebound effect)
What’s Really Causing Your Hypoglycemia? The Hidden Triggers
Most articles tell you hypoglycemia is caused by “not eating enough” or “eating too much sugar.” That’s oversimplified garbage that doesn’t help anyone. The real causes are much more complex and interesting.
Obvious Culprits (What Everyone Knows)
- Skipping meals
- Too much simple sugar
- Excessive alcohol
- Diabetes medications
Hidden Triggers (What Doctors Often Miss)
- Chronic stress disrupting cortisol
- Poor sleep fragmenting glucose control
- Gut inflammation affecting absorption
- Thyroid dysfunction altering metabolism
Let me tell you about the most surprising cause: chronic stress. Research from Medscape shows that people under chronic stress have dysregulated cortisol patterns that can trigger reactive hypoglycemia even with perfect diets. Your body literally can’t maintain stable blood sugar when it’s constantly in fight-or-flight mode.
“I see more hypoglycemia caused by chronic stress and poor sleep than by actual dietary problems. Fix the stress, and the blood sugar often stabilizes on its own.”
The Medication Connection Nobody Talks About
Here’s something that will blow your mind: dozens of common medications can trigger hypoglycemia, and most people (including doctors) don’t make the connection. We’re talking about medications millions of people take daily.
The scary part? These medications don’t just cause hypoglycemia—they can also mask the symptoms. Beta-blockers, for example, prevent the rapid heartbeat and shakiness that usually warn you of low blood sugar, so you might progress to severe hypoglycemia without any warning signs.
How to Fix Hypoglycemia: Beyond the Obvious Solutions
Forget everything you’ve heard about just “eating more protein” or “avoiding sugar.” While those help, they’re band-aids on a bigger problem. Real hypoglycemia management requires understanding your individual patterns and triggers.
The Personalized Approach That Actually Works
Remember Jessica from the beginning? Here’s how she finally solved her hypoglycemia crisis. Instead of generic dietary advice, she used a targeted approach based on her specific symptoms and triggers:
What She Used to Do
- Skip breakfast due to morning rush
- Large lunch with refined carbs
- Crash at 3 PM, grab coffee and cookies
- Large dinner to “make up” for poor day
- Late-night snacking when couldn’t sleep
Her New Strategy
- Protein-fat breakfast within 1 hour of waking
- Smaller lunch with complex carbs and fiber
- Planned snack at 2:30 PM before crash time
- Moderate dinner 3 hours before bed
- Magnesium supplement for better sleep

The Emergency Protocol Every Adult Should Know
When hypoglycemia hits hard, you need to act fast. The Endocrine Society’s protocol is more sophisticated than the basic “15-15 rule” most people know:
| Severity Level | Symptoms | Immediate Action | Follow-up |
|---|---|---|---|
| Mild | Hunger, slight shaking | 15g fast carbs | Recheck in 15 min |
| Moderate | Sweating, rapid heartbeat | 20g fast carbs + protein | Monitor for 30 min |
| Severe | Confusion, coordination problems | Glucagon injection if available | Seek medical attention |
| Critical | Unconscious, seizures | Call 911 immediately | Emergency room care |
Advanced Strategies: What the Experts Do Differently
Once you’ve mastered the basics, there are advanced strategies that can take your blood sugar stability to the next level. These are techniques that endocrinologists use with their most challenging patients.
Circadian Glucose Optimization
Your body’s glucose needs change dramatically throughout the day based on natural hormone cycles. Recent research reveals that insulin sensitivity is highest in the morning and lowest in the evening—which means meal timing matters more than meal content.
The Advanced Timing Protocol
6-8 AM: Largest meal with moderate carbs (your body handles them best now)
12-2 PM: Moderate meal with balanced macros
6-7 PM: Smallest meal, mostly protein and vegetables
After 8 PM: Nothing but water and herbal tea
The Stress-Glucose Connection
Here’s something most doctors miss: chronic stress can cause hypoglycemia even with perfect eating habits. When cortisol patterns get disrupted, your body loses the ability to maintain steady glucose between meals.
Stress-Related Hypoglycemia Management:
- ✓ Morning sunlight exposure within 30 minutes of waking to regulate cortisol rhythms
- ✓ Deep breathing exercises during traditional “crash times” to activate parasympathetic recovery
- ✓ Magnesium glycinate supplementation to support stress resilience and glucose regulation
- ✓ Regular sleep and wake times to maintain circadian glucose control
When Hypoglycemia Means Something More Serious
Most hypoglycemia is manageable with lifestyle changes, but sometimes it’s a warning sign of serious underlying conditions that require immediate medical attention. Don’t ignore these red flags.
Research from NCBI indicates that recurrent unexplained hypoglycemia can signal rare but serious conditions like insulinomas (insulin-producing tumors), adrenal insufficiency, or liver disease. These conditions require specialized testing and treatment that goes far beyond dietary management.
The Diabetes Connection Everyone Should Understand
Here’s the plot twist: reactive hypoglycemia often appears years before someone develops type 2 diabetes. It’s like your body’s early warning system malfunctioning. WebMD research shows that people with late-stage reactive hypoglycemia have a 60-70% increased risk of developing diabetes within 10 years.
The good news? Catching it at the hypoglycemia stage means you can potentially prevent diabetes entirely through targeted interventions. This is where the connection to comprehensive approaches like The Ultimate Guide to Natural Diabetes Support becomes crucial—addressing hypoglycemia often requires the same metabolic optimization strategies used for diabetes prevention and management.
“Hypoglycemia and diabetes aren’t opposite conditions—they’re different points on the same spectrum of metabolic dysfunction.”
Your Action Plan: What to Do Starting Tomorrow
Knowledge without action is useless. Here’s your step-by-step plan for taking control of hypoglycemia, starting with the highest-impact changes first.
Week 1-2: Foundation
Priority Actions:
- Track symptoms and timing for patterns
- Never skip breakfast—protein + fat essential
- Eat every 3-4 hours during waking hours
- Carry emergency glucose tablets
Week 3-4: Optimization
Advanced Strategies:
- Time largest meal for morning hours
- Add stress management techniques
- Consider targeted supplementation
- Evaluate medication effects with doctor
Remember Jessica? Six months after implementing these strategies, she’s not the same person. Stable energy, clear thinking, and—most importantly—confidence that her body is working with her instead of against her. That same transformation is possible for you.
References
- Cleveland Clinic. Hypoglycemia (Low Blood Sugar): Symptoms & Treatment. Cleveland Clinic Medical Professional. 2017.
- Mathew P, Thoppil D. Hypoglycemia. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. PMID: 30252231.
- Mayo Clinic. Hypoglycemia – Symptoms and causes. Mayo Foundation for Medical Education and Research. 2023.
- Tuzcu A, Bahceci M, Gokalp D, et al. Postprandial Reactive Hypoglycemia. PMC. 2017;8:e000143.
- Mayo Clinic. Diabetic hypoglycemia – Symptoms & causes. Mayo Foundation for Medical Education and Research. 2025.
- Healthline. Hypoglycemia Without Diabetes: What Does It Mean? Healthline Media. 2024.
- Endocrine Society. Hypoglycemia Patient Guide. Endocrine Society Patient Engagement. 2022.
- Agiostratidou G, Anhalt H, Ball D, et al. Hypoglycemia in diabetes: An update on pathophysiology, treatment, and prevention. PMC. 2017;8:e000143.
- Cryer PE, Axelrod L, Grossman AB, et al. Non-Diabetic Hypoglycemia. StatPearls [Internet]. 2023.
- WebMD. Reactive Hypoglycemia, What Is It? Symptoms, Causes, Treatment. WebMD Medical Reference. 2024.
Medical Disclaimer
The information provided in this article is for educational purposes only and should not be considered as medical advice. Always consult with a qualified healthcare professional before making any changes to your health management plan. Hypoglycemia can be a serious medical condition that requires proper diagnosis and treatment. Individual results may vary, and what works for one person may not be appropriate for another. If you experience symptoms of hypoglycemia, especially severe episodes involving loss of consciousness or seizures, seek immediate medical attention. This content is not intended to diagnose, treat, cure, or prevent any disease.