Learn why systolic blood pressure matters most for heart health, what causes isolated systolic hypertension, and proven strategies to lower your top number safely.”>
Systolic Blood Pressure: What Your Top Number Really Means
When your doctor checks your blood pressure and says “120 over 80,” do you know what those numbers mean? Most people focus on whether their reading is “normal” or “high,” but understanding each number individually can help you better protect your heart health.
The top number (systolic pressure) often gets the spotlight, and for good reason. Research shows that systolic blood pressure is the strongest predictor of cardiovascular problems, especially as you get older. But what exactly makes this number so important?
Let’s explore everything you need to know about systolic blood pressure, from what it measures to why it matters more than you might think.
Understanding Systolic Blood Pressure
Systolic blood pressure measures the maximum pressure your blood exerts against your artery walls when your heart contracts and pumps blood throughout your body. Think of it as the peak force during each heartbeat.
When your heart squeezes, it pushes blood out into your arteries with considerable force. This surge of blood creates pressure against the artery walls. Your systolic reading captures this moment of maximum pressure.
The term “systolic” comes from the Greek word “systole,” which means contraction. So systolic pressure literally refers to the pressure during heart muscle contraction.
Systolic vs. Diastolic: The Key Differences
Your blood pressure reading contains two numbers for a reason. While systolic pressure measures the force during heartbeats, diastolic pressure (the bottom number) measures the force between beats when your heart relaxes and fills with blood.
Systolic Pressure (Top Number)
Diastolic Pressure (Bottom Number)
- Pressure when heart relaxes
- Measures resting force
- Usually lower than systolic
- Stays stable or decreases with age
- Important predictor in younger adults under 50
Interestingly, research in the journal Hypertension found that which number matters most depends partly on your age. In younger adults (under 50), both numbers provide important information. But in older adults, systolic pressure becomes the stronger predictor of heart problems.
Why Systolic Blood Pressure Matters Most
You might wonder why doctors pay so much attention to the systolic number. Several major research studies have shown that systolic pressure is a powerful predictor of cardiovascular events like heart attack and stroke.
The landmark SPRINT study (Systolic Blood Pressure Intervention Trial) demonstrated this clearly. Researchers found that lowering systolic pressure to less than 120 mmHg reduced heart attacks, heart failure, and strokes by 25% compared to targeting less than 140 mmHg.
This finding led to updated blood pressure guidelines in 2017. Before then, systolic pressure up to 140 was often considered acceptable. Now doctors know that lower is better for protecting your heart, brain, and kidneys.
The Link Between Systolic Pressure and Heart Disease
High systolic pressure damages your cardiovascular system through several mechanisms. But how exactly does elevated pressure harm your arteries and organs?
How High Systolic Pressure Causes Damage:
The higher your systolic pressure stays over time, the more damage accumulates. That’s why controlling systolic pressure early, before complications develop, is so important.
What Is Isolated Systolic Hypertension?
Sometimes only the top number is high while the bottom number stays normal. This condition is called isolated systolic hypertension, and it’s particularly common in older adults.
Isolated systolic hypertension means your systolic pressure is 130 mmHg or higher while your diastolic pressure remains below 80 mmHg. So a reading like 145/75 would indicate this condition.
For years, doctors debated whether treating isolated systolic hypertension was necessary. Some thought that if the diastolic number was normal, the condition wasn’t serious. We now know this assumption was wrong and potentially dangerous.
Why Isolated Systolic Hypertension Develops
Understanding why isolated systolic hypertension occurs helps explain why it’s so common in older adults. Several age-related changes contribute to this pattern.
As you age, your arteries naturally lose elasticity. Healthy, flexible arteries expand slightly when blood surges through them during heartbeats, then return to their normal size. But stiff arteries can’t expand as easily, so all that force stays concentrated as higher systolic pressure.
| Cause | How It Affects Systolic Pressure |
|---|---|
| Arterial Stiffening | Reduces artery flexibility, preventing normal expansion during heartbeats |
| Plaque Buildup | Narrows arteries and makes walls more rigid |
| Reduced Kidney Function | Impairs blood pressure regulation through fluid balance |
| Changes in Hormones | Affects renin-aldosterone system that controls blood pressure |
| Calcification | Calcium deposits in artery walls increase stiffness |
Meanwhile, diastolic pressure often stays stable or even decreases with age. This happens because stiff arteries also don’t recoil as well between heartbeats, so the resting pressure may actually drop slightly.
Health Risks of Isolated Systolic Hypertension
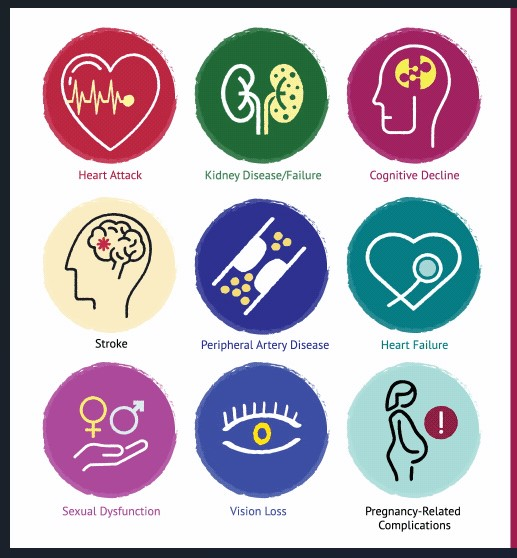
Don’t let the word “isolated” fool you into thinking this condition is less serious. Research shows that isolated systolic hypertension carries substantial risks for stroke, heart attack, heart failure, and kidney disease.
Major clinical trials like SHEP (Systolic Hypertension in the Elderly Program) and HYVET (Hypertension in the Very Elderly Trial) proved that treating isolated systolic hypertension provides significant benefits. Treatment reduced stroke risk by 30%, cardiovascular events by 23%, and overall death rates by 13%.
These findings changed medical practice. Now doctors know that high systolic pressure needs treatment regardless of whether diastolic pressure is also elevated.
Normal Systolic Blood Pressure Ranges
What should your systolic blood pressure be? The American Heart Association provides clear categories based on systolic readings.
| Blood Pressure Category | Systolic (Top Number) | And/Or | Diastolic (Bottom Number) |
|---|---|---|---|
| Normal | Less than 120 mmHg | and | Less than 80 mmHg |
| Elevated | 120-129 mmHg | and | Less than 80 mmHg |
| High BP Stage 1 | 130-139 mmHg | or | 80-89 mmHg |
| High BP Stage 2 | 140 mmHg or higher | or | 90 mmHg or higher |
| Hypertensive Crisis | Higher than 180 mmHg | and/or | Higher than 120 mmHg |
Notice that you can have high blood pressure based on either your systolic or diastolic number. If your systolic is 145 mmHg but your diastolic is only 70 mmHg, you still have Stage 2 hypertension.
How Systolic Pressure Changes With Age

While the target remains less than 120 mmHg regardless of age, average systolic pressure does increase as people get older. This trend is common but not inevitable or harmless.
Many people mistakenly believe that rising blood pressure is a normal, acceptable part of aging. This belief is dangerous because it discourages people from seeking treatment or making lifestyle changes.
The truth is that age-related blood pressure increases result largely from modifiable factors like weight gain, reduced physical activity, and dietary changes. People who maintain healthy habits throughout life often keep their systolic pressure in the normal range well into their senior years.
What Causes High Systolic Blood Pressure?
Understanding what drives your systolic pressure higher helps you identify areas where you can make improvements. Some causes you can’t change, but many respond well to lifestyle modifications or treatment.
For most people, high systolic pressure develops gradually over years or decades. This type is called primary or essential hypertension, and it doesn’t have one single identifiable cause.
Primary Causes and Risk Factors
Multiple factors typically work together to raise systolic blood pressure over time. Some of these you can control, while others you can’t.
Risk Factors You Can’t Change:
- Age: Arteries naturally stiffen as you get older, raising systolic pressure
- Family history: Genetics play a role in your blood pressure regulation
- Race: African Americans tend to develop high blood pressure earlier and more severely
Risk Factors You Can Modify:
- Excess weight: Extra body weight increases the workload on your heart
- Physical inactivity: Sedentary lifestyle leads to stiff arteries and poor circulation
- High sodium diet: Too much salt causes your body to retain fluid, raising pressure
- Low potassium intake: Potassium helps balance sodium’s effects
- Excessive alcohol: Drinking too much can damage your heart and raise pressure
- Chronic stress: Ongoing stress keeps pressure elevated through hormonal effects
- Poor sleep: Sleep deprivation disrupts blood pressure regulation
- Smoking: Tobacco damages blood vessels and causes temporary pressure spikes
The good news is that most of these modifiable factors respond well to lifestyle changes. Even small improvements can produce meaningful reductions in systolic pressure.
Secondary Causes of High Systolic Pressure
Sometimes high systolic blood pressure results from specific medical conditions. This is called secondary hypertension, and identifying the underlying cause can lead to more targeted treatment.
Conditions that can cause or worsen high systolic pressure include kidney disease, thyroid disorders, sleep apnea, certain medications (like decongestants and NSAIDs), and hormonal problems. If your blood pressure suddenly increases or doesn’t respond to treatment, your doctor may investigate these possibilities.
How to Lower Systolic Blood Pressure
Whether you have slightly elevated systolic pressure or full-blown hypertension, proven strategies can help bring your numbers down. The most effective approach usually combines lifestyle changes with medication when necessary.
Don’t expect overnight miracles. Lowering systolic pressure takes time and consistency. But the effort pays off with reduced risk of heart attack, stroke, and other serious complications.
Lifestyle Modifications That Work
These evidence-based lifestyle changes can significantly lower systolic blood pressure. Many people see improvements within weeks of making these adjustments.
For detailed guidance on implementing these strategies, including specific supplement recommendations and medication options, visit our comprehensive guide on effective high blood pressure management strategies.
Medications for Systolic Hypertension
When lifestyle changes aren’t enough to reach your systolic blood pressure goal, medications provide proven benefits. Several drug classes effectively lower systolic pressure, and your doctor can help determine which works best for you.
For isolated systolic hypertension, certain medications work particularly well. Thiazide diuretics and calcium channel blockers are often first-line choices because research shows they effectively reduce systolic pressure in older adults.
| Medication Class | How It Lowers Systolic Pressure | Best For |
|---|---|---|
| Thiazide Diuretics | Reduce fluid volume and relax blood vessels | Isolated systolic hypertension in older adults |
| Calcium Channel Blockers | Relax artery walls, improving flexibility | Isolated systolic hypertension, especially with stiff arteries |
| ACE Inhibitors | Block hormones that constrict blood vessels | People with diabetes, kidney disease, or heart failure |
| ARBs | Similar to ACE inhibitors with fewer side effects | Alternative to ACE inhibitors, especially if cough develops |
Research shows that combination therapy often works better than single medications for achieving systolic blood pressure goals. Your doctor might prescribe two medications together to maximize effectiveness while minimizing side effects.
Monitoring Your Systolic Blood Pressure
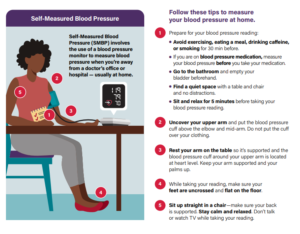
Regular monitoring helps you track your progress and catch problems early. Home blood pressure monitoring is particularly valuable because it provides more information than occasional office readings.
When monitoring at home, focus on your systolic number but don’t ignore the diastolic. Both numbers matter for your overall cardiovascular health.
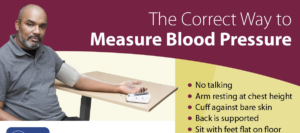
Best Practices for Accurate Readings
Getting accurate systolic pressure readings requires proper technique. Small mistakes can produce readings that are 10-20 mmHg too high or too low.
Steps for Accurate Measurement:
- Rest quietly for 5 minutes before measuring
- Sit with your back supported and feet flat on the floor
- Place the cuff on bare skin at heart level
- Don’t talk or move during the reading
- Take two readings one minute apart and average them
- Measure at the same time each day for consistency
- Avoid caffeine, exercise, or smoking for 30 minutes before
- Empty your bladder before measuring
Keep a log of your readings with the date and time. Look for patterns over days and weeks rather than worrying about individual readings. Blood pressure naturally fluctuates throughout the day, so one high reading doesn’t necessarily indicate a problem.
When to Check Your Systolic Pressure
How often should you monitor your systolic blood pressure? The answer depends on your current readings and risk factors.
If you have normal blood pressure, check it at least once every two years. But if you’re in the elevated or Stage 1 hypertension range, monitor more frequently – ideally weekly or even daily while making lifestyle changes.
People with Stage 2 hypertension or those taking blood pressure medications should check at home several times per week. This frequent monitoring helps you and your doctor know whether your treatment plan is working effectively.
When High Systolic Pressure Becomes Dangerous
While chronically elevated systolic pressure damages your health gradually over years, extremely high readings can create immediate medical emergencies. Knowing the warning signs helps you respond appropriately.
A hypertensive crisis occurs when systolic pressure rises above 180 mmHg. At these levels, you face immediate risk of organ damage. But the severity depends on whether you’re experiencing symptoms.
Hypertensive Urgency
Systolic > 180 mmHg
No symptoms present
Contact your doctor same day
May need medication adjustment
Hypertensive Emergency
Systolic > 180 mmHg
Plus chest pain, shortness of breath, vision changes, or severe headache
Call 911 immediately
Requires emergency treatment
Never try to rapidly lower extremely high systolic pressure on your own. Paradoxically, lowering pressure too quickly can reduce blood flow to your brain and other organs, potentially causing a stroke. Emergency medical teams know how to lower pressure safely and gradually.
Signs Your Systolic Pressure Needs Immediate Attention
Most people with high systolic pressure feel fine, which is why it’s called the silent killer. However, certain symptoms suggest your pressure has reached dangerous levels.
Seek emergency care if you have a systolic reading above 180 mmHg along with chest pain, severe headache, vision changes, difficulty breathing, confusion, or any stroke symptoms (facial drooping, arm weakness, speech difficulty).
Also contact your doctor promptly if your normally well-controlled systolic pressure suddenly increases by 20-30 mmHg or more. This could indicate that your medications need adjustment or that a new health problem has developed.
Special Considerations for Different Age Groups
While the goal of less than 120 mmHg systolic pressure applies broadly, certain age groups face unique challenges and considerations.
Systolic Pressure in Younger Adults
High systolic blood pressure isn’t just an older person’s problem. Increasingly, younger adults are developing elevated systolic pressure due to obesity, sedentary lifestyles, and poor dietary habits.
For people under 50, both systolic and diastolic pressure matter. Research shows that in younger adults, an elevated diastolic number combined with normal systolic pressure can also predict cardiovascular problems.
The good news is that younger adults often respond very well to lifestyle changes. Because arterial stiffening hasn’t yet occurred, diet, exercise, and weight management can frequently normalize systolic pressure without medication.
Systolic Hypertension in Older Adults
Treating high systolic pressure in older adults requires balancing benefits with potential risks. While lowering systolic pressure definitely reduces stroke and heart attack risk at any age, treatment needs individualization.
Older adults are more prone to orthostatic hypotension (dizziness when standing up) and may take multiple medications that interact. Some frail elderly people may need slightly higher systolic targets to avoid falls and other complications from overly aggressive treatment.
However, most healthy older adults benefit from achieving the same systolic blood pressure goals as younger people. Age alone shouldn’t prevent appropriate treatment.
The Future of Systolic Blood Pressure Management
Research continues to refine our understanding of optimal systolic blood pressure targets and treatment approaches. Several exciting developments may improve how we manage systolic hypertension in the future.
Personalized medicine approaches using genetic testing might help identify who will benefit most from aggressive systolic pressure lowering. This could allow doctors to tailor treatment intensity based on individual risk profiles.
New medications targeting arterial stiffness are in development. Since stiff arteries are the main driver of isolated systolic hypertension in older adults, treatments that restore arterial flexibility could be game-changing.
Digital health technologies like continuous blood pressure monitoring may also improve management. Instead of relying on sporadic readings, people could track systolic pressure trends throughout the day and night, allowing for more precise treatment adjustments.
Taking Control of Your Systolic Blood Pressure
Your systolic blood pressure is one of the most important numbers for your cardiovascular health. As the top number in your blood pressure reading, it measures the peak force against your artery walls with each heartbeat.
Research clearly shows that keeping systolic pressure below 120 mmHg protects your heart, brain, and kidneys at any age. This is especially important as you get older, when isolated systolic hypertension becomes increasingly common.
The good news is that you have significant control over your systolic pressure through lifestyle choices. Diet, exercise, weight management, stress reduction, and adequate sleep all contribute to healthier readings. When lifestyle changes aren’t enough, effective medications can help you reach your goals.
Don’t wait for symptoms to develop before addressing high systolic pressure. By the time you feel problems, significant damage may have already occurred. Instead, be proactive about checking your blood pressure and taking steps to keep it in the healthy range.
Your systolic pressure today predicts your cardiovascular health tomorrow. Make it a priority, and your future self will thank you.
References
- American Heart Association. Understanding Blood Pressure Readings. Retrieved September 29, 2025.
- Harvard Health Publishing. (2024). Reading the new blood pressure guidelines. Retrieved September 29, 2025.
- American Heart Association. (2023). Blood pressure: What do the numbers mean and why do they matter? Retrieved September 29, 2025.
- American Heart Association. (2021). Which blood pressure number matters most? The answer might depend on your age. Retrieved September 29, 2025.
- Cleveland Clinic. (2025). Isolated Systolic Hypertension: Causes, Symptoms & Treatment. Retrieved September 29, 2025.
- Mayo Clinic. (2024). Isolated systolic hypertension: A health concern? Retrieved September 29, 2025.
- Mayo Clinic. (2024). High blood pressure (hypertension) – Diagnosis & treatment. Retrieved September 29, 2025.
- National Heart, Lung, and Blood Institute. High Blood Pressure – What Is High Blood Pressure? Retrieved September 29, 2025.
- StatPearls. (2023). Systolic Hypertension. Retrieved September 29, 2025.
- WebMD. (2025). High Systolic Blood Pressure & Isolated Systolic Hypertension. Retrieved September 29, 2025.
Medical Disclaimer
This article is for informational purposes only and does not constitute medical advice. Systolic blood pressure management requires professional medical supervision and evaluation. Always consult with a qualified healthcare provider for blood pressure diagnosis, treatment recommendations, and medication management. Individual blood pressure targets may vary based on age, health conditions, and cardiovascular risk factors. This information should not replace professional medical guidance or regular blood pressure monitoring by healthcare professionals.