Chromium for Diabetes Support: Evidence, Dosage, Safety & Practical Use
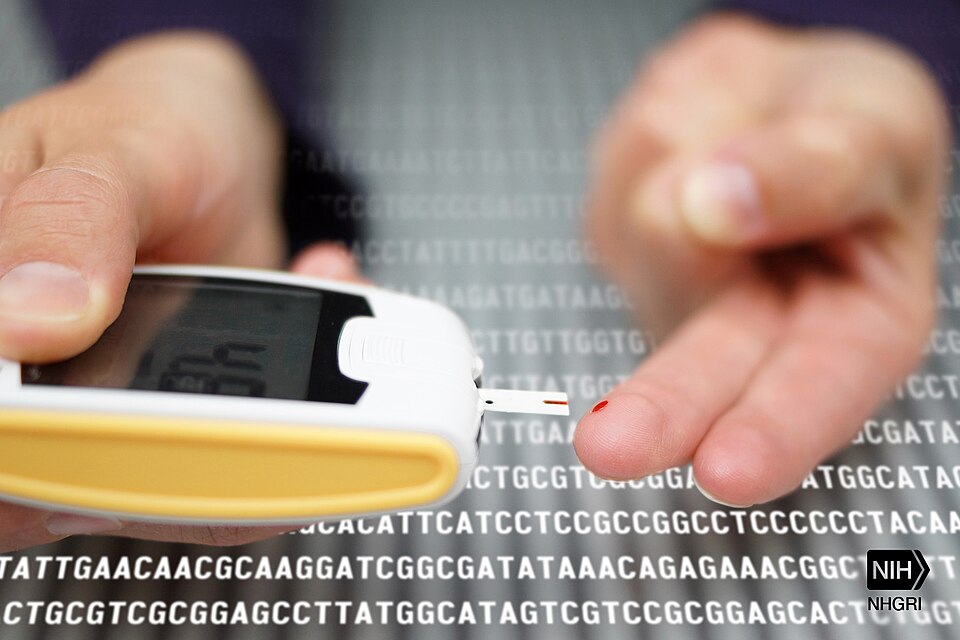
How Chromium Might Support Glycemia
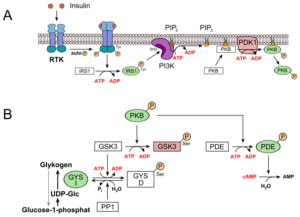
Chromium is proposed to influence insulin receptor activity and downstream signaling, potentially improving cellular glucose uptake when conditions are right. Think of insulin as a key and the receptor as a lock; chromium may help the lock turn more smoothly. That is a plausible mechanism, not a guarantee of benefit. Human outcomes depend on the form used, dose, baseline diet, medication context, study duration, and individual biology—hence the variability you see in clinical findings.
What the Evidence Says

The clinical literature on chromium for diabetes support is mixed. Meta-analyses and trials land on both sides—some reporting small improvements in fasting glucose or A1C, others finding no advantage over placebo. The heterogeneity is hard to ignore: differing forms and doses, diverse populations, and variable study designs make apples-to-apples comparisons difficult.
- Signals of benefit: A 2020 meta-analysis found chromium supplementation could improve several glycemic indices in type 2 diabetes, although effect sizes varied and clinical significance remains debated. See: Asbaghi 2020 (PubMed) and ScienceDirect.
- Neutral findings: Multiple randomized trials—particularly in Western cohorts—reported no meaningful changes in insulin sensitivity or A1C despite generous intakes; for example, Diabetes Care 2005 and Diabetes Care 2006.
- Guideline perspective: The American Diabetes Association does not recommend supplements (including chromium) to lower glucose for routine management due to insufficient consistent efficacy.
Bottom line: Chromium may be worth a cautious, time-boxed trial for select individuals under clinician guidance, with clear metrics, and a willingness to discontinue if no benefit appears. It is not a substitute for indicated medications or lifestyle foundations.
Who Might Consider Chromium?
- Type 2 diabetes patients exploring adjuncts: If your clinician agrees, run a short, monitored trial with a defined goal (e.g., fasting average, % in range, post-meal peak), then keep or drop based on objective results rather than hopes.
- People with low dietary variety: Diets heavy in ultra-processed foods can miss trace minerals; address diet first. If a supplement trial still makes sense, set dates, metrics, and stop criteria in advance.
- Users balancing cost and risk: Supplements cost time and money and can interact with meds. Use conservative doses, track results, and discontinue if there’s no measurable upside.
Studied Dosage Ranges & Forms
Trials have explored multiple forms and a wide range of intakes. More is not automatically better; quality and monitoring matter more than chasing high numbers on a label.
- Forms: Picolinate (most common in research), nicotinate, and chloride. Bioavailability may differ by form.
- Studied ranges (time-limited): Chromium picolinate appears frequently around ~200–1,000 mcg/day in trials; other forms vary by protocol. Use clinician guidance—especially if you take glucose-lowering medications.
- Dietary context: Adequate Intake (AI) is ~25 mcg/day for adult women and ~35 mcg/day for adult men, reflecting typical intake levels rather than supplement targets. See NIH ODS (consumer).
- Timing & tolerability: Many users take chromium with meals; track fasting and post-meal readings and stop the trial if adverse effects or no benefit appear.
Safety, Interactions & Monitoring
Most adults tolerate typical amounts, but caution is warranted. Because chromium may influence glycemia, combining it with insulin or insulin-secretagogues without coordination can increase hypoglycemia risk. Special populations—pregnancy, kidney or liver disease, adolescents/older adults—should only consider supplements with clinician oversight.
- Medication interactions: Coordinate with your care team if you use insulin or sulfonylureas; introduce one change at a time and verify with meter/CGM data.
- Set stop criteria: Decide in advance when to discontinue (e.g., adverse effects, no objective improvement, conflicting priorities) to prevent indefinite use.
- Share outcomes: Document brand, form, lot, dose, and trends; review results with your clinician and keep only what helps.
Food Sources of Chromium

Chromium content varies with soil and processing, but commonly cited contributors include whole grains, broccoli and other
vegetables, legumes, nuts and seeds, lean meats, and seafood. A minimally processed dietary pattern remains the foundation; supplements are supplementary. See the NIH ODS professional fact sheet for an overview.
Choosing a Quality Chromium Supplement
- Third-party testing: Prefer USP/NSF or brands that publish batch-level testing; independent verification reduces risks of contaminants or label inaccuracy.
- Transparent label: Demand the elemental chromium amount per serving and the exact form; avoid ambiguous complexes.
- Clean excipients: Fewer unnecessary additives reduce exposure to potential allergens or GI irritants; choose capsules or tablets based on personal tolerability.
- Data discipline: Track dose and readings; keep what helps and discontinue what doesn’t—then reallocate effort to pillars like diet quality and activity.
How to Discuss Chromium With Your Clinician (Step-by-Step)

“Chromium trials should be supervised and guided by objective data with a healthcare provider.” Bring data: Recent A1C, fasting/post-meal logs, current meds/supplements, and relevant symptoms—objective context speeds decisions.
- Define a trial: Agree on form/dose and a 4–8-week window with specific metrics (fasting average, % in range, post-meal peak).
- Set stop criteria: Write down when to discontinue—adverse effects or no measurable benefit—so the plan doesn’t drift.
- Review outcomes: Reassess with your clinician and either keep, adjust, or drop based on measured results—not marketing claims.
Myth vs Fact: Chromium & Diabetes
| Myth | Fact |
|---|---|
| “Chromium cures diabetes.” | No supplement cures diabetes. At best, chromium is an adjunct within a comprehensive, clinician-guided plan anchored by lifestyle and indicated medications. See ADA guidance. |
| “Higher doses guarantee better results.” | Trials span wide ranges with inconsistent outcomes; pushing dose raises risk without ensuring benefit. Use conservative, time-boxed trials with monitoring (e.g., Diabetes Care 2005). |
| “All chromium forms act the same.” | Forms differ (picolinate, nicotinate, chloride) and may vary in bioavailability; product quality and testing matter more than marketing around forms (see NIH ODS). |
| “Supplements let me relax on diet and movement.” | Foundational habits still drive most glycemic improvement; supplements can’t compensate for missing basics. Pair any trial with nutrition and activity upgrades. |
Pros & Cons at a Glance
- Pros: Biologically plausible mechanism, inexpensive, widely available, and may assist select individuals when monitored within a comprehensive plan.
- Cons: Evidence is inconsistent; potential drug–supplement interactions; brand quality varies; can distract from proven lifestyle levers.
FAQs
Does chromium lower A1C?
Some analyses and trials report small improvements, while others show no effect. Expect variability and rely on a supervised, time-boxed trial with objective monitoring before deciding whether to continue.
Which form is best studied?
Chromium picolinate appears most frequently in research, though other forms exist. Prioritize third-party tested products with transparent labels over marketing language.
Can chromium replace my medication?
No. Current ADA guidance does not support supplements to lower glucose routinely; coordinate changes with your clinician to avoid interactions or hypoglycemia.
How long should a trial last?
A defined 4–8-week window with meter/CGM tracking and pre-agreed stop criteria is common; extend only if data show meaningful benefit and safety is maintained.
References
- NIH Office of Dietary Supplements. Chromium — Health Professional Fact Sheet. U.S. National Institutes of Health; 2022.
- American Diabetes Association. Vitamins & Supplements for Diabetes. ADA; 2024–2025.
- Asbaghi O, et al. Effects of chromium supplementation on glycemic control in type 2 diabetes: Meta-analysis. PubMed (2020); see also ScienceDirect.
- Gunton JE, et al. Chromium supplementation does not improve glucose metabolism in impaired glucose tolerance. Diabetes Care. 2005.
- Josefsson A, et al. Chromium treatment has no effect in Western patients with type 2 diabetes. Diabetes Care. 2006.
- Costello RB, et al. Chromium supplements for glycemic control in type 2 diabetes: Narrative review. Nutrition Reviews (PMC). 2016.
- NIH ODS. Chromium — Consumer Fact Sheet. U.S. National Institutes of Health; 2021.
Author Bio
The Remedy Verified Team is dedicated to exploring natural, research-backed approaches to chronic health conditions. Our writers translate complex scientific studies into clear, practical insights to help readers make informed decisions about their health. also check About the Author
Disclaimer
⚠️ Disclaimer: The information provided in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. Natural remedies, supplements, and lifestyle changes may affect individuals differently. Always consult a qualified healthcare professional before making any changes to your diet, medications, or health routine—especially if you have an existing medical condition, are pregnant, or are taking prescription drugs. Remedy Verified does not provide medical services, and the content shared here should not be considered a substitute for professional medical guidance. Use of this website and its information is at your own risk.