Tonsils and Adenoids: Symptoms, Treatment & When to Worry
What You Need to Know About Tonsils and Adenoids
Tonsils are two round tissue pads at the back of your throat that filter bacteria and viruses. Adenoids sit behind your nose and do the same job. Both are part of your immune system. Problems happen when they get infected repeatedly (tonsillitis) or grow so large they block breathing and cause sleep apnea.
See a doctor if: infections occur more than 5-7 times yearly, you notice breathing pauses during sleep, snoring disrupts sleep quality, throat pain lasts beyond 3 days with high fever, or swallowing becomes extremely difficult.
Most tonsil and adenoid problems resolve with rest, fluids, and pain management. Antibiotics treat bacterial infections like strep throat. Surgery (tonsillectomy and adenoidectomy) becomes necessary when infections recur frequently despite treatment or when enlarged tonsils and adenoids significantly block airways.
Track symptoms for 3 months: Document infection dates, severity, treatments used, and impact on daily life. This data guides your doctor in determining whether conservative care, medication, or surgery is the right path forward.
Where They Are and What They Actually Do
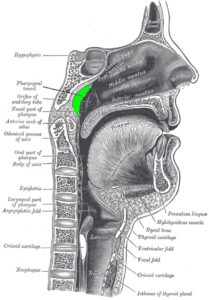
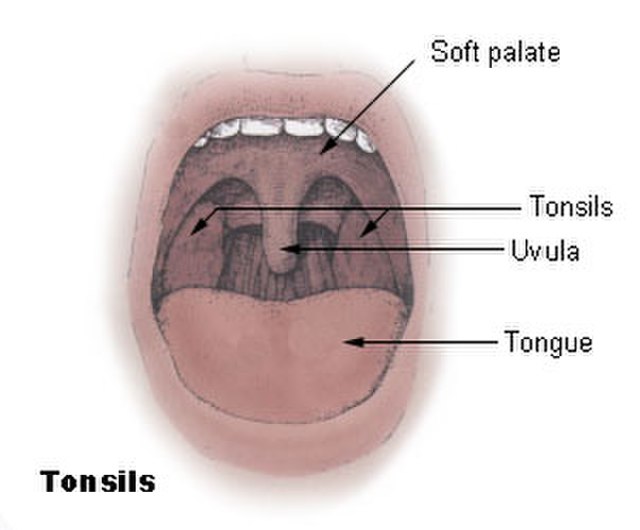
Your tonsils and adenoids form part of what’s called the tonsillar ring—essentially a circle of lymphoid tissue positioned right where your nasal cavity and mouth meet the throat. The two palatine tonsils are the ones you can see on either side of the back of your throat. The adenoid (sometimes called the pharyngeal tonsil) sits high in the throat behind your nose and soft palate—you can’t see it without special instruments. There’s also a third component, the lingual tonsil, which rests at the base of your tongue.
These tissues are part of your lymphatic system. They’re made of cells that sample incoming pathogens—basically, they’re security checkpoints. When bacteria or viruses enter through your nose or mouth, your tonsils and adenoids trap them and activate immune responses. Think of it as an early warning system that analyzes threats and alerts your broader immune system when necessary.
In children, tonsils and adenoids are proportionally larger than in adults. Why? They’re actively building immune memory during those critical developmental years.
That’s why tonsil and adenoid problems hit children harder and more frequently than adults.
Tonsils were once written off as useless evolutionary remnants. We know better now. Research shows they play a functional role in immune defense—particularly in early childhood. However, when chronic infection or extreme enlargement occurs, these tissues can shift from protector to problem. In patients with recurrent inflammation, studies show impaired cellular function within the tonsils. At that point, they’re no longer providing effective immune protection and may actually be harboring persistent infection.
Symptoms That Signal Tonsil or Adenoid Issues
Tonsil and adenoid problems fall into two main categories: infections and enlargement. Let’s break down what each looks like.
Acute tonsillitis strikes suddenly. You’ll know it—sore throat, painful swallowing, fever, and swollen lymph nodes. The tonsils may develop a white or gray coating. Viral infections like adenovirus, influenza, Epstein-Barr virus (mononucleosis), and coronavirus commonly trigger tonsillitis. Bacterial infections, particularly streptococcus (strep throat), require antibiotic treatment.

Chronic tonsillitis develops after repeated acute episodes or from persistent low-grade infection. Symptoms include ongoing

throat discomfort, bad breath, tonsil stones (small, foul-smelling white deposits lodged in tonsil crevices), and general malaise. Some people experience chronic tonsillitis without obvious flare-ups—just persistent inflammation that disrupts daily life.
Enlarged tonsils and adenoids create different problems centered on obstruction. When adenoids swell, nasal breathing becomes difficult, forcing mouth breathing day and night. The voice may sound nasal or muffled—like talking with your nose pinched. Children with enlarged adenoids often experience recurring ear infections because swollen tissue blocks the eustachian tube, trapping fluid in the middle ear and creating an environment where bacteria thrive. This can cause temporary hearing loss that affects speech development and school performance.
Sleep-disordered breathing represents one of the most concerning complications of tonsil and adenoid enlargement. Watch for loud snoring, gasping or choking sounds during sleep, pauses in breathing (apnea), restless sleep with frequent position changes, excessive sweating at night, and daytime fatigue or behavioral issues.
Peritonsillar abscess is a serious complication where infection creates a pocket of pus next to the tonsil, pushing it toward the opposite side. This requires immediate drainage. Less commonly, tonsil cancer can occur, particularly in adults. That’s another reason for prompt evaluation of persistent one-sided throat pain or a rapidly growing tonsil mass.
Decision Guide: Medical Care or Watchful Waiting
Call your doctor immediately if you see:
- Difficulty breathing or gasping for air
- Inability to swallow saliva (drooling)
- Severe one-sided throat pain with visible neck swelling
- Fever above 103°F (39.4°C) for more than 3 days
- Signs of dehydration (dark urine, extreme thirst, no tears)
- Muffled voice with rapid throat swelling
Schedule a routine appointment when:
- Throat infections happen 5-7+ times per year
- Your child snores loudly with breathing pauses during sleep
- Chronic mouth breathing affects speech or facial development
- Recurring ear infections require multiple antibiotic courses
- Persistent bad breath with visible white spots on tonsils (tonsil stones)
- School performance declines alongside sleep problems
Home observation is appropriate for:
- First or second mild sore throat of the season
- Viral symptoms (runny nose, cough, gradual onset)
- Mild discomfort manageable with over-the-counter pain relief
- Normal eating, drinking, and sleeping patterns maintained
The Paradise criteria provide objective surgical thresholds: 7+ documented infections in one year, 5+ per year for two years, or 3+ per year for three years. “Documented” means physician-confirmed cases—not every sore throat you remember having. Start tracking now: date, symptoms, treatment, days missed from school or work. Most families overestimate or underestimate frequency without written records.
Here’s a critical distinction many people miss: enlarged tonsils and adenoids without infection rarely need removal unless they’re obstructing breathing or causing sleep apnea. Conversely, normal-sized tonsils with chronic infection may require removal based on frequency alone. The decision centers on function and impact—not how they look.
From Antibiotics to Surgery: Standard Medical Treatments

Treatment pathways follow a stepwise approach based on cause, severity, and how much these issues are affecting quality of life. If you’ve got bacterial tonsillitis—particularly strep throat—you’ll need antibiotic therapy. This isn’t just about feeling better; it’s about preventing complications like rheumatic fever or kidney problems. Your clinician will likely run a rapid strep test or throat culture before prescribing anything. Why? Because viral infections don’t respond to antibiotics, and using them unnecessarily contributes to antibiotic resistance.
Standard antibiotic courses for strep throat last ten days, typically using penicillin or amoxicillin as first-line agents. Here’s the critical part: complete the entire course even if you feel better after three to four days. Stopping early lets surviving bacteria rebound and may promote resistant strains. Some clinicians used to try prophylactic (preventive) antibiotics for recurrent infections, but that approach has fallen out of favor due to resistance concerns and limited long-term benefit.
Tonsillectomy with or without adenoidectomy becomes a consideration when conservative approaches aren’t cutting it. The Paradise criteria provide evidence-based guidelines, but clinical judgment weighs additional factors: how severe each episode is (days missed from school or work, hospitalization, complications), impact on growth and development, sleep quality deterioration, and chronic symptoms despite treatment attempts.
“Surgery should be the last resort, but for the right candidates, it transforms quality of life.”
— Dr. Sarah Mitchell, Pediatric Otolaryngologist
Adenotonsillectomy takes approximately 45 minutes, performed through the mouth under general anesthesia. Most patients go home the same day, though children under age three, those with severe sleep apnea, significant obesity, or complex medical conditions often require overnight observation for safety monitoring.
Recovery runs seven to fourteen days for most patients—some need up to three weeks for complete healing. Pain management is critical because let’s be honest, the surgical site creates significant discomfort. Pain typically peaks around days four to six before gradually improving. Clinicians prescribe age-appropriate pain medication and emphasize hydration. Dehydration is actually the most common complication requiring return visits or readmission.
Bleeding represents the most serious surgical risk, occurring in approximately two to four percent of patients. Small amounts of blood-tinged saliva are normal, but bright red blood or clots require immediate medical evaluation. Dehydration risk increases because swallowing hurts, causing patients to avoid drinking. Cool liquids, popsicles, and soft foods help—and contrary to old advice about avoiding dairy, most patients tolerate ice cream and yogurt just fine if they prefer these options.
Partial tonsillectomy (tonsillotomy) has emerged as an alternative for select cases, particularly in young children with sleep-disordered breathing but minimal infection history. This procedure removes enough tissue to restore airway patency while leaving some tonsil tissue intact. Recovery is typically faster with less pain, though tonsil regrowth can occur in some cases, potentially requiring completion tonsillectomy later.
One thing often overlooked: insurance coverage requirements. Many insurers demand specific documentation—frequency logs, failed conservative treatments, sleep study results—before approving surgery. Work with your clinician’s office early to understand these requirements, because retroactive documentation rarely works for approval.
Post-surgery outcomes generally show significant improvement in quality of life for appropriately selected patients. Studies demonstrate reduced infection frequency, improved sleep quality, better behavior and attention in children with previous sleep apnea, and fewer missed school or work days. That said, surgery doesn’t eliminate all throat infections—patients can still develop pharyngitis from other causes. Setting realistic expectations about outcomes helps families make informed decisions aligned with their actual goals.
Evidence-Based Home Support and Prevention Strategies
Natural approaches serve two roles: easing discomfort during infections and building immune foundations that may reduce infection frequency. These complement medical treatment—they don’t replace antibiotics for strep throat or surgery for obstructive sleep apnea.
During active tonsillitis, do this now:
- Hydrate aggressively: Water, popsicles, ice chips, cold smoothies. Dehydration worsens pain and slows healing.
- Salt water gargles: 1/4 tsp salt in 8 oz warm water, 3-4 times daily. Reduces inflammation and clears debris from tonsil crypts. (Ages 6+)
- Honey for comfort: 1 tsp raw honey or mixed in herbal tea soothes throat irritation. (Ages 1+ only—never give honey to infants)
- Humidify your space: Cool-mist humidifier keeps airways moist, especially for mouth breathers. Clean weekly to prevent mold.
- Throat lozenges: Menthol or benzocaine types provide temporary numbing. Follow age guidelines on packaging.
Foundation prevention—what actually reduces infection frequency:
Sleep quality matters most. Children ages 6-12 need 9-12 hours nightly; teens need 8-10 hours; adults need 7-9 hours. Inadequate sleep impairs immune surveillance—your body’s ability to detect and stop pathogens before infection takes hold.
Nutrition over supplements. Whole foods provide vitamins A, C, D, zinc, and selenium that immune cells require. Ultra-processed diets high in added sugar correlate with increased inflammation. No supplement compensates for poor dietary foundations.
Hand hygiene prevents transmission. Wash hands 20 seconds with soap before meals, after bathroom use, and after coughing. Don’t share cups, utensils, toothbrushes, or food. Replace toothbrushes after strep throat treatment.
About supplements—use this framework if you’re considering them:
Vitamin D supplementation makes sense for documented deficiency (blood test showing levels below 20 ng/mL). Low vitamin D is associated with increased respiratory infections. But supplementing beyond sufficiency doesn’t add extra benefit.
Probiotics (Lactobacillus and Bifidobacterium strains) show modest evidence for reducing upper respiratory infections in children in some studies. A 2019 Cochrane review found probiotics might reduce infection frequency, though effect sizes varied and study quality was mixed. If you’re trying probiotics, choose third-party tested brands (USP, NSF) and coordinate with your doctor—especially if your child has immune conditions.
Zinc lozenges may shorten cold duration when started within 24 hours of symptoms. But preventive zinc supplementation lacks strong support and risks copper depletion long-term.
Structured supplement trial if you proceed: Add one supplement at a time. Trial for 8-12 weeks minimum. Track infection frequency in your log. Set stop criteria upfront (no reduction in infections, adverse effects, cost doesn’t justify benefit). Review results with your clinician before continuing.
What doesn’t have good evidence: Herbal throat sprays claiming to “boost immunity” without studied compounds and doses, colloidal silver (toxicity risk, no proven benefit), essential oils in young children (aspiration risk), and aggressive “detox” protocols that may delay appropriate medical care.
“Natural doesn’t automatically mean safe or effective. Start with sleep, nutrition, and hygiene foundations before adding supplements—and always coordinate with your medical team when infections are frequent.”
— Dr. James Chen, Integrative Pediatrician
When natural approaches aren’t enough: If infections continue despite optimizing sleep, nutrition, hygiene, and appropriate medical treatment, the conversation naturally shifts toward surgery. Don’t indefinitely pursue ineffective interventions—your symptom log will show what’s actually working.
Reducing Infection Risk and Supporting Throat Health
Daily prevention habits that work:
Hand hygiene (most effective): Wash hands with soap and water for 20 seconds before meals, after bathroom use, and after coughing or nose-blowing. Use alcohol-based sanitizer (60%+ alcohol) when soap isn’t available. Teach children to avoid touching their face, especially mouth and nose.
Don’t share these items: Drinking cups, water bottles, eating utensils, toothbrushes, lip balm, or food. During active infections, use separate towels and wash in hot water. Replace toothbrushes after completing strep throat antibiotics to prevent reinfection.
Environmental factors: Secondhand smoke irritates throat tissues and increases infection risk. If anyone smokes, do it outside and change clothes before close contact with children. Maintain indoor humidity between 30-50% and address mold or excessive dust. Clean regularly and consider HEPA air filters if allergies worsen throat symptoms.
When to keep children home: Stay home until fever-free for 24 hours without fever-reducing medication, and for at least 24 hours after starting antibiotics for strep throat. This reduces transmission while allowing recovery during the most contagious period. For viral tonsillitis without fever, decide based on energy level—exhausted, uncomfortable children need rest more than school attendance.
Post-surgery care (critical first 2 weeks):
- Follow all activity restrictions—no contact sports or strenuous exercise
- Drink fluids constantly even though swallowing hurts (prevents dehydration)
- Avoid crunchy, sharp, or acidic foods that irritate surgical sites
- Take pain medication on schedule as prescribed
- Watch for warning signs: bright red bleeding, inability to drink, fever above 102°F, severe uncontrolled pain, breathing difficulty
Peak pain occurs days 4-6 after tonsillectomy. Scabs fall off days 7-10, sometimes causing small amounts of blood-tinged saliva (normal). Complete healing takes 2-3 weeks. Call your surgeon immediately if you see bright red blood or large clots—not just pink-tinged saliva.
Building Your Decision Framework
Here’s the reality: tonsil and adenoid problems exist on a spectrum. Some are minor issues that resolve on their own. Others are serious conditions requiring surgical intervention. The path forward depends on objective criteria—infection frequency, symptom severity, impact on daily function, and how you’re responding to conservative treatments. Not assumptions or guesswork.
Not every sore throat needs antibiotics. Not every enlarged tonsil requires removal. The most successful outcomes happen when the intervention matches the specific problem: supportive care for viral infections and mild symptoms, antibiotics for confirmed bacterial infections, and surgery reserved for cases meeting evidence-based criteria where quality of life impact justifies the risks and recovery burden. Natural support approaches have their place within this framework—as adjuncts that optimize immune function and ease discomfort, not as replacements for necessary medical treatment.
Start with your symptom log. Track infection frequency, severity, treatment received, and impact on school, work, or sleep quality for the next three months. This data tells the real story and cuts through conflicting advice. If patterns suggest a problem, you’ll have the documentation needed for productive conversations with your clinician. If symptoms remain occasional and manageable, you’ll have confirmation that watchful waiting is working. Either way, you’re making informed choices based on evidence—not uncertainty. And that clarity? That’s worth more than any supplement or internet opinion could ever provide.
Myth vs. Fact: Clearing Up Tonsil Misconceptions
| Myth | Fact |
|---|---|
| “Tonsils are useless organs left over from evolution.” | Tonsils actively participate in immune defense, particularly during childhood when immune memory is developing. Research shows they sample pathogens and initiate immune responses. However, when chronically infected or severely enlarged, they can shift from asset to liability—removal in these specific cases improves outcomes without compromising overall immune function. |
| “Everyone with large tonsils needs surgery.” | Size alone doesn’t determine surgical necessity. Many children have naturally large tonsils that cause no problems and shrink with age. Surgery becomes appropriate when enlargement causes functional issues—breathing difficulty, sleep apnea, swallowing problems—or when frequent infections meet evidence-based criteria (Paradise criteria). Appearance matters less than impact. |
| “Removing tonsils will weaken my immune system permanently.” | Multiple studies show no clinically significant immune compromise after tonsillectomy. The body has numerous other lymphoid tissues and immune mechanisms that compensate. The American Academy of Otolaryngology states: “There are no studies to date that demonstrate a significant clinical impact of tonsillectomy on the immune system.” For appropriate candidates, benefits typically outweigh theoretical immune concerns. |
Frequently Asked Questions
Can adults have adenoid problems?
Yes, though it’s uncommon. Adenoids typically shrink significantly after puberty, but some adults retain adenoid tissue that can become infected or enlarged. Adult adenoid problems more often relate to chronic sinusitis or—rarely—tumors. Evaluation requires endoscopic examination since you can’t see adenoids during a routine throat check.
How do I know if it’s viral or bacterial tonsillitis?
You can’t reliably tell based on symptoms alone—that’s why your clinician will test. Bacterial tonsillitis (often strep) typically presents with sudden onset, high fever, white patches on tonsils, swollen lymph nodes, and absence of cough. Viral tonsillitis often includes cough, runny nose, and more gradual onset. Your doctor will perform a rapid strep test or throat culture to confirm bacterial infection before prescribing antibiotics.
Will removing tonsils stop all throat infections?
No, but it dramatically reduces them. Tonsillectomy typically cuts throat infection frequency significantly—most studies show 70-90% reduction in the first year post-surgery, with continued benefit over time. You can still develop pharyngitis from viruses or bacteria affecting other throat tissues. Set realistic expectations: surgery improves things dramatically but doesn’t eliminate all throat problems.
What foods should I eat after tonsillectomy?
Start with cool, soft foods: popsicles, ice cream, yogurt, smoothies, applesauce, mashed potatoes, scrambled eggs, and well-cooked pasta. Progress to your regular diet as tolerated, typically over seven to ten days. Avoid sharp, crunchy, acidic, or spicy foods that can irritate the surgical site. Despite old recommendations against dairy, most patients tolerate it fine—choose what provides comfort and encourages adequate calorie and fluid intake during recovery.
Can tonsil stones cause chronic bad breath?
Absolutely. Tonsil stones (tonsilloliths) are calcified debris lodged in tonsil crypts that produce foul-smelling sulfur compounds. They develop when food particles, bacteria, and dead cells accumulate in tonsil crevices. Most people can dislodge stones with gentle pressure using a cotton swab or water pick, though they tend to come back. Chronic, bothersome tonsil stones that don’t respond to home removal can be one indication for tonsillectomy—though this decision weighs symptom severity against surgical risks.
How long after tonsil surgery until full recovery?
Most patients return to normal activities within two weeks, though complete healing takes three weeks. Pain peaks around days four to six, then gradually improves. Scabs fall off around day seven to ten, sometimes causing minor bleeding. Avoid strenuous activity and contact sports for at least two weeks to prevent bleeding complications. Some patients—particularly adults—require closer to three weeks before feeling fully recovered. Follow your surgeon’s specific activity restrictions; they’re based on typical healing patterns and complication risk windows.
References
- American Academy of Otolaryngology–Head and Neck Surgery. Tonsils and Adenoids: Conditions and Treatments. ENT Health; 2019.
- Paradise JL, et al. Tonsillectomy and adenotonsillectomy for recurrent throat infection in moderately affected children. Pediatrics. 1984;73(6):855-866.
- Mitchell RB, et al. Clinical practice guideline: Tonsillectomy in children (Update). Otolaryngology–Head and Neck Surgery. 2019;160(1_suppl):S1-S42.
- Marcus CL, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):e714-e755.
- Hao GJ, et al. Probiotics for preventing acute upper respiratory tract infections. Cochrane Database of Systematic Reviews. 2015;(2):CD006895.
- National Institutes of Health. Vitamin D: Fact Sheet for Health Professionals. Office of Dietary Supplements; 2023.
- Centers for Disease Control and Prevention. Strep Throat: Information for Parents. CDC; 2023.
- Besedovsky L, et al. Sleep and immune function. Pflügers Archiv – European Journal of Physiology. 2012;463(1):121-137.
- Burton MJ, et al. Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis. Cochrane Database of Systematic Reviews. 2014;(11):CD001802.
- Georgalas CC, et al. The role of the surgery in the management of sleep-disordered breathing in children. Paediatric Respiratory Reviews. 2006;7(Suppl 1):S199-S201.
Disclaimer
⚠️ Disclaimer: The information provided in this article is for educational purposes only and is not intended as medical advice, diagnosis, or treatment. Tonsil and adenoid conditions vary significantly between individuals, and treatment decisions should be made in consultation with qualified healthcare professionals. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition, especially before making decisions about surgery or changing treatment approaches. Never disregard professional medical advice or delay seeking it because of something you have read in this article. If you think you or your child may have a medical emergency related to tonsil or adenoid problems—such as difficulty breathing, severe pain, or signs of dehydration—call your doctor or emergency services immediately. Remedy Verified does not provide medical services, and the content shared here should not be considered a substitute for professional medical guidance. Use of this website and its information is at your own risk.