Cloudy Urine in Women: Causes, When to Worry & What to Do
You’ve noticed your urine looks cloudy, milky, or hazy—and you’re wondering whether it’s something harmless or a sign you need to see a doctor. Cloudy urine in women can feel alarming, especially when you’re not sure if it’s caused by something in your urinary tract, vaginal discharge mixing with your sample, or just dehydration from a busy day.
Women face unique considerations when it comes to cloudy urine. Your anatomy makes you more vulnerable to urinary tract infections, hormonal fluctuations can affect vaginal discharge that contaminates samples, and pregnancy brings additional concerns like preeclampsia. Most articles treat cloudy urine as a generic topic—but female-specific factors matter for accurate self-assessment and knowing when to seek care.
This guide combines peer-reviewed research with practical guidance tailored to women’s urinary health. You’ll learn how to distinguish between harmless causes and red flags requiring medical attention, understand what tests your clinician may recommend, and discover evidence-based prevention strategies that address your unique anatomy and hormonal patterns. We’ll help you make informed decisions while emphasizing when professional evaluation is necessary.
What Does Cloudy Urine Mean for Women? (Quick Answer)
Cloudy urine in women is usually caused by harmless factors like dehydration, high dietary alkalinity, or vaginal discharge contaminating the urine sample during collection. The cloudiness you’re seeing may not be in your actual urine at all—normal vaginal discharge can mix with urine and create a milky appearance that resolves once you use a clean-catch method.
Most common causes in women:
- Vaginal discharge mixing with urine (not a urine problem at all)
- Dehydration making urine concentrated and murky
- Urinary tract infections (especially with burning or frequency)
- High alkaline diet (lots of fruits and vegetables)
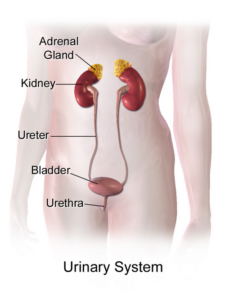
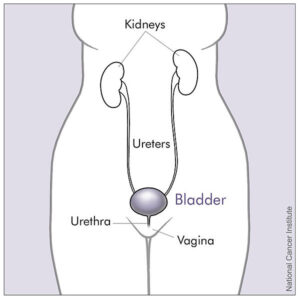
When to worry: Seek medical care within 24 hours if cloudiness persists beyond 48 hours or you experience burning during urination, pelvic pain, fever above 100.5°F, foul odor, or visible blood. Women face 8 times higher UTI risk than men due to shorter urethra anatomy—about 1.5 inches versus 8 inches—making bacterial infections more common and requiring prompt attention.

What to Do Right Now (Quick Decision Guide)
If you ONLY have cloudy urine with no other symptoms:
- Drink 16-20 ounces of water immediately
- Wait 2-3 hours and check your next urine sample
- Use clean-catch midstream technique (urinate briefly, then collect, then finish)
- If still cloudy after 24 hours of good hydration → schedule appointment
If you have cloudy urine PLUS burning, frequency, or urgency:
- Contact your healthcare provider today for urinalysis
- Don’t wait more than 24-48 hours—UTIs worsen without treatment
- Drink plenty of water while waiting for appointment
- Avoid irritants (caffeine, alcohol, spicy foods) until evaluated
If you have fever, severe pain, or vomiting with cloudy urine:
- Seek urgent care or emergency evaluation immediately
- These symptoms suggest kidney infection requiring prompt treatment
- Don’t drive yourself if you’re feeling very unwell
If you’re pregnant with any cloudy urine:
- Contact your obstetric provider the same day
- Never dismiss as “just pregnancy” without evaluation
- Untreated infections risk preterm labor
What Normal Urine Should Look Like (and Why Women’s Can Differ)

Healthy urine appears clear to transparent with a pale yellow color—similar to the color of straw or light lemonade. When you’re well-hydrated, your urine should be light enough that you could easily see through it if poured into a clear glass. The exact shade varies based on your fluid intake, with darker yellow indicating you need more water and nearly clear urine suggesting you’re well-hydrated or possibly overhydrated.
Urine consists of water (about 95%), dissolved salts, and metabolic waste products filtered by your kidneys. The balance of these components determines your urine’s pH level—a measure of how acidic or alkaline your urine is. Normal urine pH ranges from 4.5 to 8.0 on the pH scale, with most people falling between 5.5 and 7.0. When your urine becomes more alkaline (pH above 7.5), often from eating lots of fruits and vegetables, it can naturally take on a cloudier appearance even when you’re perfectly healthy.
Women experience several unique factors that can temporarily alter urine appearance. Hormonal fluctuations during your menstrual cycle affect vaginal discharge volume and consistency—what’s normal mid-cycle may look different during menstruation or ovulation. Hormonal birth control can increase vaginal discharge, which may contaminate urine samples more frequently. During pregnancy, hormonal changes increase both discharge production and urinary frequency, making it more challenging to collect a clean sample.
Understanding the difference between cloudy, foamy, milky, and hazy helps you communicate accurately with your clinician. Cloudy or milky urine looks opaque and white-tinged, like diluted milk. Foamy urine creates persistent bubbles on the surface, similar to beer foam, and may indicate protein in your urine. Hazy urine appears slightly unclear but not fully opaque—you can still see through it somewhat. Each presentation suggests different potential causes, so noting the specific appearance helps your healthcare provider narrow down the diagnosis.
Quick Self-Assessment: Is This Discharge or a Urine Problem?
Signs it’s likely vaginal discharge contamination:
- Cloudiness only appears in first part of stream, not midstream sample
- You notice discharge on underwear throughout the day
- External itching or irritation around vaginal opening
- Cloudiness varies with your menstrual cycle (worse mid-cycle or before period)
- No burning sensation when urinating
Signs it’s likely a urinary tract issue:
- Cloudiness persists even in clean midstream sample
- Internal burning feeling when you pee
- Needing to urinate frequently with little output
- Urgent sensation you can’t delay
- Strong, foul-smelling urine odor
- Pelvic pressure or discomfort
Common Causes of Cloudy Urine in Women (and Why We’re More Vulnerable)
Multiple factors can cause cloudy urine in women, ranging from completely harmless to conditions requiring medical treatment. We’ll cover each cause with specific context for female anatomy and hormones, so you understand not just what might be happening but why women face different risks than men.
Quick Reference: Top Causes at a Glance
| Cause | How Common | Key Identifying Features | Action Needed |
|---|---|---|---|
| Vaginal discharge | Very common | Clears with midstream sample; vaginal symptoms | None if normal; treat if abnormal |
| Dehydration | Very common | Dark urine; clears with hydration in 24hrs | Drink 8-10 glasses water daily |
| UTI | Common | Burning, frequency, urgency, odor | Medical care within 24-48hrs |
| Alkaline diet | Common | High fruit/vegetable intake; no other symptoms | None needed; benign |
| Yeast infection/BV | Common | Vaginal itching, abnormal discharge, odor | Medical care within 1 week |
| STI | Less common | Abnormal discharge, recent exposure | Medical care within 1 week |
| Kidney stones | Less common | Severe flank pain, blood in urine | Same-day medical care |
| Proteinuria | Less common | Foamy urine, swelling, fatigue | Medical care within 1 week |
Urinary Tract Infections (UTIs): The Leading Cause
UTIs are the most common medical cause of cloudy urine in women, leading to more than 8 million doctor visits annually. The milky or hazy appearance comes from white blood cells, bacteria, and sometimes small amounts of blood or pus entering your urinary tract as your immune system fights the infection. You’ll typically notice other symptoms alongside the cloudy appearance—burning or pain when you urinate, needing to go frequently (often with little urine output), urgency that feels impossible to ignore, or pelvic discomfort.
Your shorter urethra creates a fundamental vulnerability: bacteria from the vaginal or rectal area need to travel only 1.5 inches to reach your bladder, compared to the 8-inch journey in males. Sexual activity, wiping technique, certain types of birth control (especially spermicides and diaphragms), menopause-related vaginal changes, and pregnancy all increase your UTI risk.
Untreated UTIs can progress to kidney infections (pyelonephritis), a more serious condition requiring immediate medical care. If you develop fever above 100.5°F, severe back or flank pain, nausea, vomiting, or chills alongside cloudy urine, contact your healthcare provider immediately or seek urgent care. Kidney infections require prompt antibiotic treatment to prevent permanent kidney damage and potential bloodstream infection.
Vaginal Discharge Contamination: The Most Overlooked Cause
This is the most frequently overlooked cause of “cloudy urine” in women—because what you’re seeing isn’t cloudy urine at all. Normal vaginal discharge varies throughout your menstrual cycle, from thin and clear after your period to thick and white before menstruation. When this discharge mixes with urine during collection, it creates a milky or cloudy appearance that can alarm you unnecessarily.
Normal discharge is white to clear, has a mild or no odor, and changes in volume and consistency with your cycle—typically increasing around ovulation (mid-cycle) and before your period. If your “cloudy urine” clears up when you carefully collect a midstream sample (urinating briefly first, then collecting, then finishing), discharge contamination is likely the culprit rather than a urinary problem.
Abnormal discharge patterns suggest infections or imbalances that need attention. Yeast infections produce thick, white, cottage-cheese-like discharge with itching and irritation. Bacterial vaginosis creates thin, grayish discharge with a distinctive fishy odor, especially after sex. Trichomoniasis (a common STI) causes yellow-green, frothy discharge with a foul smell. These conditions affect the vagina, not your urinary tract, but the discharge they produce will make your urine appear cloudy when mixed during collection.
Vaginitis: When Vaginal Inflammation Causes Cloudy Urine
Vaginitis refers to inflammation or infection of the vagina and possibly the surrounding vulva. The three most common types—yeast infections (candidiasis), bacterial vaginosis, and trichomoniasis—all increase vaginal discharge that can make urine look cloudy when mixed during collection. Beyond creating murky or milky-looking urine, these conditions cause vaginal itching, irritation, abnormal discharge color or odor, and sometimes painful urination (because urine touches inflamed vaginal tissues, not because your urinary tract is infected).
Many women confuse vaginal symptoms with UTI symptoms because both can cause discomfort during urination. The key difference: UTIs cause internal burning or pain that feels like it’s coming from inside your bladder or urethra, while vaginitis causes external burning when urine contacts inflamed vaginal or vulvar skin. If you’re experiencing vaginal itching, abnormal discharge, or external irritation, coordinate with your clinician for an exam—vaginal swabs and visual inspection can quickly distinguish between these conditions.
Pregnancy and Cloudy Urine: What’s Normal vs. Concerning
Pregnancy brings hormonal shifts that increase vaginal discharge (leukorrhea), making discharge-related cloudy urine more common. Morning sickness can cause dehydration, concentrating your urine and making it appear darker and cloudier. Increased urinary frequency means you’re producing urine continuously, sometimes not allowing your bladder to fully dilute its contents before you need to go again.
Pregnant women face higher UTI risk—hormonal changes relax the urinary tract muscles, and the growing uterus can partially obstruct urine flow, creating conditions where bacteria multiply more easily. Cloudy urine during pregnancy should never be dismissed as “just normal pregnancy changes” without evaluation, because untreated UTIs can lead to preterm labor and low birth weight.
Preeclampsia, a serious pregnancy complication, can cause proteinuria (protein in urine) that makes urine appear cloudy or foamy. If you’re pregnant and notice cloudy urine along with swelling in your hands or face, severe headache, vision changes (spots or blurriness), or upper abdominal pain, contact your healthcare provider immediately—these symptoms require urgent evaluation.
Sexually Transmitted Infections (STIs)
Common STIs including chlamydia, gonorrhea, and trichomoniasis can cause cloudy urine through increased white blood cell production and abnormal discharge. These infections prompt your immune system to send white blood cells to fight the bacteria or parasites, and those cells can appear in your urine or mix with vaginal discharge to create cloudiness.
STI symptoms overlap significantly with UTI symptoms—painful urination, unusual discharge, pelvic discomfort—making it difficult to self-diagnose. The critical difference: STIs more commonly cause vaginal discharge with abnormal color (yellow, green, or gray), genital sores or bumps, pain during intercourse, and bleeding between periods or after sex. If you’ve had unprotected sexual contact or a new partner within the past several weeks, mention this to your clinician—STI testing may be appropriate alongside UTI screening.
Dehydration: When Concentrated Urine Looks Murky
When you don’t drink enough fluids, your kidneys conserve water by producing less, more concentrated urine. This concentration makes urine appear darker and can create a cloudy or hazy appearance as minerals and waste products become more densely packed. Dehydration is particularly common during menstruation (when you may retain water but still need consistent fluid intake), in hot weather, during exercise, or when you’re busy and forget to drink regularly.
Women generally need 2.0-2.7 liters (about 8-11 cups) of total fluids daily from all sources, though individual needs vary based on activity level, climate, and overall health. Your urine color provides immediate feedback: pale yellow indicates good hydration, while dark yellow to amber suggests you need more fluids. If increasing your water intake to 8-10 glasses daily clears your cloudy urine within 24-48 hours, dehydration was likely the cause.
Kidney Stones in Women: Symptoms and Cloudy Urine
Kidney stones can cause cloudy urine, especially if they’re blocking urine flow or irritating the urinary tract lining. Small crystals forming in your urine may create cloudiness even before they develop into symptomatic stones. Women who form calcium oxalate stones (the most common type) may notice cloudy urine when consuming high-oxalate foods like spinach, nuts, chocolate, or tea—though this alone rarely causes concerning cloudiness.
Kidney stones typically announce themselves with severe pain—sudden, intense cramping in your back, side, lower abdomen, or groin that comes in waves. You may notice blood in your urine (pink, red, or brown color), nausea, vomiting, fever if infection develops, and urgent, frequent urination. If you experience these symptoms alongside cloudy urine, seek medical evaluation the same day—kidney stones can require pain management and sometimes intervention to pass.
Birth Control and Menopause: How Hormones Affect Urine Appearance
Hormonal contraceptives alter vaginal pH and increase cervical mucus production, which can lead to more noticeable vaginal discharge throughout your cycle. This isn’t harmful—it’s your body responding to synthetic hormones—but it does mean you may observe cloudy or milky urine more frequently simply from discharge contamination during collection. If you recently started or changed birth control methods and noticed cloudy urine appearing, this timing suggests a hormonal influence.
Menopause brings declining estrogen levels that thin vaginal tissues, reduce natural lubrication, and change vaginal pH. These changes can increase urinary tract infection risk and may alter discharge patterns. Postmenopausal women who notice new or persistent cloudy urine should coordinate with their clinician—sometimes vaginal estrogen therapy can restore tissue health and reduce urinary symptoms when appropriate for your overall health profile.
Proteinuria: When Protein in Urine Creates Cloudiness
Excessive protein in your urine can create a cloudy or foamy appearance, often described as looking like beaten egg whites. Proteinuria may indicate kidney damage or disease, though temporary protein elevation can occur after intense exercise, dehydration, or during fever. Persistent proteinuria requires evaluation because it suggests your kidneys aren’t filtering properly—protein molecules that should stay in your bloodstream are leaking into your urine.
If your cloudy urine is accompanied by foamy bubbles that don’t dissipate quickly, swelling in your hands, feet, or face (edema), fatigue, or decreased urine output, contact your healthcare provider for kidney function testing. Simple urinalysis can detect protein levels, and if elevated, your clinician will likely order additional tests to determine the cause and extent of kidney involvement.
Medications and Supplements
Certain medications can change urine appearance, making it cloudy, darker, or even colorful. Antibiotics, particularly nitrofurantoin (commonly prescribed for UTIs), can darken urine and create cloudiness. Diuretics concentrate urine by increasing fluid elimination. High-dose vitamin supplements—especially B vitamins and vitamin C—can alter urine appearance and pH. Some multivitamins contain phosphate, which may precipitate in urine and cause temporary cloudiness.
If cloudiness started within a few days of beginning a new medication or supplement, note this timing and discuss it with your prescriber or pharmacist. Don’t stop prescription medications without guidance, but you may choose to temporarily discontinue supplements to see if cloudiness resolves—then reintroduce them one at a time to identify the culprit if desired.
When Cloudy Urine Signals Serious Conditions
| Condition | Key Distinguishing Features | Urgency Level |
|---|---|---|
| Urinary Tract Infection (UTI) | Burning urination, frequency, urgency, pelvic discomfort | 24-48 hours |
| Kidney Infection | High fever, severe back/flank pain, nausea, vomiting | Same day/urgent care |
| Preeclampsia (pregnancy) | Swelling, severe headache, vision changes, high blood pressure | Immediate/ER |
| Kidney Disease | Foamy urine, persistent protein, swelling, fatigue | Within 1 week |
| STI | Abnormal discharge color/odor, genital symptoms, pelvic pain | Within 1 week |
| Kidney Stones | Severe cramping pain, blood in urine, nausea | Same day |
Most women experiencing cloudy urine have benign, self-resolving causes. However, understanding which accompanying symptoms signal more serious conditions helps you make appropriate decisions about when to seek care. When in doubt, a simple urinalysis can provide clarity—it’s a quick, noninvasive test that definitively identifies whether infection, protein, blood, or other abnormalities are present.
How to Distinguish Vaginal Discharge from Actual Urine Problems
The single most important skill for women concerned about cloudy urine is learning to distinguish between actual urinary changes and discharge contamination. This distinction prevents unnecessary panic, saves you from emergency visits for non-urgent issues, and helps you accurately describe symptoms to your healthcare provider. Most articles skip this critical assessment step—yet it’s the first thing experienced clinicians evaluate.
The Clean-Catch Midstream Collection Technique
Healthcare professionals use a specific collection method to minimize discharge contamination, and you can replicate this at home for self-assessment. Start by washing your hands thoroughly. Using mild soap and water, gently clean your genital area from front to back, then rinse completely and pat dry with a clean towel or paper towel. This removes external discharge without introducing new bacteria.
Here’s the technique that matters most: Begin urinating into the toilet for 1-2 seconds to flush your urethra, then—without stopping the stream—position a clean container to catch the middle portion, then finish urinating into the toilet. This “midstream” sample captures urine that hasn’t contacted your vaginal area or mixed with external discharge. If your midstream sample appears clear but your initial stream looked cloudy, discharge contamination was creating the appearance—not an actual urine problem.
For the most accurate assessment, check your sample immediately after collection. Urine that sits for more than 5-10 minutes may develop cloudiness as minerals precipitate at room temperature—this doesn’t indicate a problem, just normal chemical changes that occur outside your body. Real urinary cloudiness appears immediately and persists even in a clean midstream sample.
Visual and Symptomatic Clues
Your accompanying symptoms provide critical context for interpretation. Vaginal discharge that contaminates urine typically comes with vulvovaginal symptoms—external itching around your labia or vulva, irritation that worsens with friction from underwear or physical activity, or observable discharge on your underwear throughout the day. You might notice discomfort during sex or when inserting a tampon if vaginitis is present.
True urinary cloudiness, especially from UTIs, presents differently: internal burning that feels like it originates inside your bladder or urethra (not on external tissues), sudden urges to urinate that feel impossible to delay, frequent trips to the bathroom with minimal urine output each time, and pelvic pressure or discomfort that’s deep rather than surface-level. Some women describe the sensation as “feeling like you need to pee even right after you just went.”
“Most women experiencing discharge-related cloudiness notice external symptoms—itching, irritation—while UTI symptoms are predominantly internal and urinary-specific.” — Dr. Sarah Chen, Urogynecologist
Timing Patterns and Cycle Awareness
Tracking when cloudiness appears relative to your menstrual cycle offers diagnostic clues that most women overlook. Normal vaginal discharge increases in volume around ovulation (typically days 12-16 of your cycle) and immediately before menstruation—these are the times you’re most likely to see discharge-contaminated urine. If your “cloudy urine” consistently appears mid-cycle and resolves afterward, discharge rather than infection is almost certainly responsible.
Conversely, UTI symptoms don’t follow menstrual patterns unless you have anatomical factors or behaviors that create predictable vulnerability windows. Some women develop UTIs consistently after sexual activity (honeymoon cystitis), after menstruation (when pH changes occur), or during times of stress (when immune function may be compromised). Recognizing your personal patterns helps you and your clinician develop targeted prevention strategies.
The pH and Odor Test
Normal vaginal pH ranges from 3.8 to 4.5—slightly acidic to maintain healthy bacterial balance. Normal urine pH is typically 5.5 to 7.0. When vaginal discharge with its lower pH mixes with urine, you might notice the combined sample has a distinctive odor that’s different from urine alone. Bacterial vaginosis specifically creates a “fishy” odor that intensifies with alkaline exposure (including mixing with urine), while yeast infections may have a yeasty, bread-like smell.
UTI-related cloudiness often produces a strong, foul, ammonia-like odor that’s distinctly unpleasant and different from normal urine smell. If your cloudy urine smells strongly of ammonia or has a rotting quality, infection becomes more likely. However, concentrated urine from dehydration can also smell strong—the difference is that infection-related odor persists even after you’ve hydrated well for 24 hours.
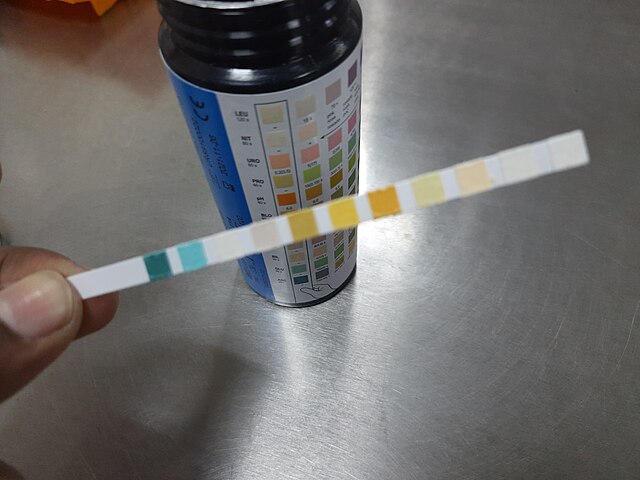
At-Home pH Testing (When and How)
Vaginal pH test strips are available over-the-counter and can help you assess whether abnormal discharge might be contaminating your samples. A vaginal pH above 4.5 suggests bacterial vaginosis or trichomoniasis rather than a yeast infection (which maintains normal pH). While this doesn’t diagnose UTIs, it can indicate whether vaginal infection treatment should be your priority.
To use vaginal pH strips correctly, collect a sample of discharge from your vaginal opening (not deeper inside) during mid-cycle when discharge is most abundant. Press the strip against the discharge for the time specified in the instructions—usually 10-30 seconds—then compare the color change to the provided chart. If results show pH above 4.5 and you have vaginal symptoms, coordinate with your clinician for evaluation even if your urine itself appears normal.
When Self-Assessment Isn’t Enough
Some situations make it difficult to confidently distinguish between causes, and that’s when professional evaluation becomes valuable rather than optional. If you’ve tried the clean-catch technique multiple times and still observe cloudiness, if you have both vaginal and urinary symptoms occurring together, if you’re pregnant, or if you have diabetes or another condition affecting immune function, don’t rely solely on self-assessment. A simple urinalysis ($20-50 without insurance at many clinics) and possibly a vaginal swab provide definitive answers within 24-48 hours.
When Cloudy Urine Requires Medical Attention: A Women’s Guide
Knowing when to seek care—and how urgently—prevents both unnecessary emergency visits and dangerous delays in treatment. Most women struggle with this decision because medical symptoms exist on a spectrum, and our healthcare system hasn’t provided clear guidance for self-triage. This section gives you specific criteria so you can make confident decisions about timing and care setting.
Seek Medical Care Within 24 Hours If You Have:
Cloudy urine lasting more than 48 hours even after increasing hydration and using clean-catch collection methods. Persistent cloudiness suggests an underlying cause that requires diagnosis—either through urinalysis to detect infection or kidney problems, or through examination to identify vaginal conditions. While not an emergency, don’t let this extend beyond 2-3 days without evaluation.
Burning or pain during urination that’s clearly internal (not external skin irritation from discharge). This dysuria indicates urethral or bladder involvement and strongly suggests UTI, especially when combined with frequency and urgency. Delaying treatment allows bacteria to multiply and potentially ascend to your kidneys, which requires more aggressive treatment and carries greater complication risks.
Pelvic pain or pressure that feels deep in your lower abdomen or pelvis, particularly if it’s one-sided or accompanied by back pain. While occasional cramping is normal, persistent or worsening pelvic pain alongside cloudy urine may indicate infection, kidney stones, or other conditions requiring imaging and evaluation.
Foul-smelling urine with strong ammonia or rotting odor that persists after hydration. Strong odor combined with cloudiness increases the probability of bacterial infection significantly—one study found that women reporting both symptoms had UTIs confirmed in 78% of cases upon testing.
Seek Urgent Care or Emergency Evaluation Immediately If You Experience:
Fever above 100.5°F (38°C) combined with cloudy urine, back pain, or urinary symptoms. Fever suggests the infection has become systemic or reached your kidneys. Kidney infections (pyelonephritis) can progress rapidly to sepsis if untreated, and pregnant women face additional risks including preterm labor. Don’t wait overnight—seek care within hours.
Severe back or flank pain (pain in your side, between your ribs and hip) that’s sudden, intense, or comes in waves. This pattern suggests either kidney infection or kidney stones. Both require prompt evaluation—kidney infections need immediate antibiotics, while kidney stones may need pain management and intervention if they’re large or completely blocking urine flow.
Visible blood in your urine (pink, red, or brown color) appearing alongside cloudiness. Small amounts of blood detected only on urinalysis are common with UTIs and less concerning, but visible blood requires same-day evaluation to rule out kidney stones, significant infection, or rarely, structural problems or malignancy.
Nausea, vomiting, or inability to keep fluids down occurring with urinary symptoms. These systemic symptoms indicate your infection or condition is affecting your whole body, and you may need intravenous fluids, medications, or closer monitoring than outpatient treatment provides.
Pregnancy-Specific Urgent Signs
If you’re pregnant, the threshold for seeking care should be lower because UTIs during pregnancy carry risks for both you and your baby. Contact your obstetric provider the same day you notice cloudy urine if you have any accompanying symptoms. Seek immediate care if you experience severe headache that doesn’t respond to usual remedies, vision changes including spots, flashing lights, or blurriness, swelling of your hands or face (not just feet—some ankle swelling is normal), or upper abdominal pain especially on your right side.
These symptoms combined with cloudy urine may indicate preeclampsia, a serious complication where high blood pressure and protein in urine can lead to seizures, placental abruption, or organ damage. Preeclampsia requires immediate treatment and close monitoring, sometimes including hospitalization or early delivery depending on your gestational age and severity.
“Pregnant women should never dismiss cloudy urine as ‘probably nothing’—untreated infections are a leading cause of complications we can easily prevent with prompt care.” — Dr. Jennifer Martinez, Maternal-Fetal Medicine
Schedule a Routine Appointment (Within 1 Week) If:
You have cloudy urine with vaginal symptoms like abnormal discharge color, itching, or irritation but no urinary burning or fever. These presentations suggest vaginitis or bacterial vaginosis rather than UTI—still requiring treatment but not urgent. A routine appointment allows time for cultures and swabs to identify the specific pathogen so treatment can be targeted.
You’ve had three or more UTIs in the past year (recurrent UTIs) even if your current symptoms are mild. Frequent infections warrant investigation into underlying anatomical factors, behavioral patterns, or immune considerations that make you vulnerable. Your clinician may recommend imaging studies, discuss prophylactic antibiotics or other prevention strategies, or identify contributing factors you can modify.
You’re postmenopausal and experiencing new or worsening urinary symptoms. Declining estrogen affects vaginal and urethral tissues, increasing infection risk and sometimes causing symptoms that mimic UTIs (urethral syndrome). Your provider can evaluate whether vaginal estrogen therapy, other hormone treatments, or different interventions might help reduce symptoms and infection frequency.
Your cloudy urine includes foam or bubbles that persist and don’t dissipate quickly. This presentation suggests possible proteinuria, which requires kidney function assessment through urinalysis and possibly blood tests. While not an emergency unless accompanied by severe symptoms, persistent protein in urine needs evaluation to determine cause and extent.
Safe to Monitor at Home (With Defined Stop Criteria):
Isolated episode of cloudiness with no other symptoms that you notice just once or occasionally. Try these steps for 24-48 hours: increase water intake to 8-10 glasses daily, practice clean-catch collection to eliminate discharge contamination, avoid potential irritants (harsh soaps, douches, scented products), and note whether cloudiness resolves.
Set clear stop criteria before you begin self-monitoring so you know exactly when to escalate. If cloudiness persists beyond 48 hours, if any painful or systemic symptoms develop, if you notice blood or foul odor, or if you feel increasingly unwell, contact your provider. This structured approach balances reasonable self-care with appropriate medical oversight.
What to Prepare Before Your Appointment
Maximize the value of your medical visit by preparing key information in advance. Write down when you first noticed cloudiness, how many times you’ve observed it, and what time of day (first morning urine often appears more concentrated and may look different). Note all accompanying symptoms even if they seem unrelated—vaginal itching, recent sexual activity, new medications or supplements, recent illness, menstrual cycle timing, and hydration patterns all provide diagnostic context.
List your current medications including birth control, any over-the-counter products, and supplements—especially if you recently started or changed anything. If you’ve tried home remedies (increased fluids, cranberry, probiotics), document what you did and whether you noticed improvement. This information helps your clinician determine whether you need testing, what tests to order, and whether symptoms suggest urinary tract involvement or vaginal conditions.
Be prepared to provide a urine sample using clean-catch technique—most clinics will test your urine on-site with a dipstick urinalysis that provides immediate results for infection markers, blood, protein, and pH. If infection is suspected but not confirmed, they’ll send a culture to the lab to identify the specific bacteria and its antibiotic sensitivities, with results typically available in 24-48 hours.
When Telehealth Is Sufficient vs. In-Person Required
Telehealth visits can effectively address many urinary symptoms, especially if you’ve had UTIs before and recognize your typical symptom pattern. Many providers will prescribe antibiotics via telemedicine if you describe classic UTI symptoms (burning, frequency, urgency, cloudy urine) without complicating factors. This saves you time and provides rapid treatment access.
However, in-person evaluation is necessary when physical examination or diagnostic testing is required—new vaginal symptoms needing swabs or pelvic exam, concerns about kidney involvement requiring flank palpation (pressing on your back to check for kidney tenderness), visible blood in urine, pregnancy, recurrent infections needing thorough evaluation, or any situation where your symptoms don’t clearly fit a straightforward diagnosis. When in doubt about which care setting is appropriate, call your provider’s office and describe your symptoms—their triage nurses can guide you based on your specific situation.
Understanding What Tests Your Clinician May Order

Urinalysis (UA): The first-line test that examines urine’s physical and chemical properties. A dipstick provides rapid results for white blood cells (leukocytes), red blood cells, bacteria presence (nitrites), protein, pH, and other markers. Most UTIs show positive leukocyte esterase and nitrites, though some bacteria don’t produce nitrites—meaning negative nitrites doesn’t completely rule out infection.
Urine culture and sensitivity: When urinalysis suggests infection or symptoms persist despite treatment, culture identifies the specific bacteria causing infection and tests which antibiotics will effectively treat it. This takes 24-48 hours but provides targeted treatment guidance, especially important for recurrent infections that may involve resistant bacteria.
Vaginal swab and wet mount: If your clinician suspects vaginal infection rather than UTI, they’ll collect vaginal discharge samples and examine them under a microscope. This quickly identifies yeast, trichomonas parasites, or clue cells suggesting bacterial vaginosis. Additional samples may be cultured if STI testing is indicated based on your symptoms and sexual history.
Blood tests: Reserved for concerning presentations like suspected kidney infection (when kidney function markers and inflammatory markers matter), recurrent infections (to check for diabetes or immune dysfunction), or proteinuria (to assess kidney disease severity).
Imaging studies: Kidney ultrasound, CT scan, or other imaging may be ordered if kidney stones are suspected, if you have recurrent infections potentially related to anatomical abnormalities, or if kidney infection symptoms are severe. These aren’t routine first-line tests but become important when symptoms suggest structural involvement.
Natural Prevention Strategies for Women: Evidence-Based Approaches That Work
Prevention strategies for cloudy urine and the conditions causing it require a nuanced approach that most articles oversimplify into generic advice like “drink more water.” While hydration matters, effective prevention addresses your specific vulnerability pattern, coordinates with your medical care rather than replacing it, and acknowledges that individual biology determines what actually works for you. We’ll focus on interventions backed by research—with clear guidance on when natural approaches make sense and when they don’t.
Smart Hydration: Beyond “Drink 8 Glasses”
You’ve heard “drink eight glasses of water” countless times, but that recommendation lacks the specificity you need for actual implementation. Research on UTI prevention suggests women should aim for 2.0-2.7 liters total daily fluids from all sources—but timing and distribution matter more than total volume alone.
Here’s a protocol based on urogyneology research: Front-load hydration in your morning and early afternoon hours (60-70% of daily intake before 3 PM) to ensure adequate bladder flushing during your active hours. Drink 8-12 ounces upon waking to dilute concentrated overnight urine. Consume another 16-20 ounces mid-morning and 16-20 ounces early afternoon. This pattern maintains consistent urine production without causing disruptive nighttime urination.
Track your urine color as immediate biofeedback—pale yellow (almost clear but with slight tint) indicates optimal hydration, while darker yellow means you need more fluids. If you’re producing very small amounts of urine infrequently (less than 4-5 times daily), increase intake. Excessive urination (more than 8-10 times daily with large volumes) may indicate overhydration or other issues worth discussing with your clinician.
One counterintuitive finding: Forcing fluids beyond comfortable levels doesn’t provide additional UTI protection and may dilute beneficial compounds in your urine that inhibit bacterial growth. The goal is consistent adequate hydration, not maximum possible fluid intake.
Post-Intercourse Hygiene: What the Research Actually Shows
Sexual activity increases UTI risk significantly—one study found women who had intercourse three or more times per week had a 3.5-fold higher UTI incidence. The mechanism is straightforward: physical contact introduces bacteria from the vaginal and anal areas into the urethra. However, the common advice to “urinate immediately after sex” lacks precision about timing and has mixed research support.
Here’s what works based on clinical trials: Urinate within 15 minutes after intercourse to flush bacteria before they can adhere to urethral walls—bacterial adherence begins within 20-30 minutes. The volume matters less than the mechanical flushing action, so don’t wait until you feel a full bladder. Even a small amount of urine provides benefit.
If you’re prone to UTIs, consider drinking 8 ounces of water 30 minutes before sexual activity. This ensures you’ll have urine ready to void afterward without forcing uncomfortable urination. For women experiencing recurrent post-coital UTIs despite hygiene measures, discuss single-dose prophylactic antibiotics with your clinician—one antibiotic tablet taken after intercourse reduces infection rates by 95% in studies, with minimal antibiotic exposure compared to daily prevention regimens.
Cranberry and D-Mannose: Separating Evidence from Marketing
Cranberry products represent the most-studied natural UTI prevention approach, but research quality and results vary dramatically. A 2017 Cochrane review found that cranberry products reduced UTI recurrence by about 26% compared to placebo—modest but measurable. However, cranberry juice cocktails (high in sugar) showed no benefit, and only products containing sufficient proanthocyanidins (PACs) demonstrated effectiveness.
If you want to trial cranberry for prevention, choose supplements standardized to deliver 36 mg PACs daily—the threshold shown effective in trials. Cranberry juice would require drinking 8-16 ounces of unsweetened pure cranberry juice daily (not cocktail), which most people find unpalatable. Take the supplement with water, ideally in morning and evening divided doses. Set a 3-month trial period with clear metrics: Are you experiencing fewer UTIs compared to the previous 3-6 months? If not, discontinue and reallocate resources.
D-mannose, a simple sugar that theoretically prevents E. coli bacteria from adhering to bladder walls, shows promise in small studies but lacks the robust evidence base of cranberry. A 2016 trial found D-mannose (2 grams daily) performed similarly to daily antibiotics for UTI prevention in women with recurrent infections. Because it’s generally safe and well-tolerated, some women find it worth trying—but coordinate with your clinician, especially if you have diabetes (D-mannose may affect blood sugar in theory, though studies haven’t shown significant impact at preventive doses).
Critical perspective: Neither cranberry nor D-mannose replaces antibiotics for active infections. They may reduce future infection frequency when used consistently, but they don’t treat established UTIs. If you develop symptoms, pursue diagnostic testing and appropriate treatment rather than hoping supplements will resolve infection.
Probiotic Strategies: Vaginal and Urinary Health
Your vaginal microbiome directly affects urinary tract health—Lactobacillus species maintain acidic vaginal pH that inhibits pathogenic bacteria growth and may prevent urinary tract colonization. Disruption of this protective flora (from antibiotics, hormonal changes, douching, or certain products) increases both vaginal infection and UTI risk.
Oral probiotics containing Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 have the strongest evidence for urogenital health. These specific strains colonize the vaginal tract when taken orally and reduce recurrent UTI rates in multiple trials. Standard gut-focused probiotics don’t provide the same benefit because different Lactobacillus strains have different tissue affinities.
Dosing protocol based on research: Take probiotics containing at least 1 billion CFU of the GR-1 and RC-14 strains daily, preferably in the evening. Allow 2-3 months for vaginal flora reestablishment. If you’re taking antibiotics for a UTI, continue probiotics but space them at least 2-3 hours apart from antibiotic doses to prevent the antibiotic from killing the beneficial bacteria before they reach your intestines.
Vaginal probiotic suppositories provide an alternative delivery method that places beneficial bacteria directly where they’re needed. Some women find this more effective than oral probiotics, though evidence is still emerging. Trial one approach at a time so you can assess which provides benefit for your particular situation.
Hygiene Practices: What Helps and What Creates Risk
Proper hygiene prevents contamination without disrupting your body’s natural defenses. The single most important practice: wipe front to back after urination and bowel movements every single time. This simple habit prevents fecal bacteria (particularly E. coli, responsible for 80-85% of UTIs) from reaching your urethra and vaginal area.
However, aggressive hygiene often backfires. Avoid douching entirely—it disrupts vaginal pH and flora, increasing infection risk rather than preventing it. Limit use of harsh soaps, scented products, feminine deodorants, and bubble baths in the genital area. These products alter pH, kill beneficial bacteria, and may cause irritation that makes you more vulnerable to infection. Plain water or gentle, unscented soap for external cleansing (labia and vulva only, not inside the vagina) provides adequate hygiene without harm.
Underwear choice affects the genital environment: cotton underwear allows air circulation and moisture evaporation, while synthetic materials trap moisture and create conditions where bacteria and yeast thrive. Sleep without underwear when possible to maximize airflow. After swimming or exercising, change out of wet clothing promptly—sitting in damp swimsuits or sweaty workout clothes prolongs warm, moist conditions that encourage bacterial growth.
“The best hygiene strategy isn’t more aggressive cleaning—it’s avoiding disruption of your body’s natural protective mechanisms while preventing fecal contamination.” — Dr. Lisa Hawes, Urologist
Dietary Patterns and pH Management
Your diet influences urinary pH, which affects bacterial growth potential and stone formation risk. While you shouldn’t obsess over every meal’s impact, understanding patterns helps you make informed choices—especially if you’re prone to recurrent UTIs or kidney stones.
High-protein, low-carbohydrate diets tend to acidify urine (lower pH), while diets rich in fruits and vegetables create more alkaline urine (higher pH). Neither extreme is necessarily better—optimal pH depends on your specific vulnerabilities. E. coli bacteria prefer neutral to slightly alkaline urine (pH 7.0-8.0), so moderately acidic urine (pH 5.5-6.5) may offer some protection. However, very acidic urine increases calcium oxalate kidney stone risk in susceptible individuals.
Vitamin C supplementation (500-1000 mg daily) acidifies urine and shows weak evidence for UTI prevention in some populations—though results are inconsistent enough that it’s not recommended as a primary strategy. If you trial vitamin C for prevention, use the same approach as other supplements: define a 2-3 month trial period, track infection frequency compared to your baseline, and continue only if you observe benefit.
Foods particularly relevant to urinary health include: fermented foods (yogurt, kefir, sauerkraut, kimchi) that support overall microbiome health; adequate protein to maintain immune function without excessive amounts that over-acidify urine; whole fruits rather than juices to obtain beneficial compounds without sugar loads; and adequate hydration-rich foods (cucumbers, melons, celery, lettuce) that contribute to your fluid intake.
Hormonal Considerations: Birth Control and Menopause
Hormonal birth control, particularly methods using spermicide, diaphragms, or certain IUDs, can increase UTI risk through different mechanisms. Spermicides alter vaginal pH and kill beneficial Lactobacillus bacteria alongside their intended targets. Diaphragms may partially obstruct the urethra and prevent complete bladder emptying, creating residual urine where bacteria multiply.
If you’re experiencing recurrent UTIs and use these contraceptive methods, discuss alternatives with your clinician. Switching to non-spermicidal condoms, hormonal pills, patches, or rings may reduce infection frequency while maintaining contraceptive efficacy. This conversation requires balancing your reproductive health goals, infection burden, and personal preferences—there’s no universal “best” choice.
Postmenopausal women face increased UTI risk as declining estrogen thins urethral and vaginal tissues, reduces protective mucus, and alters vaginal pH. For women with recurrent UTIs in this context, vaginal estrogen therapy (cream, tablet, or ring applied vaginally) can restore tissue health and significantly reduce infection rates—studies show up to 50% reduction in UTI recurrence.
Vaginal estrogen has minimal systemic absorption, making it safer than oral estrogen therapy for most women, including those with history of breast cancer in many cases. However, this requires individualized discussion with your clinician weighing your specific health history, risk factors, and current symptoms. If vaginal estrogen isn’t appropriate for you, other options include vaginal moisturizers, lubricants during intercourse, and meticulous hygiene practices adapted for sensitive postmenopausal tissues.
When to Consider Prophylactic Antibiotics
For women experiencing frequent recurrent UTIs (three or more per year) despite implementing behavioral and natural prevention strategies, low-dose prophylactic antibiotics represent an evidence-based option that dramatically reduces infection burden. This isn’t a failure or “giving up on natural approaches”—it’s appropriate medical care when prevention strategies alone prove insufficient.
Prophylactic regimens typically involve very low antibiotic doses (much lower than treatment doses) taken either daily, three times weekly, or as a single dose after intercourse if infections follow a post-coital pattern. Studies show these approaches reduce UTI frequency by 80-95%, vastly improving quality of life for women whose infections interfere with work, relationships, and daily activities.
Concerns about antibiotic resistance and microbiome disruption are valid but must be weighed against the burden of recurrent infections and repeated full-course antibiotic treatments. Discuss with your clinician: Is my infection pattern predictable enough for targeted prevention? Have we addressed all modifiable risk factors? Would the quality-of-life improvement justify prophylaxis risks? What’s my plan for eventually discontinuing if successful?
Alternative or complementary approaches to prophylaxis include methenamine hippurate, an antiseptic compound that releases formaldehyde in urine, creating an inhospitable environment for bacteria. It shows moderate effectiveness (about 50% reduction in UTI recurrence) without antibiotic resistance concerns. Some clinicians recommend combining methenamine with vitamin C to ensure adequate urine acidification for optimal effectiveness.
Prevention Tracking: Measuring What Works for You
Individual responses to prevention strategies vary dramatically—what works for one woman may provide no benefit for another. Rather than implementing everything simultaneously and hoping something helps, use a structured approach that reveals which interventions actually work for your unique biology.
Track these baseline metrics for 1-2 months before changing anything: number of UTIs or episodes of cloudy urine, timing relative to menstrual cycle, relationship to sexual activity, hydration patterns, and any other relevant health factors. This baseline establishes your natural frequency and patterns.
Then implement one prevention strategy at a time, allowing 2-3 months to assess effectiveness before adding another change. Track the same metrics you measured at baseline. After the trial period, compare: Has infection frequency decreased? Has symptom severity lessened? Are you experiencing any adverse effects from the intervention?
Keep what works, discontinue what doesn’t, and build your personalized prevention protocol gradually based on data rather than assumptions. This disciplined approach prevents the common problem of implementing five strategies at once, experiencing improvement, then continuing all five indefinitely without knowing which actually provided benefit. It also helps you and your clinician make informed decisions about whether to escalate to prophylactic antibiotics or try additional interventions.
Special Considerations: Pregnancy Prevention Strategies
Pregnancy changes the prevention calculus significantly. Some interventions safe outside pregnancy require modification: high-dose vitamin C supplementation may not be advisable, certain probiotic strains lack pregnancy safety data, and any signs of infection require more prompt evaluation due to preterm labor risks.
Safe, evidence-based pregnancy prevention strategies include: maintaining excellent hydration (8-12 cups daily minimum), emptying bladder every 2-3 hours even if you don’t feel full urge, urinating before and after intercourse, wearing cotton underwear and avoiding tight synthetic clothing, and continuing safe probiotics (many Lactobacillus strains are considered safe during pregnancy, but verify specific products with your obstetric provider).
Your prenatal care should include urinalysis at every visit to catch asymptomatic bacteriuria (bacteria in urine without symptoms)—a condition that’s relatively harmless outside pregnancy but increases preterm birth risk during pregnancy. If detected, treatment prevents progression to symptomatic infection. Don’t delay reporting any urinary symptoms to your obstetric provider, even if they seem minor.
Creating Your Prevention Protocol
| Strategy | Evidence Strength | Implementation Ease | Trial Period |
|---|---|---|---|
| Adequate hydration (2-3L daily) | Strong | Easy | 1-2 weeks |
| Post-intercourse urination (within 15 min) | Strong | Easy | Immediate |
| Front-to-back wiping | Strong | Easy | Immediate |
| Cotton underwear, avoid irritants | Moderate | Easy | 2-4 weeks |
| Cranberry (36mg PAC daily) | Moderate | Moderate (cost) | 3 months |
| Probiotics (GR-1/RC-14 strains) | Moderate | Moderate (cost) | 3 months |
| D-mannose (2g daily) | Weak-Moderate | Moderate (cost) | 3 months |
| Vaginal estrogen (postmenopausal) | Strong (specific population) | Requires Rx | 3-6 months |
| Prophylactic antibiotics | Very Strong | Requires Rx, monitoring | 6-12 months |
Start with the easy, high-evidence strategies (top of table) that cost little and cause no harm. If these prove insufficient after 2-3 months of consistent implementation, add one supplement or intervention from the moderate-evidence category. Reserve prescription interventions for recurrent infections that persist despite comprehensive prevention efforts. This tiered approach maximizes your chance of finding effective prevention while minimizing unnecessary interventions, costs, and potential side effects.
Key Takeaways: What Every Woman Should Know About Cloudy Urine
Most important points to remember:
- Discharge contamination is the #1 overlooked cause. Use clean-catch midstream technique before worrying—cloudy urine that only appears in your first stream isn’t a urine problem.
- Women face 8x higher UTI risk than men due to shorter urethra anatomy (1.5 inches vs. 8 inches), making bacterial infections more common and requiring prompt attention when symptoms appear.
- The 48-hour rule: Cloudy urine without other symptoms deserves 48 hours of good hydration and observation. If it persists beyond that or any concerning symptoms develop, seek medical evaluation.
- Internal vs. external burning matters. UTI burning feels internal (from bladder/urethra), while vaginal infection burning is external (urine touching inflamed skin). This distinction guides proper treatment.
- Prevention works best with a tiered approach: Start with hydration and hygiene basics, add evidence-based supplements only if needed, reserve antibiotics for recurrent infections despite other measures.
- Pregnancy changes the rules. Never dismiss cloudy urine as “just pregnancy”—contact your provider same-day for any urinary changes due to preterm labor risks.
- Track your patterns. Note timing relative to your cycle, sexual activity, and dietary changes. Personal data reveals what actually triggers your cloudiness and guides effective prevention.
Your next step: If you have cloudy urine right now, start with proper hydration (16-20 oz of water immediately) and clean-catch collection technique. If cloudiness persists beyond 48 hours or you develop burning, frequency, fever, or pain, contact your healthcare provider for evaluation. Most cases resolve quickly with simple interventions—but when they don’t, prompt medical care prevents complications and gets you back to normal faster.
Cloudy Urine Myths: What Women Get Wrong
| Myth | Fact |
|---|---|
| “Cloudy urine always means I have an infection.” | Most cloudy urine results from benign causes—dehydration, dietary pH changes, or vaginal discharge contaminating the sample. Infections typically include additional symptoms like burning, frequency, or fever. |
| “Cranberry juice cures UTIs.” | Cranberry products may help prevent some UTIs when used consistently (36mg PACs daily), but they don’t treat active infections. Once symptoms begin, you need diagnostic testing and appropriate treatment—usually antibiotics. |
| “I can diagnose a UTI myself based on symptoms.” | UTI symptoms overlap significantly with yeast infections, bacterial vaginosis, STIs, and other conditions. Only urinalysis and culture provide definitive diagnosis—self-diagnosis often leads to incorrect treatment. |
| “Vaginal discharge means something is wrong.” | Normal discharge varies throughout your menstrual cycle—thin and clear after periods, thicker and white before menstruation. Only abnormal color (yellow, green, gray), foul odor, or accompanying symptoms suggest infection. |
| “Holding my urine causes it to become cloudy.” | Holding urine increases UTI risk by allowing bacteria more time to multiply, but it doesn’t directly cause cloudiness. The cloudiness comes from the resulting infection, not from urine retention itself. |
| “Natural remedies are always safer than antibiotics.” | Untreated UTIs can progress to kidney infections causing permanent damage. When infection is present, antibiotics provide rapid, effective treatment with minimal side effects for most women. Natural approaches work best for prevention, not active infection treatment. |
Frequently Asked Questions About Cloudy Urine in Women
Can hormonal birth control cause cloudy urine?
Hormonal contraceptives don’t directly cause cloudy urine, but they increase vaginal discharge production and alter cervical mucus, which can contaminate urine samples more frequently. If you started birth control recently and noticed cloudiness, use clean-catch midstream collection to determine whether discharge is the cause. Some contraceptive methods (diaphragms, spermicides) increase UTI risk, potentially leading to infection-related cloudiness.
Is cloudy urine normal during pregnancy?
Pregnancy increases normal vaginal discharge (leukorrhea), making discharge-related cloudy urine more common. However, pregnant women also face higher UTI risk, and untreated infections can cause preterm labor and other complications. Never dismiss cloudy urine as “just pregnancy” without evaluation—contact your obstetric provider if cloudiness persists beyond 24-48 hours or if you develop any accompanying symptoms like burning, fever, or pelvic pain.
How do I collect a clean urine sample at home?
Wash your hands and gently clean your genital area from front to back with mild soap and water, then rinse thoroughly. Begin urinating into the toilet for 1-2 seconds to flush the urethra. Without stopping the stream, position a clean container to catch the middle portion of urine. Remove the container and finish urinating into the toilet. This midstream sample minimizes vaginal discharge contamination and provides the most accurate representation of your actual urine.
Can my menstrual cycle affect urine appearance?
Yes, hormonal fluctuations throughout your cycle influence vaginal discharge volume and consistency. Discharge typically increases around ovulation (mid-cycle, days 12-16) and just before menstruation, making discharge-related cloudy urine more likely during these windows. If your cloudiness consistently appears at the same point in your cycle and resolves afterward, discharge contamination rather than infection is likely responsible. True UTIs don’t follow menstrual patterns unless specific behaviors or anatomical factors create cyclical vulnerability.
What’s the difference between cloudy urine and foamy urine?
Cloudy urine appears opaque, milky, or hazy—you can’t see through it clearly. Foamy urine creates persistent bubbles on the surface (like beer foam) that don’t quickly dissipate. Cloudiness often results from infection, discharge, dehydration, or alkaline pH. Foamy urine more commonly indicates proteinuria (protein in urine), which may signal kidney problems and requires evaluation if persistent. Some overlap exists—both can appear together—but noting the specific presentation helps your clinician identify the cause.
Should I stop my medication if it causes cloudy urine?
Never stop prescription medications without guidance from your prescriber. Some medications (antibiotics, certain vitamins, diuretics) temporarily change urine appearance as a harmless side effect. Contact your pharmacist or prescriber to determine whether cloudiness is an expected effect, requires dose adjustment, or suggests a problem needing evaluation. For over-the-counter supplements causing cloudiness, you may choose to discontinue temporarily and observe whether urine clears—then reintroduce to confirm the supplement was responsible.
Can stress or anxiety cause cloudy urine?
Stress doesn’t directly cause cloudy urine, but chronic stress can suppress immune function and increase UTI vulnerability, potentially leading to infection-related cloudiness. Stress may also alter hydration habits (drinking less water) or cause you to hold urine longer (fewer bathroom breaks during busy periods), both of which increase infection risk indirectly. Managing stress through established techniques supports overall health but won’t treat or prevent cloudy urine if infection or other medical causes are present.
References
- Foxman B. Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin North Am. 2014;28(1):1-13. PMC3922003
- Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med. 2012;366(11):1028-1037. PubMed
- Jepson RG, Williams G, Craig JC. Cranberries for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD001321. Cochrane Library
- American College of Obstetricians and Gynecologists. Vaginitis in nonpregnant patients: ACOG Practice Bulletin, Number 215. Obstet Gynecol. 2020;135(1):e1-e17. ACOG
- Kranjcec B, Papeš D, Altarac S. D-mannose powder for prophylaxis of recurrent urinary tract infections in women: a randomized clinical trial. World J Urol. 2014;32(1):79-84. PubMed
- Reid G, Bruce AW. Probiotics to prevent urinary tract infections: the rationale and evidence. World J Urol. 2006;24(1):28-32. PubMed
- National Institute of Diabetes and Digestive and Kidney Diseases. Urinary Tract Infections in Adults. NIDDK
- Stapleton AE, Au-Yeung M, Hooton TM, et al. Randomized, placebo-controlled phase 2 trial of a Lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin Infect Dis. 2011;52(10):1212-1217. PubMed
- Gupta K, Trautner BW. Diagnosis and management of recurrent urinary tract infections in non-pregnant women. BMJ. 2013;346:f3140. BMJ
- Cleveland Clinic. Cloudy Urine: Causes, Treatment & What Does It Mean. Cleveland Clinic
- Centers for Disease Control and Prevention. Sexually Transmitted Infections Treatment Guidelines, 2021. CDC
- American Urological Association. Recurrent Uncomplicated UTI in Women: AUA/CUA/SUFU Guideline. AUA
Author Bio
The Remedy Verified team explores evidence-based approaches to common health concerns affecting women. We translate complex clinical research into practical guidance that helps you make informed decisions about your urinary and reproductive health. Our content emphasizes coordination with healthcare providers while empowering you with knowledge to recognize patterns, implement prevention strategies, and advocate for appropriate care. Learn more about our editorial approach and commitment to research-backed health information.
Disclaimer
⚠️ Disclaimer: The information provided in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. Natural remedies, supplements, and lifestyle changes may affect individuals differently. Always consult a qualified healthcare professional before making any changes to your diet, medications, or health routine—especially if you have an existing medical condition, are pregnant, or are taking prescription drugs. Remedy Verified does not provide medical services, and the content shared here should not be considered a substitute for professional medical guidance. Use of this website and its information is at your own risk.
Related Articles
This section will be populated with related content from Remedy Verified.
- The Ultimate Guide to Natural Diabetes Support
- Natural Antibiotics: 12 Evidence-Based Options + Safety Guide
- Tonsils and Adenoids: Symptoms, Treatment & When to Worry
- Can You Eat Before an MRI? 5 Cases That Require Fasting
- Hypoglycemia: Beyond the Blood Sugar Drop – Hidden Causes, Metabolic Consequences & Prevention Strategies