My Ear Won’t Pop: What to Try After Everything Fails
You’ve tried yawning, swallowing, chewing gum, the Valsalva maneuver—even those weird YouTube tricks. Yet your ear still feels clogged, muffled, and maddeningly blocked. That persistent pressure is disrupting your hearing, sleep, and focus.
When standard popping techniques fail, you’re usually dealing with eustachian tube dysfunction rather than simple air pressure. Plugged ears from inflammation need different treatment than altitude-related pressure. This guide gives you a tier-by-tier protocol with specific timelines and clear criteria for when to escalate. Most cases resolve within 1-3 weeks when you address the underlying cause systematically.
Quick Answer: What to Do When Your Ear Won’t Pop
When ears won’t pop despite yawning and swallowing, you’re usually dealing with eustachian tube dysfunction from congestion, allergies, or post-viral inflammation. For clogged ears: try steam inhalation with nasal saline irrigation, then attempt the Toynbee maneuver (pinch nose and swallow). If plugged ears persist beyond 5 days or include pain with hearing loss, consult a healthcare provider.
Start These 4 Steps Today:
- Days 1-2: Steam inhalation (10-15 min, 3x daily) + nasal saline irrigation + drink 8-10 cups water daily + sleep with head elevated 30-45 degrees
- Days 2-3: Add Toynbee maneuver (pinch nose and swallow) after each steam session; avoid forcing Valsalva if there’s no improvement
- Days 3-5: Consider OTC nasal corticosteroid spray (fluticasone) or oral decongestant (pseudoephedrine) if it’s congestion-related
- Day 5+: Schedule medical evaluation if there’s zero improvement or symptoms worsen—bring your timeline of everything you’ve tried
Red Flags Requiring Immediate Care: Severe pain (>6/10), sudden hearing loss, bloody or purulent discharge, dizziness with nausea, or fever above 101°F.
Why Your Clogged Ears Won’t Pop Despite Trying Standard Techniques
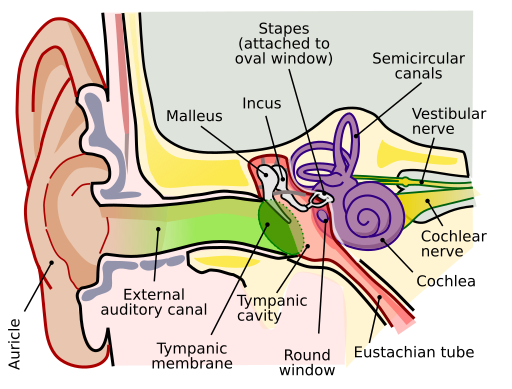
The popping sensation represents your eustachian tube opening to equalize pressure between your middle ear and the outside environment. Simple barotrauma—like pressure changes during a flight—responds well to basic techniques because the tube functions normally.
But when those methods fail repeatedly? The eustachian tube itself is compromised. Think of it as a garden hose connecting your middle ear to your throat. Simple pressure is a kink you can shake out. Eustachian tube dysfunction (ETD) is the hose clogged with debris—no amount of shaking helps because you need to clear the blockage first.
The Congestion-Inflammation Cycle
ETD develops through a self-reinforcing cycle. Initial mucus buildup—from allergies, a cold, or sinus infection—blocks the tube opening. The trapped fluid creates an environment where bacteria multiply, triggering more inflammation. More inflammation produces more mucus, worsening the blockage. This explains why your ear might feel worse days after your cold symptoms improved.
Timeline matters: Acute ETD (under 7 days) usually resolves with conservative measures. Subacute ETD (1-3 weeks) may require medical support like prescription nasal steroids. Chronic ETD (over 3 weeks) warrants ENT evaluation to identify underlying causes—enlarged adenoids, chronic sinusitis, reflux affecting the tube opening, or structural issues.
Post-Viral Persistence
Many people experience stubborn ear blockage 1-2 weeks after respiratory symptoms resolve. The virus is gone, but residual inflammation keeps the eustachian tube swollen. This post-viral ETD can persist 2-3 weeks even without active infection—your ear isn’t getting worse, it’s following a predictable inflammatory resolution curve that takes time.
This differs from a new middle ear infection, which would show worsening pain, fever, and possibly discharge. Post-viral cases benefit from anti-inflammatory approaches like nasal corticosteroids and time, while bacterial infections require antibiotics.
For context on managing inflammation through natural approaches that coordinate with medical care, see our guide to evidence-based natural health strategies.
Step-by-Step Protocol for Blocked Ears That Won’t Clear
Success depends on matching your approach to the underlying cause and escalating systematically. This protocol progresses through four tiers with defined timelines—data-driven troubleshooting rather than indefinite repetition of methods that aren’t helping.
Tier 1: Foundational Home Remedies (Try 24-48 Hours)
Steam Inhalation (Most Important): Boil water, pour into a large bowl, lean over it with a towel over your head. Inhale steam for 10-15 minutes, three times daily. Add 2-3 drops of eucalyptus oil if available. The moist heat thins mucus and reduces eustachian tube inflammation. Best times: morning upon waking, mid-afternoon, and before bed.

Nasal Saline Irrigation: Use a neti pot or squeeze bottle with distilled or previously boiled water (never tap water). Flush each nostril 2-3 times daily. Tilt your head sideways over a sink, insert the spout in your upper nostril, let saline flow through. Blow your nose gently afterward.
Hydration Target: Drink 8-10 cups (64-80 oz) of water daily. Dehydration thickens mucus, making blockage worse. Warm fluids like herbal tea provide additional steam exposure. Your urine should be pale yellow.
Sleep Elevated: Prop your head up 30-45 degrees using a wedge pillow or 2-3 standard pillows. If one ear’s affected, sleep with that ear facing up. Elevation promotes overnight drainage.
Stop Criteria: If pressure hasn’t improved at all after 48 hours of consistent Tier 1 interventions, escalate to Tier 2.
Tier 2: Advanced Techniques (Try 2-3 Days)
Toynbee Maneuver (Safest Option): Pinch your nose closed and swallow. Try with a mouthful of water if easier. Do 3-4 repetitions every few hours. This combines pressure with muscle movement to open stubborn tubes. Stop immediately if you feel sharp pain. The Toynbee’s gentler than the Valsalva and carries lower rupture risk.

Modified Valsalva (Use Caution): Pinch your nose, close your mouth, and gently blow as if trying to fog a mirror—not inflate a balloon. Try 2-3 gentle attempts, then stop if no pop occurs. Never force it. Aggressive Valsalva can rupture your eardrum.
Frenzel Maneuver (For Stubborn Cases): Pinch your nose and make a “K” clicking sound with your tongue against your palate while tensing throat muscles. This technique requires practice but can succeed when others fail.
Combination Timing: Do steam inhalation for 10 minutes, then immediately try Toynbee or modified Valsalva while tissues are warm and mucus is thinned. The combined effect often exceeds either method alone. Log your results to identify your personal pattern.
Stop Criteria: After 2-3 days, if pressure remains unchanged or symptoms worsen, escalate to Tier 3. Continued forceful attempts risk eardrum damage without benefit.
Tier 3: Over-the-Counter Medical Support (3-5 Days)
Oral Decongestants: Pseudoephedrine (Sudafed, not the “PE” version) reduces blood vessel swelling in nasal passages and eustachian tubes. Typical adult dosing: 30-60 mg every 4-6 hours, not exceeding 240 mg daily. Works within 30 minutes if it’s going to help. Cautions: raises blood pressure and heart rate, causes insomnia if taken late, may worsen anxiety. Check with your healthcare provider if you have cardiovascular conditions.
Nasal Corticosteroid Sprays: Fluticasone (Flonase), mometasone (Nasonex), or triamcinolone reduce inflammation over several days. Unlike decongestants, these don’t provide immediate relief but target the underlying inflammatory process. Use 1-2 sprays per nostril daily, aiming toward the outer ear. Peak effectiveness takes 3-7 days of consistent use. Safe for extended use unlike decongestant nasal sprays, which cause rebound congestion after 3 days.
Antihistamines (If Allergy-Related): If your ETD coincides with seasonal allergies or known triggers, try cetirizine (Zyrtec) or loratadine (Claritin). Take consistently rather than as-needed for best results. You should notice improvement within 24-48 hours if allergies drive your symptoms.
Usage Limits: Never use decongestant nasal sprays (Afrin, Neo-Synephrine) for more than 3 consecutive days—they cause severe rebound congestion. Document what you try, at what dose, and for how long.
Stop Criteria: If 5 days of appropriate OTC medication produces zero improvement, or if symptoms worsen despite treatment, schedule medical evaluation. You’ve completed a reasonable trial of self-management.
Tier 4: Medical Evaluation Triggers
Escalate to professional care under any of these conditions:
- Duration: More than 5 days without any improvement despite systematic interventions
- Symptom Progression: Increasing pain, worsening hearing loss, or new symptoms developing
- Functional Impact: Significant hearing impairment affecting daily activities, balance problems, or inability to sleep
- Red Flags: Discharge from the ear, fever >101°F, severe pain >6/10, sudden hearing loss, dizziness with nausea
Bring documentation to your appointment: timeline of symptoms, complete list of interventions tried with durations, any patterns you’ve noticed, and current medications. This data discipline allows your provider to make informed decisions rather than starting from scratch.
For more on systematic health monitoring approaches, see our article on evidence-based supplement trials with defined metrics.
Quick Reference: When to Try Each Approach
- Hours 0-48: Steam 3x/day + saline irrigation + hydration + elevated sleep
- Hours 48-96: Add Toynbee maneuver after steam (don’t force Valsalva)
- Days 3-5: OTC decongestant or nasal steroid spray if needed
- Day 5: Medical evaluation if no improvement
- Immediate care: Severe pain, sudden hearing loss, discharge, or fever
⚠️ Important: This tiered protocol assumes no red-flag symptoms are present. Severe pain, sudden hearing loss, bloody discharge, high fever, or facial weakness require immediate medical attention—do not attempt home remedies in these scenarios.
Targeted Solutions Based on What’s Blocking Your Eustachian Tube
Eustachian tube dysfunction has different root causes that respond to different interventions. Post-viral ETD requires anti-inflammatory strategies. Allergy-driven blockage needs antihistamine management. Altitude-induced pressure responds to mechanical techniques. Accurate cause identification shortens your resolution timeline.
Post-Cold or Sinus Infection ETD
Respiratory infections leave an inflammatory trail even after the virus clears. The eustachian tube lining remains swollen and hypersensitive, producing excess mucus that blocks normal drainage for 1-3 weeks post-infection.
Priority Interventions: Nasal saline irrigation combined with steam inhalation targets residual mucus. Add an oral decongestant (pseudoephedrine) for the first 3-5 days if nasal passages still feel congested. Transition to a nasal corticosteroid spray (fluticasone) by day 3-4 to address ongoing inflammation.
Timeline Expectations: Expect gradual improvement over 7-14 days, not sudden resolution. You might notice fluctuations—better in the afternoon after upright activity, worse in the morning after overnight mucus accumulation. Track the trend across days rather than hour-to-hour changes. Stable or worsening symptoms after 10 days warrant medical evaluation.
Bacterial vs Viral: Know the Difference
Post-viral ETD: Stable symptoms, uncomfortable but not progressive, clear mucus
Bacterial infection: Worsening symptoms after 5-7 days, yellow-green discharge, facial pressure when bending forward, returning fever
Bacterial vs Viral Markers: Post-viral ETD maintains relatively stable symptoms—uncomfortable but not progressive. A bacterial sinus infection complicating your recovery shows: yellow-green nasal discharge (not just clear mucus), facial pain/pressure that worsens when bending forward, symptoms that initially improved then worsened after 5-7 days, or fever returning after being gone. These markers suggest bacterial superinfection requiring antibiotic evaluation.
Allergy-Related Eustachian Tube Dysfunction
Allergic rhinitis causes chronic nasal and eustachian tube inflammation that fluctuates with exposure. Unlike infection-related ETD, allergy-driven blockage often shows seasonal patterns (spring pollen, fall ragweed) or follows specific triggers (dust, pets, mold).
Recognition Pattern: Allergy-related ETD typically involves both ears, accompanies other allergic symptoms (itchy eyes, sneezing, clear nasal drainage), improves temporarily with antihistamines, and worsens during high-pollen counts.
Targeted Approach: Start with a daily second-generation antihistamine (cetirizine, loratadine, or fexofenadine) rather than as-needed dosing. Add a nasal corticosteroid spray for sustained control. Environmental modifications: use HEPA filters, minimize outdoor exposure during peak pollen times, wash bedding in hot water weekly to reduce dust mites, and shower before bed to remove allergens from hair and skin.
Timeline Expectations: Antihistamines provide relief within 24-48 hours if allergies drive your symptoms. Nasal corticosteroids take 3-7 days to reach full effectiveness. If you see no improvement after 5 days of combined therapy, allergies may not be the primary driver—reconsider the diagnosis. Chronic allergy sufferers might need maintenance treatment during their trigger seasons rather than reactive intervention after symptoms develop.
Altitude or Flying-Induced Barotrauma
Airplane descent creates rapid pressure changes that overwhelm the eustachian tube’s normal equalization capacity, especially if you have any baseline congestion. The pressure differential can trap air in the middle ear or create a vacuum effect.
Immediate Response: Try swallowing repeatedly while pinching your nose (Toynbee maneuver). Chew gum vigorously to stimulate frequent swallowing. If those fail within the first few hours, transition to gentle modified Valsalva attempts. Most altitude-related ETD resolves within 12-72 hours as the pressure differential gradually equalizes.
Prevention for Next Flight: Take an oral decongestant (pseudoephedrine) 30-60 minutes before descent if you have any nasal congestion. Use a nasal corticosteroid spray daily for 3 days before flying if you have a history of flight-related ear problems. Stay awake during descent—you swallow less frequently while sleeping, preventing pressure equalization. Consider pressure-regulating earplugs (EarPlanes) that slow the rate of pressure change, giving your eustachian tubes more time to adjust.
Why It Persists After Landing: The eustachian tube may have sustained minor trauma from the pressure differential, causing temporary dysfunction. Or residual negative pressure in the middle ear creates a vacuum effect that prevents the tube from opening normally—it needs to “reset” before normal function returns. Most altitude-related ETD resolves within 12-72 hours as the pressure differential gradually equalizes.
Device Evaluation: EarPlanes show mixed evidence—some travelers report significant benefit, others notice no difference. They’re inexpensive enough to warrant a trial if you fly frequently. The Otovent device (inflating a balloon through your nostril) demonstrates approximately 80% success rates in pediatric studies for eustachian tube dysfunction, though adult data is more variable.
Chronic Eustachian Tube Dysfunction (Symptoms >3 Weeks)
ETD persisting beyond three weeks despite appropriate treatment requires investigation for underlying causes. Common culprits include: enlarged adenoids blocking the tube opening, chronic sinusitis, gastroesophageal reflux irritating the nasopharynx, TMJ dysfunction affecting tube mechanics, or structural abnormalities like a deviated septum.
Lifestyle Factors That Maintain Dysfunction: Low ambient humidity (below 30%) dries nasal and eustachian tube mucosa, impairing function. Chronic dehydration thickens secretions that should drain easily. Sleeping flat promotes mucus accumulation. Smoking or secondhand smoke exposure causes chronic mucosal inflammation. These factors don’t cause ETD initially but prevent resolution once it develops.
GERD Connection: Gastroesophageal reflux affects the upper airway more commonly than many realize. Acid or non-acid reflux irritates tissues around the eustachian tube opening, causing chronic swelling. This connection explains why some people experience worsening ear symptoms after eating, when lying down, or first thing in the morning. If you have heartburn, regurgitation, chronic throat clearing, or persistent hoarseness alongside ETD, discuss reflux evaluation with your provider.
Medical Intervention Thresholds: ENT specialists may recommend balloon dilation—threading a small balloon through the nose to the eustachian tube opening, then inflating it to widen the tube. This procedure shows 60-75% success rates for appropriately selected patients with chronic ETD. Pressure equalization tubes (tympanostomy tubes) drain middle ear fluid when medical management fails. These are last-resort options after exhausting conservative management.
Coordination Strategy: Document your complete treatment history before ENT consultation: everything tried, durations, any response patterns, aggravating or relieving factors, and impact on daily function. This data allows the specialist to bypass treatments you’ve already failed and move toward diagnostic evaluation or procedural interventions.
When Plugged Ears Signal Something More Serious
Most eustachian tube dysfunction is uncomfortable but not dangerous. However, certain symptom patterns indicate complications requiring immediate medical attention.
Dangerous Techniques to Avoid
Forcing the Valsalva Maneuver: Aggressive pressure can rupture a compromised eardrum or worsen existing middle ear damage. If gentle attempts don’t work after 2-3 tries, the tube isn’t ready to open—more force won’t change that.
Q-tips or Objects in Ear Canal: ETD is a middle ear problem behind your eardrum. Nothing you insert into your ear canal reaches the middle ear. Q-tips push wax deeper and can perforate the eardrum.

Ear Candling: Multiple studies demonstrate it doesn’t work—no wax or debris is removed—and it carries real risks including burns, ear canal obstruction, and eardrum perforation. The FDA issued a safety warning advising consumers to avoid ear candling entirely.
Excessive Nose Blowing: Forceful nose blowing can drive infected mucus from your nasal cavity up through the eustachian tube into your middle ear, converting ETD into an acute middle ear infection. Blow gently, one nostril at a time, and stop if you feel pressure building in your ears. If you need to blow frequently, you’re treating symptoms rather than addressing underlying congestion—switch to nasal irrigation or decongestants.
Red Flags Requiring Immediate Medical Attention
Sudden Hearing Loss: Significant hearing reduction developing over hours to days can indicate inner ear problems unrelated to ETD. Sudden sensorineural hearing loss is a medical emergency, and outcomes depend on how quickly treatment begins. Get evaluated within 24-48 hours.

Severe Unrelenting Pain: ETD typically causes pressure and fullness rather than sharp pain. Pain above 6/10 despite over-the-counter pain relievers may indicate acute middle ear infection requiring antibiotic evaluation.
Bloody or Purulent Discharge: Blood-tinged or yellow-green pus-like discharge indicates eardrum perforation with possible infection. This requires medical treatment to prevent complications and ensure proper healing.
Vertigo with Nausea/Vomiting: True vertigo—the sensation that the room’s spinning—suggests inner ear involvement or vestibular dysfunction requiring professional evaluation.
Signs Your Eardrum May Have Ruptured
Eardrum perforation sometimes occurs from aggressive pressure equalization attempts, severe infection, or extreme barotrauma. Key indicators include: sharp pain that suddenly stops (the pressure releases when the drum tears), clear fluid or blood draining from the ear canal, significant hearing reduction in the affected ear, and sometimes tinnitus (ringing or buzzing) onset. Most small perforations heal spontaneously within 6-8 weeks if kept clean and dry, but they require medical documentation and monitoring.
If You Suspect Perforation: Keep water out of the ear—no swimming, and use cotton ball coated with petroleum jelly as a water barrier during showers. Don’t use ear drops unless prescribed by your provider. Avoid nose blowing or Valsalva maneuvers, which can force bacteria through the perforation. Schedule evaluation within 1-2 days.
Potential Complications of Untreated ETD
Acute Otitis Media: Trapped fluid in the middle ear creates an ideal environment for bacterial growth. What began as sterile ETD can develop into a bacterial middle ear infection requiring antibiotic treatment.
Serous Otitis Media (Fluid Accumulation): Chronic ETD can lead to persistent fluid behind the eardrum—not infected, but impeding hearing and creating fullness. This fluid won’t drain without restoring eustachian tube function. Children develop this more commonly than adults; it can affect speech development and learning if sustained. Treatment may require extended medical management or eventual tube placement.
Hearing Impact: Temporary conductive hearing loss accompanies ETD and resolves when the tube dysfunction clears. However, recurrent or chronic ETD with repeated infections can cause permanent changes to middle ear structures over months to years—scarring on the eardrum that stiffens it, damage to the tiny bones (ossicles) that conduct sound, or cholesteatoma formation (abnormal skin growth behind the eardrum). These complications develop over time, which is why chronic symptoms merit investigation.
How to Work With Your Healthcare Provider on Persistent Ear Blockage

When ETD doesn’t resolve, effective medical coordination depends on bringing objective data rather than vague descriptions. Healthcare providers make better decisions when they can review your complete treatment history and understand response patterns.
Document Your Trial Before the Appointment
Create a written timeline that includes: exact symptom onset date, triggering event if known, severity progression, complete list of interventions with dates, subjective improvement percentage for each (0% = no change, 100% = resolved), and associated symptoms (hearing loss, pain level, drainage, dizziness).
Questions to Ask During Your Visit
- “Based on examination, is this eustachian tube dysfunction, fluid behind the eardrum, or something else?” — Accurate diagnosis determines treatment.
- “What’s the typical resolution timeline for my specific situation?” — Sets realistic expectations.
- “What are my stop criteria—when should I return if this treatment doesn’t work?” — Prevents indefinite continuation of ineffective treatment.
- “Are there underlying factors we should investigate—allergies, reflux, sinus disease?” — Addresses root causes rather than just symptoms.
Understanding Examination and Testing
Otoscopy: Your provider visualizes your eardrum looking for: eardrum position (retracted inward or bulging outward), color changes, perforation or scarring, and wax blockage.
Tympanometry: This test measures eardrum movement and middle ear pressure. Abnormal tympanometry confirms ETD and guides treatment intensity.
Audiometry: If you report significant hearing loss, formal hearing testing quantifies the deficit and determines type—conductive hearing loss accompanies ETD and reverses with treatment.
Nasal Endoscopy: For chronic or recurrent ETD, ENT specialists may visualize the eustachian tube opening in your nasopharynx using a small flexible camera through your nose. This identifies structural blockages (enlarged adenoids, polyps, masses), chronic inflammation, or anatomic variations affecting tube function. Local anesthetic makes the procedure tolerable; it provides direct visualization that external examination can’t achieve.
Treatment Hierarchy Discussion
First-Line: Prescription Nasal Corticosteroids — Provide sustained anti-inflammatory effect superior to OTC versions. These work best for ETD related to inflammation—allergies, post-viral, chronic sinusitis.
Second-Line: Short-Course Oral Corticosteroids — If inflammation is severe, a 5-7 day prednisone taper can provide rapid relief. Use requires medical supervision due to side effects and interactions.
Antibiotics (Selective Use) — Prescribed only when bacterial infection is confirmed or highly suspected. ETD alone without infection doesn’t benefit from antibiotics.
Specialty Referral Triggers — Your primary provider will refer to ENT (otolaryngology) when: symptoms persist >3-4 weeks despite appropriate medical management, recurrent episodes occur (3+ episodes within 6 months), complications develop (persistent hearing loss, chronic fluid), or structural problems are suspected. ENT evaluation includes specialized examination and testing, plus procedural intervention options.
Advanced Interventions: For refractory chronic ETD, balloon dilation shows 60-75% success rates with symptom improvement lasting 6-12+ months. Tympanostomy tubes provide alternative drainage when the eustachian tube won’t function properly. Neither procedure is first-line treatment—they’re reserved for cases that have exhausted conservative management.
Preventing Recurrent Ear Pressure Issues
Prevention strategies reduce recurrence risk by addressing underlying factors that predispose to ETD.
For Frequent Flyers and Altitude Changes
Use nasal corticosteroid spray daily for 3 days before traveling if you have ETD history. Take an oral decongestant 30 minutes before descent. Stay awake during descent and chew gum continuously. Pressure-regulating earplugs (EarPlanes) cost $10-15 and are worth trying if you fly regularly.
For Allergy Sufferers
HEPA air filters in bedrooms reduce allergen exposure. Dust mite covers on pillows and mattresses prevent exposure. Daily nasal saline irrigation during allergy seasons mechanically removes pollen before it triggers inflammation. Daily antihistamine use during peak seasons prevents symptom development.
Lifestyle Optimization
Humidity Maintenance: Indoor humidity between 40-50% maintains optimal mucosal function. Use a humidifier in winter or dry climates.
Adequate Hydration: Most adults benefit from 8-10 cups of fluid daily. Morning urine should be pale yellow.
Sleep Position Elevation: Sleeping with your head elevated 30-45 degrees promotes overnight drainage.
GERD Management: If you have heartburn or chronic throat clearing alongside ETD, address reflux: eat dinner 3+ hours before bed, elevate head during sleep, avoid trigger foods.
Smoking Cessation: Tobacco smoke causes chronic inflammation of respiratory mucosa including the eustachian tube lining. If you smoke and have recurrent ear issues, cessation will reduce recurrence more than any other single intervention.
Separating Ear-Popping Facts From Fiction
| Myth | Fact |
|---|---|
| “Force the Valsalva maneuver until your ears pop” | Forcing pressure can rupture your eardrum or worsen existing middle ear damage. If gentle attempts fail after 24-48 hours, escalate to medical evaluation—don’t increase force. |
| “Ear candling removes blockages” | Ear candling is ineffective and dangerous. Studies show no wax removal or pressure relief, and it causes burns, eardrum perforation, and ear canal obstruction. The FDA issued a consumer safety warning advising complete avoidance. |
| “Your ears should pop immediately” | ETD from inflammation may take 3-7 days to resolve even with proper treatment. Simple altitude-related pressure equalizes quickly; ETD from congestion requires addressing the underlying inflammation first. |
| “Q-tips can help unblock ears” | Q-tips push wax deeper and can damage ear canal or eardrum. ETD is middle ear dysfunction behind your eardrum—no external object reaches that space. They add earwax impaction to your existing problem. |
| “All ear pressure needs identical treatment” | Simple barotrauma (altitude changes) resolves quickly with mechanical techniques. ETD from congestion requires anti-inflammatory treatment. Chronic ETD may require addressing GERD, allergies, or structural issues. Accurate diagnosis determines appropriate treatment. |
Common Questions About Stubborn Ear Blockage
How long should I try home remedies before seeing a doctor?
Follow the 5-day rule with progressive escalation: foundational remedies (days 1-2), advanced techniques (days 2-3), OTC medical support (days 3-5). Don’t wait the full five days if you see zero improvement. Seek immediate care for severe pain, sudden hearing loss, bloody discharge, high fever, or significant dizziness.
Can I fly or dive with ears that won’t pop?
Avoid flying or scuba diving during active ETD if possible. Pressure changes worsen existing blockage and risk barotrauma. If flight is unavoidable, use oral decongestant 30-60 minutes before descent, stay awake throughout landing, and continuously chew gum. For diving, any ear dysfunction is a contraindication.
Will my hearing return to normal?
Most ETD cases resolve within 1-3 weeks with proper treatment, and hearing returns fully. The hearing loss is conductive (mechanical blockage) rather than sensorineural (nerve damage), so it reverses when the blockage clears. Persistent cases lasting over 3 weeks require ENT evaluation.
Why do my ears feel worse in the morning?
Overnight mucus accumulation while lying flat creates morning pressure that improves throughout the day. Solutions: sleep with head elevated 30-45 degrees, use a humidifier if indoor air is dry, try nasal saline irrigation before bed, and address potential GERD.
Are there natural alternatives to decongestants and nasal sprays?
Steam inhalation, nasal saline irrigation, adequate hydration (8-10 cups daily), and sleep elevation are evidence-based natural approaches that work through mechanical mucus clearance and reduced inflammation. These methods work well for mild to moderate ETD. However, they’re not substitutes for medical evaluation if symptoms persist beyond 5 days, worsen, or include red-flag features. The Remedy Verified philosophy emphasizes natural approaches that coordinate with medical care rather than replace it.
Moving Forward: From Frustration to Resolution
Persistent ear blockage feels isolating when standard methods fail, but understanding the distinction between simple pressure changes and eustachian tube dysfunction transforms frustration into a systematic path forward. The four-tier protocol outlined here progresses from conservative home remedies through medical coordination, with each step defined by specific timelines and clear stop criteria.
What separates this approach from generic advice is matching interventions to underlying causes while setting realistic expectations. Post-viral inflammation needs different management than allergy-driven blockage or altitude-related barotrauma.
Here’s your first action: Set a timer for 10 minutes, boil water for steam inhalation, and start Tier 1 today. Give each tier its full time window before escalating. If symptoms persist beyond 5 days or red-flag features develop, schedule medical evaluation with your complete trial documentation.
Most eustachian tube dysfunction resolves within 1-3 weeks when the underlying cause is addressed systematically—and you now have the roadmap to get there.
References
- American Academy of Otolaryngology–Head and Neck Surgery. Eustachian Tube Dysfunction. ENT Health; 2024.
- National Institute on Deafness and Other Communication Disorders. Ear Infections in Children. U.S. National Institutes of Health; 2021.
- American Academy of Otolaryngology–Head and Neck Surgery. Ears and Altitude (Barotrauma). ENT Health; 2023.
- Schilder AGM, et al. Eustachian tube dysfunction: consensus statement on definition, types, clinical presentation and diagnosis. Clinical Otolaryngology (PMC). 2015;40(5):407-411.
- U.S. Food and Drug Administration. Don’t Get Burned: Stay Away from Ear Candles. FDA Consumer Updates; 2023.
- Randrup TS, Ovesen T. Balloon eustachian tuboplasty: a systematic review. Otolaryngology–Head and Neck Surgery (PubMed). 2015;152(3):383-392.
Author Bio
The Remedy Verified Team explores evidence-based natural approaches that coordinate with medical care rather than replace it. Our ear health content translates ENT research into systematic protocols with defined timelines, measurable outcomes, and clear medical coordination guidelines. We emphasize data-driven decision making—try conservative approaches with specific stop criteria, track objective results, and escalate to professional care when home management reaches its limits. Learn more about our evidence-based approach to natural health.
⚠️ Disclaimer
The information provided in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. Eustachian tube dysfunction and ear-related conditions vary significantly in cause and severity. Natural remedies, over-the-counter treatments, and home management strategies may affect individuals differently and are not appropriate for all cases—particularly those involving severe pain, hearing loss, discharge, or other red-flag symptoms requiring immediate medical evaluation.
Always consult a qualified healthcare professional before attempting to treat persistent ear blockage, especially if you have existing medical conditions, are pregnant, take prescription medications, or experience symptoms lasting more than 5 days. Some techniques described carry risk of eardrum rupture if performed incorrectly or when contraindicated.
Remedy Verified does not provide medical services, and the content shared here should not be considered a substitute for professional medical examination, diagnosis, or treatment planning. The systematic protocols and timelines provided are general guidelines—your individual situation may require different approaches. Use of this website and its information is at your own risk. When in doubt, err toward professional evaluation rather than continued self-management.
Related Articles
This section will be populated with contextually relevant internal links.
- High Blood Pressure: Effective Management Strategies(Opens in a new browser tab)
- How to Get Rid of Inflammation in the Body: 7 Science-Backed Methods
- Systolic Blood Pressure: What Your Top Number Really Means
- Can Garlic Lower Blood Pressure? Science-Backed Facts
- High Cortisol Levels: Causes, Symptoms & Natural Treatment Guide